Abstract
Polymeric films are drug delivery systems that maintain contact with the delivery tissue and sustain a controlled release of therapeutic molecules. These systems allow a longer time of drug contact with the target site in the case of topical treatments and allow the controlled administration of drugs. They can be manufactured by various methods such as solvent casting, hot melt extrusion, electrospinning, and 3D bioprinting. Furthermore, they can employ various polymers, for example PVP, PVA, cellulose derivatives, chitosan, gelling gum, pectin, and alginate. Its versatility is also applicable to different routes of administration, as it can be administered to the skin, oral mucosa, vaginal canal, and eyeballs. All these factors allow numerous combinations to obtain a better treatment. This review focuses on exploring some possible ways to develop them and some particularities and advantages/disadvantages in each case. It also aims to show the versatility of these systems and the advantages and disadvantages in each case, as they bring the opportunity to develop different medicines to facilitate therapies for the most diverse purposes .



Similar content being viewed by others
References
Singh I, Morris A. Performance of transdermal therapeutic systems: effects of biological factors. Int J Pharm Investig. 2011;1(1):4–9. https://doi.org/10.4103/2230-973X.76721.
Hermans K, Van Den Plas D, Kerimova S, Carleer R, Adriaensens P, Weyenberg W, et al. Development and characterization of mucoadhesive chitosan films for ophthalmic delivery of cyclosporine A. Int J Pharm [Internet]. 2014;472(1–2):10–9. https://doi.org/10.1016/j.ijpharm.2014.06.017.
Ham AS, Rohan LC, Boczar A, Yang L, Buckheit KW, Buckheit RW. Vaginal film drug delivery of the pyrimidinedione IQP-0528 for the prevention of HIV infection. Pharm Res. 2012;29(7):1897–907. https://doi.org/10.1007/s11095-012-0715-7.
RohaniShirvan A, Bashari A, Hemmatinejad N. New insight into the fabrication of smart mucoadhesive buccal patches as a novel controlled-drug delivery system. Eur Polym J [Internet]. 2019;119(July):541–50. https://doi.org/10.1016/j.eurpolymj.2019.07.010.
Hoffmann EM, Breitenbach A, Breitkreutz J. Advances in orodispersible films for drug delivery. Expert Opin Drug Deliv. 2011;8(3):299–316. https://doi.org/10.1517/17425247.2011.553217.
Al Hanbali OA, Khan HMS, Sarfraz M, Arafat M, Ijaz S, Hameed A. Transdermal patches: design and current approaches to painless drug delivery. Acta Pharm. 2019;69(2):197–215. https://doi.org/10.2478/acph-2019-0016.
Kianfar F, Chowdhry BZ, Antonijevic MD, Boateng JS. Novel films for drug delivery via the buccal mucosa using model soluble and insoluble drugs. Drug Dev Ind Pharm. 2012;38(10):1207–20. https://doi.org/10.3109/03639045.2011.644294.
Sizílio RH, Galvão JG, Trindade GGG, Pina LTS, Andrade LN, Gonsalves JKMC, et al. Chitosan/pvp-based mucoadhesive membranes as a promising delivery system of betamethasone-17-valerate for aphthous stomatitis. Carbohydr Polym. 2018;190(15):339–45. https://doi.org/10.1016/j.carbpol.2018.02.079.
Boddupalli BM, Mohammed ZNK, Nath AR, Banji D. Mucoadhesive drug delivery system: an overview. J Adv Pharm Technol Res. 2010;1(4):381–7. https://doi.org/10.4103/0110-5558.76436.
Pastore MN, Kalia YN, Horstmann M, Roberts MS. Transdermal patches: history, development and pharmacology. Br J Pharmacol. 2015;172(9):2179–209 https://pubmed.ncbi.nlm.nih.gov/25560046/.
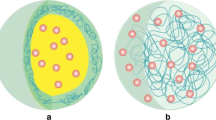
Yang WW, Pierstorff E. Reservoir-based polymer drug delivery systems. J Lab Autom. 2012;17(1):50–8. https://doi.org/10.1177/2211068211428189.
Sarwar MS, Huang Q, Ghaffar A, Abid MA, Zafar MS, Khurshid Z, et al. A smart drug delivery system based on biodegradable chitosan/poly(Allylamine hydrochloride) blend films. Pharmaceutics. 2020;12(2):131. https://doi.org/10.3390/pharmaceutics12020131.
Jacob J, Haponiuk JT, Thomas S, Gopi S. Biopolymer based nanomaterials in drug delivery systems: a review. Mater Today Chem. 2018;9:43–55. https://doi.org/10.1016/J.MTCHEM.2018.05.002.
Mogoşanu GD, Grumezescu AM. Natural and synthetic polymers for wounds and burns dressing. Int J Pharm. 2014;463(2):127–36. https://doi.org/10.1016/j.ijpharm.2013.12.015.
Sizílio RH, Galvão JG, Trindade GGG, Pina LTS, Andrade LN, Gonsalves JKMC, et al. Chitosan/pvp-based mucoadhesive membranes as a promising delivery system of betamethasone-17-valerate for aphthous stomatitis. Carbohydr Polym. 2017;2018(190):339–45. https://doi.org/10.1016/j.carbpol.2018.02.079.
Ravikumar R, Ganesh M, Senthil V, Ramesh YV, Jakki SL, Choi EY. Tetrahydro curcumin loaded PCL-PEG electrospun transdermal nanofiber patch: preparation, characterization, and in vitro diffusion evaluations. J Drug Deliv Sci Technol. 2017;2018(44):342–8. https://doi.org/10.1016/j.jsps.2017.02.004.
Fernandes JG, Correia DM, Botelho G, Padrão J, Dourado F, Ribeiro C, et al. PHB-PEO electrospun fiber membranes containing chlorhexidine for drug delivery applications. Polym Test. 2014;34:64–71. https://doi.org/10.1016/j.polymertesting.2013.12.007.
Reddy AB, Manjula B, Jayaramudu T, Sadiku ER, Anand Babu P, Periyar SS. 5-Fluorouracil loaded chitosan–PVA/Na+MMT nanocomposite films for drug release and antimicrobial activity. Nano-Micro Lett. 2016;8(3):260–9. https://doi.org/10.1007/s40820-016-0086-4.
Shit SC, Shah PM. Edible polymers: challenges and opportunities. J Polym. 2014;2014:1–13. https://doi.org/10.1155/2014/427259.
