Abstract
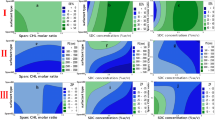
Transdermal drug delivery systems (TDDSs) were developed for prolonged tamsulosin (TMS) delivery. Double layer (DL) TDDSs were prepared using Eudragit® RL by conventional film-forming. Ethylene-vinyl acetate was used as the backing layer, triethylcitrate as plasticizer, and Capmul® PG-8-70 NF and Captex 170 EP as penetration enhancers (PEs). An increase in either drug or PE concentration caused a significant increase in drug permeation flux. Modulation of drug permeation across Strat-M® membrane was examined using a single layer (SL) having the same thickness and drug content as the DLs, while the DLs were formulated to have variable drug spatial distribution across each layer (DL 4:6 and DL 6:4). SL/TDDS showed significantly higher daily drug permeation than DL/TDDSs for the first 4 days which could be related to the presence of high TMS concentration located on the upper surface of SL/TDDS as a result of solute migration of TMS during the drying process. However, this increase was followed by a progressive linear decrease after 5 days. Deflection points that were characterized by lower drug flux had been shown by SL/TDDS at more than one-point times. In contrast, DL 4:6 and DL 6:4 TDDSs demonstrated an ability to sustain TMS delivery for up to 2 weeks.
Graphical Abstract







Similar content being viewed by others
References
Dunn CJ, Matheson A, Faulds DM. Tamsulosin: a review of its pharmacology and therapeutic efficacy in the management of lower urinary tract symptoms. Drugs Aging. 2002;19(2):135–61. https://doi.org/10.2165/00002512-200219020-00004.
Chughtai B, Forde JC, Thomas DD, Laor L, Hossack T, Woo HH, et al. Benign prostatic hyperplasia. Nat Rev Dis Primers. 2016;2(1):16031. https://doi.org/10.1038/nrdp.2016.31.
Unnikrishnan R, Almassi N, Fareed K. Benign prostatic hyperplasia: evaluation and medical management in primary care. Clev Clin J Med. 2017;84(1):53–64. https://doi.org/10.3949/ccjm.84a.16008.
Abrams P, Speakman M, Stott M, Arkell D, Pocock R. A dose-ranging study of the efficacy and safety of tamsulosin, the first prostate-selective alpha 1A-adrenoceptor antagonist, in patients with benign prostatic obstruction (symptoms benign prostatic hyperplasia). Br J Urol. 1997;80(4):587–96. https://doi.org/10.1046/j.1464-410x.1997.00380.x.
Kawahara K, Nakao K, Yamaki H. Inventors. Tamsulosin-containing transdermal patch. U.S. Patent US 2009/0155343 A1, 2009.
Chapple CR. The oral controlled absorption system (OCAS®): the evolution of tamsulosin for the treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH). Eur Urol Suppl. 2005;4(7):20–2. https://doi.org/10.1016/j.eursup.2005.07.006.
Emberton M, Cornel EB, Bassi PF, Fourcade RO, Gómez JMF, Castro R. Benign prostatic hyperplasia as a progressive disease: a guide to the risk factors and options for medical management. Int J Clin Pract. 2008;62(7):1076–86. https://doi.org/10.1111/j.1742-1241.2008.01785.x.
Chaplin S, Kirby R. Alpha-blockers in the treatment of benign prostatic hypertrophy. Prescriber. 2013;24(4):13