Kolakovic R, Peltonen L, Laukkanen A, Hirvonen J, Laaksonen T. Nanofibrillar cellulose films for controlled drug delivery. Eur J Pharm Biopharm [Internet]. 2012;82(2):308–15. https://doi.org/10.1016/j.ejpb.2012.06.011.
Riccio BVF, Klosowski AB, Prestes E, de Sousa TB, de Assunção Morais LC, Lemes BM, et al. Chitosan/nanocellulosebased bionanocomposite films for controlled betamethasone and silver sulfadiazine delivery. J Appl Polym Sci. 2020;2021:1–13. https://doi.org/10.1002/app.50468.
Adrover A, Di Muzio L, Trilli J, Brandelli C, Paolicelli P, Petralito S, et al. Enhanced loading efficiency and mucoadhesion properties of gellan gum thin films by complexation with hydroxypropyl-β-cyclodextrin. Pharmaceutics. 2020;12(9):1–21. https://doi.org/10.3390/pharmaceutics12090819.
Liakos I, Rizzello L, Bayer IS, Pompa PP, Cingolani R, Athanassiou A. Controlled antiseptic release by alginate polymer films and beads. Carbohydr Polym [Internet]. 2013;92(1):176–83. https://doi.org/10.1016/j.carbpol.2012.09.034.
Taylor P, Božani DK, Djokovi V, Krsmanovi R, Radhakrishnan T. J Biomater Sci. Inhibition of microbial growth by silver – starch nanocomposite thin films. 2013;2012:2343–55. https://doi.org/10.1163/092050610X539532.
Kulkarni V, Butte K, Rathod S. Natural polymers – a comprehensive review. Int J Res Pharm Biomed Sci. 2012;3(4):1597–613. https://doi.org/10.1201/9781003130765.
Irfan M, Rabel S, Bukhtar Q, Qadir MI, Jabeen F, Khan A. Orally disintegrating films: a modern expansion in drug delivery system. Saudi Pharm J [Internet]. 2016;24(5):537–46. https://doi.org/10.1016/j.jsps.2015.02.024.
WHO Expert Committee on Specifications for Pharmaceutical Preparations. Annex 5 Development of paediatric medicines: points to consider in formulation. Tech Reports. 2012;46(970):197–225 http://www.who.int/medicines/areas/quality_safety/quality_assurance/Annex5TRS-970.pdf?ua=1.
Takahashi K, Komai M, Kinoshita N, Nakamura E, Hou XL, Takatani-Nakase T, et al. Application of hydrotropy to transdermal formulations: hydrotropic solubilization of polyol fatty acid monoesters in water and enhancement effect on skin permeation of 5-FU. J Pharm Pharmacol. 2011;63(8):1008–14.
Parivesh S, Sumeet D, Abhishek D. Design, evaluation, parameters and marketed products of transdermal patches: a review. J Pharm Res. 2010;3(2):235–40. https://doi.org/10.1590/S1984-82502015000200015.
Bacakova L, Pajorova J, Bacakova M, Skogberg A, Kallio P, Kolarova K, et al. Versatile application of nanocellulose: from industry to skin tissue engineering and wound healing. Nanomaterials. MDPI AG. 2019;29(9):164. https://doi.org/10.3390/nano9020164.
Phanthong P, Reubroycharoen P, Hao X, Xu G. Nanocellulose : extraction and application. Carbon Resour Convers [Internet]. 2018;1(1):32–43. https://doi.org/10.1016/j.crcon.2018.05.004.
Falamarzpour P, Behzad T, Zamani A. Preparation of nanocellulose reinforced chitosan films, cross-linked by adipic acid. Int J Mol Sci. 2017;18(2):1–12. https://doi.org/10.3390/ijms18020396.
Tayeb AH, Amini E, Ghasemi S, Tajvidi M. Cellulose nanomaterials-binding properties and applications: a review. Molecules. 2018;23(10):1–24. https://doi.org/10.3390/molecules23102684.
Abdul Khalil HPS, Saurabh CK, Adnan AS, Nurul Fazita MR, Syakir MI, Davoudpour Y, et al. A review on chitosancellulose blends and nanocellulose reinforced chitosan biocomposites: properties and their applications. Carbohydrate Polymers. Elsevier Ltd. 2016;150:216–26. https://doi.org/10.1016/j.carbpol.2016.05.028.
Tajeddin B. Cellulose-based polymers for packaging applications. Lignocellul Polym Compos Process Charact Prop. 2014;2014(9781118773):477–98. https://doi.org/10.1016/B978-0-323-88528-7.00013-7.
Mariano M, El Kissi N, Dufresne A. Cellulose nanomaterials: size and surface influence on the thermal and rheological behavior. Polimeros. 2018;28(2):93–102. https://doi.org/10.1590/0104-1428.2413.
Kiss É. Characterization of polymer blends: miscibility, morphology and interfaces. Ellipsometry. 2015;9783527331:299–326.
Intakhab Alam M, Alam N, Singh V, Sarfaraz Alam M, Sajid Ali M, Anwer T, et al. Type, preparation and evaluation of transdermal patch: a review. 2013;(May 2020). https://doi.org/10.1590/S1984-82502015000200015.
Jhawat VC, Saini V, Kamboj S, Maggon N. Transdermal drug delivery systems: approaches and advancements in drug absorption through the skin. 2013;20(1):47–56.
Brown MB, Martin GP, Jones SA, Akomeah FK. Dermal and transdermal drug delivery systems: current and future prospects. Drug Deliv J Deliv Target Ther Agents. 2006;13(3):175–87. https://doi.org/10.1080/10717540500455975.
Ruela ALM, Perissinato AG, de Lino ME, S, Mudrik PS, Pereira GR. Evaluation of skin absorption of drugs from topical and transdermal formulations. Brazilian. J Pharm Sci. 2016;52(3):527–44. https://doi.org/10.1590/S1984-82502016000300018.
Villasante J, Martin-Lujano A, Almajano MP. Characterization and application of gelatin films with pecan walnut and shell extract (Carya illinoiensis). Polymers (Basel). 2020;12(6). https://doi.org/10.3390/polym12061424.
Kuo MS, Mort AJ, Dell A. Identification and location of l-glycerate, an unusual acyl substituent in gellan gum. Carbohydr Res. 1986;156(C):173–87. https://doi.org/10.1590/fst.05518.
Milas M, Shi X, Rinaudo M. On the physicochemical properties of gellan gum. Biopolymers. 1990;30(3–4):451–64. https://doi.org/10.1002/bip.360300322.
Kang KS, Veeder GT, Mirrasoul PJ. Agar-like polysaccharide produced by a Pseudomonas species: production and basic properties. Appl Environ Microbiol. 1982;43(5):1086–91. https://doi.org/10.1128/aem.43.5.1086-1091.1982.
Osmałek T, Froelich A, Tasarek S. Application of gellan gum in pharmacy and medicine. Int J Pharm. 2014;466(1–2):328–40. https://doi.org/10.1016/j.ijpharm.2014.03.038.
Zia KM, Tabasum S, Khan MF, Akram N, Akhter N, Noreen A, et al. Recent trends on gellan gum blends with natural and synthetic polymers: a review. Int J Biol Macromol. 2018;109:1068–87. https://doi.org/10.1016/j.ijbiomac.2017.11.099.
Palumbo FS, Federico S, Pitarresi G, Fiorica C, Giammona G. Gellan gum-based delivery systems of therapeutic agents and cells. Carbohydr Polym. 2020;229(June):115430. https://doi.org/10.1016/j.carbpol.2019.115430.
Milivojevic M, Pajic-lijakovic I, Bugarski B, Nayak AK, Hasnain S. Chapter 6 - Gellan gum in drug delivery applications. Natural polysaccharides in drug delivery and biomedical applications. Elsevier Inc. 2019:145–86. https://doi.org/10.1016/B978-0-12-817055-7.00006-6.
Prezotti FG, Siedle I, Boni FI, Müller I, Stringhetti B, Cury F. delivery ce pt ip t. Pharm Dev Technol. 2019. https://doi.org/10.1080/10837450.2019.1682608.
Das M, Giri TK. Hydrogels based on gellan gum in cell delivery and drug delivery. J Drug Deliv Sci Technol. 2020;56:101586. https://doi.org/10.1016/j.jddst.2020.101586.
Vuornos K, Ojansivu M, Koivisto JT, Häkkänen H, Belay B, Montonen T, et al. Bioactive glass ions induce efficient osteogenic differentiation of human adipose stem cells encapsulated in gellan gum and collagen type I hydrogels. Mater Sci Eng C. 2019;99(February):905–18. https://doi.org/10.1016/j.msec.2019.02.035.
Musazzi UM, Cencetti C, Franze S, Zoratto N, Di MC, Procacci P, et al. Gellan nanohydrogels: novel nanodelivery systems for cutaneous administration of piroxicam. 2018. https://doi.org/10.1021/acs.molpharmaceut.7b00926.
Meneguin AB, Beyssac E, Garrait G, Hsein H, Cury BSF. Retrograded starch/pectin coated gellan gum-microparticles for oral administration of insulin: a technological platform for protection against enzymatic degradation and improvement of intestinal permeability. Eur J Pharm Biopharm. 2018;123:84–94. https://doi.org/10.1016/j.ejpb.2017.11.012.
Karemore MN, Bali NR. Gellan gum based gastroretentive tablets for bioavailability enhancement of cilnidipine in human volunteers. Int J Biol Macromol. 2021;174:424–39. https://doi.org/10.1016/j.ijbiomac.2021.01.199.
Adetunji LR, Adekunle A, Orsat V, Raghavan V. Advances in the pectin production process using novel extraction techniques: a review. Food Hydrocoll. 2017;62:239–50. https://doi.org/10.1016/j.foodhyd.2016.08.015.
Andersen NM, Cognet T, Santacoloma PA, Larsen J, Armagan I, Larsen FH, et al. Dynamic modelling of pectin extraction describing yield and functional characteristics. J Food Eng. 2017;192:61–71. https://doi.org/10.1016/j.jfoodeng.2016.08.006.
Cao L, Lu W, Mata A, Nishinari K, Fang Y. Egg-box model-based gelation of alginate and pectin: a review. Carbohydr Polym. 2020;242(May):116389. https://doi.org/10.1016/j.carbpol.2020.116389.
Wusigale Liang L, Luo Y. Casein and pectin: Structures, interactions, and applications. Trends Food Sci Technol. 2020;97(September2019):391–403. https://doi.org/10.1016/j.tifs.2020.01.027.
Dranca F, Vargas M, Oroian M. Physicochemical properties of pectin from Malus domestica ‘Fălticeni’ apple pomace as affected by non-conventional extraction techniques. Food Hydrocoll. 2019;2020(100):105383. https://doi.org/10.1590/S1516-89132005000200013.
Meneguin AB, Ferreira Cury BS, dos Santos AM, Franco DF, Barud HS, da Silva Filho EC. Resistant starch/pectin freestanding films reinforced with nanocellulose intended for colonic methotrexate release. Carbohydrate Polymers. 2017;157:1013–23. https://doi.org/10.1016/j.carbpol.2016.10.062.
Wang S-Y, Meng Y-J, Li J, Liu J-P, Liu Z-Q, Li D-Q. A novel and simple oral colon-specific drug delivery system based on the pectin/modified nano-carbon sphere nanocomposite gel films. Int J Biol Macromol. 2020;157:170–6. https://doi.org/10.1016/j.ijbiomac.2020.04.197.
Cao L, Lu W, Mata A, Nishinari K, Fang Y, Dranca F, et al. Fully physically crosslinked pectin-based hydrogel with high stretchability and toughness for biomedical application. Food Hydrocoll. 2020;149(12):1–31. https://doi.org/10.1016/j.ijbiomac.2020.01.297.
Nesic A, Meseldzija S, Cabrera-Barjas G, Onjia A. Novel biocomposite films based on high methoxyl pectin reinforced with zeolite Y for food packaging applications. Foods. 2022;11(3):1–11. https://doi.org/10.3390/foods11030360.
Loureiro dos Santos LA. Natural polymeric biomaterials: processing and properties. Ref Modul Mater Sci Mater Eng. 2016;2017:1–6. https://doi.org/10.1016/B978-0-12-803581-8.02253-0.
Lee KY, Mooney DJ. Alginate: properties and biomedical applications. Prog Polym Sci. 2012;37(1):106–26. https://doi.org/10.1016/j.progpolymsci.2011.06.003.
Bennacef C, Desobry-Banon S, Probst L, Desobry S. Advances on alginate use for spherification to encapsulate biomolecules. Food Hydrocoll. 2021;118(November 2020). https://doi.org/10.1016/j.foodhyd.2021.106782.
Yang JS, Xie YJ, He W. Research progress on chemical modification of alginate: a review. Carbohydr Polym. 2011;84(1):33–9. https://doi.org/10.1016/j.carbpol.2010.11.048.
Davidovich-Pinhas M, Bianco-Peled H. Alginate-PEGAc: a new mucoadhesive polymer. Acta Biomater. 2011;7(2):625–33. https://doi.org/10.1016/j.actbio.2010.09.021.
Pacheco MS, Barbieri D, da Silva CF, de Moraes MA. A review on orally disintegrating films (ODFs) made from natural polymers such as pullulan, maltodextrin, starch, and others. Int J Biol Macromol. 2021;178:504–13. https://doi.org/10.1016/j.ijbiomac.2021.02.180.
Kowalska-Krochmal B, Dudek-Wicher R. The minimum inhibitory concentration of antibiotics : methods, interpretation, clinical relevance. 2021. https://doi.org/10.3390/pathogens10020165.
Ahmad A, Mubarak NM, Jannat FT, Ashfaq T, Santulli C, Rizwan M, et al. A critical review on the synthesis of natural sodium alginate based composite materials: an innovative biological polymer for biomedical delivery applications. Processes. 2021;9(1):1–27. https://doi.org/10.3390/pr9010137.
T. Pelegrino M, B. Seabra A. Chitosan-based nanomaterials for skin regeneration. AIMS. Med Sci. 2017;4(3):352–81. https://doi.org/10.3934/medsci.2017.3.352.
Elieh-Ali-Komi D, Hamblin MR. Chitin and chitosan: production and application of versatile biomedical nanomaterials. Int J Adv Res. 2016;4(3):411–27.
Shamloo A, Aghababaie Z, Afjoul H, Jami M, Bidgoli MR, Vossoughi M, et al. Fabrication and evaluation of chitosan/gelatin/PVA hydrogel incorporating honey for wound healing applications: an in vitro, in vivo study. Int J Pharm. 2020;2020(592):6–13. https://doi.org/10.1016/j.ijpharm.2020.120068.
De SC, De MNH, Palmira M, Gremi D, Chorilli M. Design of mucoadhesive nanostructured polyelectrolyte complexes based on chitosan and hypromellose phthalate for metronidazole delivery intended to the treatment of Helicobacter pylori infections. 2020;12(12):1211. https://doi.org/10.3390/pharmaceutics12121211.
Yassue-Cordeiro PH, Zandonai CH, Genesi BP, Lopes PS, Sanchez-Lopez E, Garcia ML, et al. Development of chitosan/silver sulfadiazine/zeolite composite films for wound dressing. Pharmaceutics. 2019;11(10):1–22. https://doi.org/10.3390/pharmaceutics11100535.
Escárcega-Galaz AA, Sánchez-Machado DI, López-Cervantes J, Sanches-Silva A, Madera-Santana TJ, Paseiro-Losada P. Mechanical, structural and physical aspects of chitosan-based films as antimicrobial dressings. Int J Biol Macromol. 2017;2018(116):472–81. https://doi.org/10.1016/j.ijbiomac.2018.04.149.
Lizardi-Mendoza J, Argüelles Monal WM, Goycoolea Valencia FM. Chemical characteristics and functional properties of chitosan. Chitosan in the preservation of agricultural commodities. Elsevier Inc. 2016:3–31. https://doi.org/10.1016/B978-0-12-802735-6/00001-X.
Croisier F, Jérôme C. Chitosan-based biomaterials for tissue engineering. Eur Polym J. 2013;49(4):780–92. https://doi.org/10.1016/j.eurpolymj.2012.12.009.
Badi N. Non-linear PEG-based thermoresponsive polymer systems. Prog Polym Sci. 2017;66:54–79. https://doi.org/10.1016/j.progpolymsci.2016.12.006.
Liu SL, Shao L, Chua ML, Lau CH, Wang H, Quan S. Recent progress in the design of advanced PEO-containing membranes for CO2 removal. Prog Polym Sci. 2013;38(7):1089–120. https://doi.org/10.1016/j.progpolymsci.2013.02.002.
Kargari A, Rezaeinia S. State-of-the-art modification of polymeric membranes by PEO and PEG for carbon dioxide separation: a review of the current status and future perspectives. J Ind Eng Chem. 2020;84:1–22. https://doi.org/10.1016/j.jiec.2019.12.020.
Spitzer M, Sabadini E, Loh W. Poly(ethylene glycol) or Poly(ethylene oxide): Magnitude of end-group contribution to the partitioning of ethylene oxide oligomers and polymers between water and organic phases. 2002;13(1):7–9. https://doi.org/10.1590/S0103-50532002000100002.
Li J, Kao WJ. Synthesis of polyethylene glycol (PEG) derivatives and PEGylated - peptide biopolymer conjugates. Biomacromol. 2003;4(4):1055–67. https://doi.org/10.1021/bm034069l.
Kolate A, Baradia D, Patil S, Vhora I, Kore G, Misra A. PEG - a versatile conjugating ligand for drugs and drug delivery systems. J Control Release. 2014;192:67–81. https://doi.org/10.1016/j.jconrel.2014.06.046.
Zhang Q. Investigating polymer conformation in poly (ethylene oxide) (PEO) based systems for pharmaceutical applications a Raman spectroscopic study of the hydration process. 2011:1–35.
Abu Lila AS, Shimizu T, Ishida T. PEGylation and anti-PEG antibodies. Engineering of biomaterials for drug delivery systems: beyond polyethylene glycol. Elsevier Ltd. 2018:51–68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4515207/.
Pidhatika B, Rodenstein M, Chen Y, Rakhmatullina E, Mühlebach A, Acikgöz C, et al. Comparative stability studies of Poly(2-methyl-2-oxazoline) and Poly(ethylene glycol) brush coatings. Biointerphases. 2012;7:1–4. https://doi.org/10.1007/s13758-011-0001-y.
Muppalaneni S. Polyvinyl alcohol in medicine and pharmacy: a perspective. J Dev Drugs. 2013;02(03):1–5. https://doi.org/10.4172/2329-6631.1000112.
Aslam M, Kalyar MA, Raza ZA. Polyvinyl alcohol: a review of research status and use of polyvinyl alcohol based nanocomposites. Polym Eng Sci. 2018;58(12):2119–32. https://doi.org/10.1002/pen.24855.
Nagarkar R, Patel J. Polyvinyl alcohol : a comprehensive study. Acta Sci Pharm Sci. 2019;3(4):34–44.
Marin E, Rojas J, Ciro Y. A review of polyvinyl alcohol derivatives: promising materials for pharmaceutical and biomedical applications. African J Pharm Pharmacol. 2014;8(24):674–84. https://doi.org/10.5897/AJPP2013.3906.
Baker MI, Walsh SP, Schwartz Z, Boyan BD. A review of polyvinyl alcohol and its uses in cartilage and orthopedic applications. J Biomed Mater Res - Part B Appl Biomater. 2012;100 B(5):1451–7. https://doi.org/10.1002/jbm.b.32694.
Wu W, Tian H, Xiang A. Influence of polyol plasticizers on the properties of polyvinyl alcohol films fabricated by melt processing. J Polym Environ. 2012;20(1):63–9. https://doi.org/10.1007/s10924-011-0364-7.
Liu B, Zhang J. Research progress of polyvinyl alcohol water-resistant film materials Figure 1. The structural formula of PVA. 2022:1–13. https://doi.org/10.3390/membranes12030347.
Kurakula M, Rao GSNK. Pharmaceutical assessment of polyvinylpyrrolidone (PVP): As excipient from conventional to controlled delivery systems with a spotlight on COVID-19 inhibition. 2020;60:102046. https://doi.org/10.1016/j.jddst.2020.102046.
Haaf F, Sanner A, Straub F. Polymers of N-Vinylpyrrolidone: Synthesis, Characterization and Uses. 1985;17(I):143–52.
Teodorescu M, Bercea M. Poly ( vinylpyrrolidone ) – A versatile polymer for biomedical and beyond medical poly (vinylpyrrolidone ) – a versatile polymer for biomedical and beyond medical applications. 2016:923–43. https://doi.org/10.1080/03602559.2014.979506.
Franco P, De Marco I. The use of poly(N-vinyl pyrrolidone) in the delivery of drugs: a review. Polymers (Basel). 2020;12(5):18–21. https://doi.org/10.3390/polym12051114.
Kurakula M, Rao GSNK. Pharmaceutical assessment of polyvinylpyrrolidone (PVP): as excipient from conventional to controlled delivery systems with a spotlight on COVID-19 inhibition. J Drug Deliv Sci Technol. 2020;60:102046. https://doi.org/10.1016/j.jddst.2020.102046.
Khan I, Mansha M. Polymer blends. 2019. 513–549 p.
Bartczak Z, Galeski A. Mechanical properties of polymer blends. 2014:1203–97. https://doi.org/10.1007/978-94-007-6064-6_13.
Guo Q. Polymer morphology. 2018;(April 2016).
Costa MS, Franco CML, Grossman MVE. Produção e caracterização estrutural, molecular e morfológica de nanocristais a partir de diferentes amidos e sua aplicação em biofilmes. 2017;0104–7760:423–34.
Li J, Zivanovic S, Davidson PM, Kit K. Characterization and comparison of chitosan/PVP and chitosan/PEO blend films. Carbohydr Polym. 2010;79(3):786–91. https://doi.org/10.1016/j.carbpol.2009.09.028.
Silva AR, Carreira P, Santos C, Reis M, Mateus AI. Film: using electrospinning to create bioactive films. Appl Mech Mater. 2019;890:260–7. https://doi.org/10.1002/jemt.24189.
Ghosal K, Chandra A, Praveen G, Snigdha S, Roy S, Agatemor C, et al. Electrospinning over solvent casting: tuning of mechanical properties of membranes. Sci Rep. 2018;8(1):1–9. https://doi.org/10.1038/s41598-018-23378-3.
Tijing LD, Woo YC, Yao M, Ren J, Shon HK. Electrospinning for membrane fabrication: strategies and applications. Comprehensive Membrane Science and Engineering. 2017:418–44. https://doi.org/10.1016/b978-0-12-409547-2.12262.
Zhao L, Duan G, Zhang G, Yang H, Jiang S, He S. Electrospun functional materials toward food packaging applications: a review. Nanomaterials. 2020;10(1). https://doi.org/10.3390/nano10010150.
Wang XX, Yu GF, Zhang J, Yu M, Ramakrishna S, Long YZ. Conductive polymer ultrafine fibers via electrospinning: preparation, physical properties and applications. Prog Mater Sci. 2021;115(405):100704. https://doi.org/10.1016/j.pmatsci.2020.100704.
Bambole V, Yakhmi JV. Tissue engineering: use of electrospinning technique for recreating physiological functions [Internet]. Nanobiomaterials in soft tissue engineering: applications of nanobiomaterials. Elsevier Inc. 2016:387–455. https://doi.org/10.1016/B978-0-323-42865-1.00014-3.
Nune SK, Rama KS, Dirisala VR, Chavali MY. Electrospinning of collagen nanofiber scaffolds for tissue repair and regeneration. Nanostructures for novel therapy: synthesis. characterization and applications. 2017:281–311. https://doi.org/10.3390/ijms23169206.
Microbiol C, Ahire JJ, Dicks LMT. Antimicrobial hyaluronic acid – cefoxitin sodium thin films produced by electrospraying. Curr Microbiol. 2016;73(2):236–41. https://doi.org/10.1007/s00284-016-1057-1.
Kumar S, Li X, Xie J. Electrospraying an enabling technology for pharmaceutical and biomedical applications : a review. 2018;125:164–81. https://doi.org/10.1016/j.jaerosci.2018.04.002.
Kashif M, Khan I, Schutyser MAI, Schroën K, Boom R. The potential of electrospraying for hydrophobic film coating on foods. J Food Eng. 2012;108(3):410–6. https://doi.org/10.1016/j.jfoodeng.2011.09.005.
Wang J, Jansen JA, Yang F. Electrospraying: possibilities and challenges of engineering carriers for biomedical applications - a mini review. Front Chem. 2019;7:1–9. https://doi.org/10.3389/fchem.2019.00258.
Rizwan M, Tse JW, Nori A, Leong KW, Yim EKF. Cell–substrate interactions. Principles of regenerative medicine. 2019:437–68. https://doi.org/10.1016/b978-0-12-809880-6.00027-8.
Stanković M, Frijlink HW, Hinrichs WLJ. Polymeric formulations for drug release prepared by hot melt extrusion: application and characterization. Drug Discov Today. 2015;20(7):812–23. https://doi.org/10.1016/j.drudis.2015.01.012.
Tiwari RV, Patil H, Repka MA. Contribution of hot-melt extrusion technology to advance drug delivery in the 21st century. Expert Opin Drug Deliv. 2016;13(3):451–64. https://doi.org/10.1517/17425247.2016.1126246.
Thakkar R, Thakkar R, Pillai A, Ashour EA, Repka MA. Systematic screening of pharmaceutical polymers for hot melt extrusion processing: a comprehensive review. Int J Pharm. 2020;576:118989. https://doi.org/10.1016/j.ijpharm.2019.118989.
Censi R, Gigliobianco MR, Casadidio C, Di Martino P. Hot melt extrusion: highlighting physicochemical factors to be investigated while designing and optimizing a hot melt extrusion process. Pharmaceutics. 2018;11;10(3):89. https://doi.org/10.3390/pharmaceutics10030089.
Maniruzzaman M, Boateng JS, Snowden MJ, Douroumis D. A review of hot-melt extrusion: process technology to pharmaceutical products. ISRN Pharm. 2012;2012:1–9. https://doi.org/10.5402/2012/436763.
Musazzi UM, Khalid GM, Selmin F, Minghetti P, Cilurzo F. Trends in the production methods of orodispersible films. Int J Pharm. 2020;576:118963. https://doi.org/10.1016/j.ijpharm.2019.118963.
Dixit RP, Puthli SP. Oral strip technology: overview and future potential. J Control Release. 2009;139(2):94–107. https://doi.org/10.1016/j.jconrel.2009.06.014.
Anbukarasu P, Sauvageau D, Elias A. Tuning the properties of polyhydroxybutyrate films using acetic acid via solvent casting. Sci Rep. 2015;5:1–14. https://doi.org/10.1038/srep17884.
Karki S, Kim H, Na SJ, Shin D, Jo K, Lee J. Thin films as an emerging platform for drug delivery. Asian J Pharm Sci. 2016;11(5):559–74. https://doi.org/10.1016/j.ajps.2016.05.004.
Notario-Pérez F, Cazorla-Luna R, Martín-Illana A, Galante J, Ruiz-Caro R, das Neves J, et al. Design, fabrication and characterisation of drug-loaded vaginal films: state-of-the-art. J Controlled Release. 2020;327:477–99. https://doi.org/10.1016/j.jconrel.2020.08.032.
Yu J, Park SA, Kim WD, Ha T, Xin YZ, Lee J, et al. Current advances in 3D bioprinting technology and its applications for tissue engineering. Polymers (Basel). 2020;12(12):1–30. https://doi.org/10.3390/polym12122958.
Agarwal S, Saha S, Balla VK, Pal A, Barui A, Bodhak S. Current developments in 3D bioprinting for tissue and organ regeneration–a review. Front. Mech Eng. 2020;6. https://doi.org/10.3389/fmech.2020.589171.
Tsegay F, Elsherif M, Butt H. Smart 3D printed hydrogel skin wound bandages: a review. Polymers (Basel). 2022;14(5). https://doi.org/10.3390/polym14051012.
Vanaei S, Parizi MS, Vanaei S, Salemizadehparizi F, Vanaei HR. An overview on materials and techniques in 3D bioprinting toward biomedical application. Eng Regen. 2021;2(November2020):1–18. https://doi.org/10.1016/j.engreg.2020.12.001.
Ali A, Ahmad U, Akhtar J. 3D printing in pharmaceutical sector: an overview. Intech. 2012;13. https://doi.org/10.1016/j.colsurfa.2011.12.014.
Ortiz-Acosta D, Moore T. Functional 3D printed polymeric materials. Intech. 2012;13. https://doi.org/10.1016/j.colsurfa.2011.12.014.
Bishop ES, Mostafa S, Pakvasa M, Luu HH, Lee MJ, Wolf JM, et al. 3-D bioprinting technologies in tissue engineering and regenerative medicine: current and future trends. Genes Dis. 2017;4(4):185–95. https://doi.org/10.1016/j.gendis.2017.10.002.
Valenta C. The use of mucoadhesive polymers in vaginal delivery, Vol. 57. Adv Drug Deliv Rev Elsevier. 2005:1692–712. https://doi.org/10.1016/j.addr.2011.02.005.
Chen G, Dong S, Zhao S, Li S, Chen Y. Improving functional properties of zein film via compositing with chitosan and cold plasma treatment. Ind Crops Prod. 2019;129:318–26. https://doi.org/10.1016/j.indcrop.2018.11.072.
Timur SS, Yüksel S, Akca G, Şenel S. Localized drug delivery with mono and bilayered mucoadhesive films and wafers for oral mucosal infections. Int J Pharm. 2019;559:102–12. https://doi.org/10.1016/j.ijpharm.2019.01.029.
Notario-Pérez F, Martín-Illana A, Cazorla-Luna R, Ruiz-Caro R, Bedoya LM, Peña J, et al. Development of mucoadhesive vaginal films based on HPMC and zein as novel formulations to prevent sexual transmission of HIV. Int J Pharm. 2019;570:118643. https://doi.org/10.1016/j.ijpharm.2019.118643.
Srisuwan Y, Baimark Y. Mechanical properties and heat resistance of stereocomplex polylactide/copolyester blend films prepared by in situ melt blending followed with compression molding. Heliyon. 2018;4(12):e01082. https://doi.org/10.1016/j.heliyon.2018.e01082.
Zhang H, Zhang J, Streisand JB. Oral mucosal drug delivery: clinical pharmacokinetics and therapeutic applications. Clin Pharmacokinet. 2002;41(9):661–80. https://doi.org/10.2165/00003088-200241090-00003.
Rossi S, Sandri G, Caramella CM. Buccal drug delivery: a challenge already won? Drug Discov Today Technol. 2005;2(1):59–65. https://doi.org/10.1016/j.ddtec.2005.05.018.
Groeger S, Meyle J. Oral mucosal epithelial cells. Front Immunol. 2019;10:1–22. https://doi.org/10.3389/fimmu.2019.00208.
Lam JKW, Xu Y, Worsley A, Wong ICK. Oral transmucosal drug delivery for pediatric use. Adv Drug Deliv Rev. 2014;73:50–62. https://doi.org/10.1016/j.addr.2013.08.011.
Squier CA, Kremer MJ. Biology of oral mucosa and esophagus. J Natl Cancer Inst Monogr. 2001;52242(29):7–15. https://doi.org/10.1093/oxfordjournals.jncimonographs.a003443.
Fonseca-Santos B, Satake CY, Calixto GMF, Dos Ssantos AM, Chorilli M. Trans-resveratrol-loaded nonionic lamellar liquid-crystalline systems: structural, rheological, mechanical, textural, and bioadhesive characterization and evaluation of in vivo anti-inflammatory activity. Int J Nanomedicine. 2017;12:6883–93. https://doi.org/10.2147/IJN.S138629.
Bruschi ML, de Freitas O. Oral bioadhesive drug delivery systems. Drug Dev Ind Pharm. 2005;31(3):293–310. https://doi.org/10.1081/ddc-52073.
Mazzarino L, Borsali R, Lemos-Senna E. Mucoadhesive films containing chitosan-coated nanoparticles: a new strategy for buccal curcumin release. J Pharm Sci. 2014;103(11):3764–71. https://doi.org/10.1002/jps.24142.
Camargo LG, De FP, Remiro R, Rezende G, Di CS, Franz-montan M, et al. Development of bioadhesive polysaccharide-based films for topical release of the immunomodulatory agent imiquimod on oral mucosa lesions. Eur Polym J. 2021;110422. https://doi.org/10.1002/jps.23386.
Vecchi CF, Said dos Santos R, Bassi da Silva J, Rosseto HC, Sakita KM, Svidzinski TIE, et al. Development and in vitro evaluation of buccal mucoadhesive films for photodynamic inactivation of Candida albicans. Photodiagnosis Photodyn Ther. 2020;32:101957. https://doi.org/10.1016/j.pdpdt.2020.101957.
Jovanović M, Petrović M, Cvijić S, Tomić N, Stojanović D, Ibrić S, et al. 3d printed buccal films for prolonged-release of propranolol hydrochloride: development, characterization and bioavailability prediction. Pharmaceutics. 2021;13(12). https://doi.org/10.3390/pharmaceutics13122143.
Abouhussein D, El Nabarawi MA, Shalaby SH, El-Bary AA. Cetylpyridinium chloride chitosan blended mucoadhesive buccal films for treatment of pediatric oral diseases. J Drug Deliv Sci Technol. 2020;57:101676. https://doi.org/10.1016/j.jddst.2020.101676.
Khiev D, Mohamed ZA, Vichare R, Paulson R, Bhatia S, Mohapatra S, et al. Emerging nano-formulations and nanomedicines applications for ocular drug delivery. Nanomaterials. 2021;11(1):1–19. https://doi.org/10.3390/nano11010173.
Tsai CH, Wang PY, Lin IC, Huang H, Liu GS, Tseng CL. Ocular drug delivery: role of degradable polymeric nanocarriers for ophthalmic application. Int J Mol Sci. 2018;19(9). https://doi.org/10.3390/ijms19092830.
Wu Y, Liu Y, Li X, Kebebe D, Zhang B, Ren J, et al. Research progress of in-situ gelling ophthalmic drug delivery system. Asian J Pharm Sci. 2019;14(1):1–15. https://doi.org/10.1016/j.ajps.2018.04.008.
Gholizadeh S, Wang Z, Chen X, Dana R, Annabi N. Advanced nanodelivery platforms for topical ophthalmic drug delivery. Drug Discov Today. 2021;26(6):1437–49. https://doi.org/10.1016/j.drudis.2021.02.027.
Zhu M, Wang J, Li N. A novel thermo-sensitive hydrogel-based on poly(N-isopropylacrylamide)/hyaluronic acid of ketoconazole for ophthalmic delivery. Artif Cells, Nanomedicine Biotechnol. 2018;46(6):1282–7. https://doi.org/10.1080/21691401.2017.1368024.
Kirchhof S, Goepferich AM, Brandl FP. Hydrogels in ophthalmic applications. Eur J Pharm Biopharm. 2015;95:227–38. https://doi.org/10.1016/j.ejpb.2015.05.016.
Nyamweya NN. Applications of polymer blends in drug delivery. Futur. J Pharm Sci. 2021;7(1). https://doi.org/10.1016/j.eurpolymj.2013.01.019.
El-Sousi S, Nácher A, Mura C, Catalán-Latorre A, Merino V, Merino-Sanjuán M, et al. Hydroxypropylmethylcellulose films for the ophthalmic delivery of diclofenac sodium. J Pharm Pharmacol. 2013;65(2):193–200. https://doi.org/10.1111/j.2042-7158.2012.01587.x.
Tighsazzadeh M, Mitchell JC, Boateng JS. Development and evaluation of performance characteristics of timolol-loaded composite ocular films as potential delivery platforms for treatment of glaucoma. Int J Pharm. 2019;566:111–25. https://doi.org/10.1016/j.ijpharm.2019.05.059.
Boateng JS, Popescu AM. Composite bi-layered erodible films for potential ocular drug delivery. Colloids Surfaces B Biointerfaces. 2016;145:353–61. https://doi.org/10.1016/j.colsurfb.2016.05.014.
Haque T, MMU T. Chemical enhancer: a simplistic way to modulate barrier function of the stratum corneum. Adv Pharm Bull. 2018, 8;(2):169–79. https://doi.org/10.15171/apb.2018.021.
Domínguez-Delgado CL, Rodríguez-Cruz IM, López-Cervantes M. The skin: a valuable route for administration of drugs. Curr Technol to Increase Transdermal Deliv. Drugs. 2010;1–22. https://doi.org/10.2174/978160805191511001010001.
Supe S, Takudage P. Methods for evaluating penetration of drug into the skin : a review. 2020;2019:1–10. https://doi.org/10.1111/srt.12968.
Alborzi Z, Izadi-Vasafi H, Ghayoumi F. Wound dressings based on chitosan and gelatin containing starch, sesame oil and banana peel powder for the treatment of skin burn wounds. 2021:1–l6. https://doi.org/10.1007/s10965-021-02427-y.
de Souza Cintra GA, Pinto LA, Calixto GMF, Soares CP, de Souza Von Zuben E, Scarpa MV, et al. 2016;21(2):1–13. https://doi.org/10.3390/molecules21020231.
Louize G, Olivato JB. Antimicrobial dressing of silver sulfadiazine-loaded halloysite/cassava starch-based ( bio) nanocomposites. 2021;35(9). https://doi.org/10.1177/0885328221995920.
Feng Y, Wang Q, He M, Zhao W, Liu X, Zhao C. Nonadherent zwitterionic composite nanofibrous membrane with a halloysite nanocarrier for sustained wound anti-infection and cutaneous regeneration. 2020;6(1):621–33. https://doi.org/10.1021/acsbiomaterials.9b01547.
Zhang D, Zhou W, Wei B, Wang X, Tang R, Nie J, et al. Carboxyl-modified poly (vinyl alcohol) -crosslinked chitosan hydrogel films for potential wound dressing. Carbohydr Polym. 2015;125:189–99. https://doi.org/10.1016/j.carbpol.2015.02.034.
Zorec B, Preat V, Miklavcic D, Pavselj N. Active enhancement methods for intra- and transdermal drug delivery: a review. 2013;82:5. https://doi.org/10.6016/1889.
Nagadev C, Rao MDS, Venkatesh P, Hepcykalarani D, Prema R. A review on transdermal drug delivery systems. Asian J Res Pharm Sci. 2020;10(2):109. https://doi.org/10.5958/2231-5659.2020.00021.1.
Saravanakumar K, Swapna P, Nagaveni P, Vani P, Pujitha K. Transdermal drug delivery system: a review. J Glob Trends Pharm Sci. 2015;6(1):2485–90. https://doi.org/10.18231/j.ijpp.2021.002.
Dhote V, Bhatnagar P, Mishra PK, Mahajan SC, Mishra DK. Iontophoresis: a potential emergence of a transdermal drug delivery system. Sci Pharm. 2012;80(1):1–28. https://doi.org/10.3797/scipharm.1108-20.
Kasetvatin C, Rujivipat S, Tiyaboonchai W. Combination of elastic liposomes and low frequency ultrasound for skin permeation enhancement of hyaluronic acid. Colloids surfaces B biointerfaces. 2015;135:458–64. https://doi.org/10.1016/j.colsurfb.2015.07.078.
Yarmush ML, Golberg A, Serša G, Kotnik T, Miklavčič D. Electroporation-based technologies for medicine: principles, applications, and challenges. Annu Rev Biomed Eng. 2014;16:295–320. https://doi.org/10.1146/annurev-bioeng-071813-104622.
Prabhakar D, Sreekanth J, Jayaveera KN. Transdermal drug delivery patches: a review. J Drug Deliv Ther. 2013;3(4):213–21. https://doi.org/10.22270/jddt.v3i4.590.
Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev. 2004;56(5):603–18. https://doi.org/10.1016/j.addr.2012.09.032.
Jamakandi VG, Mulla JS, Vinay BL, Shivakumar HN. Formulation, characterization, and evaluation of matrix-type transdermal patches of a model antihypertensive drug. Asian J Pharm. 2009;3(1):59–65. https://doi.org/10.22377/ajp.v3i1.243.
Shah S, Prabhu P, Gundad S. Formulation development and investigation of domperidone transdermal patches. Int J Pharm Investig. 2011;1(4):240. https://doi.org/10.4103/2230-973X.93008.
Ariamoghaddam AR, Ebrahimi-Hosseinzadeh B, Hatamian-Zarmi A, Sahraeian R. In vivo anti-obesity efficacy of curcumin loaded nanofibers transdermal patches in high-fat diet induced obese rats. Mater Sci Eng C. 2018;92(July):161–71. https://doi.org/10.1016/j.msec.2018.06.030.
Hussain A, Ahsan F. The vagina as a route for systemic drug delivery. Journal of Controlled Release. J Control Release. 2005;103:301–13. https://doi.org/10.1016/j.jconrel.2004.11.034.
Machado RM, Palmeira-De-Oliveira A, Martinez-De-Oliveira J, Palmeira-De-Oliveira R. Vaginal films for drug delivery. Journal of Pharmaceutical Sciences. John Wiley and Sons Inc. 2013;13:2069–81. https://doi.org/10.1002/jps.23577.
das Neves J, Amaral MH, Bahia MF. Vaginal drug delivery. In: Pharmaceutical Manufacturing Handbook. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2007. p. 809–78.
Harwood B, Mishell DRJ. Contraceptive vaginal rings. Semin Reprod Med. 2001;19(4):381–90. https://doi.org/10.1055/s-2001-18646.
Bunge KE, Dezzutti CS, Hendrix CW, Marzinke MA, Spiegel HML, Moncla BJ, et al. FAME-04: A Phase 1 trial to assess the safety, acceptability, pharmacokinetics and pharmacodynamics of film and gel formulations of tenofovir. J Int AIDS Soc. 2018;21(8):e25156. https://doi.org/10.1002/jia2.25156.
Ghosal K, Taran Hazra B, BrataBhowmik B, Thomas S. Formulation development, physicochemical characterization and in vitro-in vivo drug release of vaginal films. Curr HIV Res. 2016;14(4):295–306. https://doi.org/10.2174/1570162x14666151113123040.
Sobel JD. Vulvovaginal candidosisv, Vol. 369, Lancet. Elsevier. 2007;369(9577):1961–71. https://doi.org/10.1016/S0140-6736(07)60917-9.
Nematpour N, Moradipour P, Zangeneh MM, Arkan E, Abdoli M, Behbood L. The application of nanomaterial science in the formulation a novel antibiotic: assessment of the antifungal properties of mucoadhesive clotrimazole loaded nanofiber versus vaginal films. Mater Sci Eng C. 2020;110:110635. https://doi.org/10.1016/j.msec.2020.110635.
Dobaria NB, Badhan AC, Mashru RC. A novel itraconazole bioadhesive film for vaginal delivery: design, optimization, and physicodynamic characterization. AAPS PharmSciTech. 2009;10(3):951–9. https://doi.org/10.1208/s12249-009-9288-0.
Borumand M, Mortazavi SA, Jafari Azar Z, Teymouri RR. Development and in vitro evaluation of a novel contraceptive vaginal mucoadhesive propranolol hydrochloride film. J Drug Deliv Sci Technol. 2014, 24(6):637–44. https://doi.org/10.22037/IJPR.2012.1059.
Acknowledgements
All figures were made by Lorena Cararotto do Amaral. The professional English editing was done by Prof. Dr. Paulo Cesar Ribeiro Filho (University of São Paulo, FFLCH-USP).
Funding
This study was financed in part by the Coordenacão de Aperfeiçoamento Pessoal de Nível Superior, Brasil (CAPES), Finance Code 001, São Paulo Research Foundation–FAPESP (grant number 2019/00164–0), CNPq (Brasília, Brazil), and PACD-FCFAr-UNESP (Araraquara, Brazil).
Author information
Authors and Affiliations
Contributions
Conceptualization: Bruno Riccio, Amanda Silvestre, Andreia Meneguin, Franciele Baveloni, Tais Ribeiro, and Marlus Chorilli. Investigation: Bruno Riccio, Amanda Silvestre, Andreia Meneguin, Franciele Baveloni, and Tais Ribeiro. Resources: Marlus Chorilli. Writing—original draft preparation: Bruno Riccio, Amanda Silvestre, Andreia Meneguin, Franciele Baveloni, and Tais Ribeiro. Writing—review and editing: Priscileila Ferrari and Marlus Chorilli. Supervision: Andreia Meneguin, Priscileila Ferrari, and Marlus Chorilli. Project administration: Priscileila Ferrari and Marlus Chorilli.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Riccio, B.V.F., Silvestre, A.L.P., Meneguin, A.B. et al. Exploiting Polymeric Films as a Multipurpose Drug Delivery System: a Review. AAPS PharmSciTech 23, 269 (2022). https://doi.org/10.1208/s12249-022-02414-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-022-02414-6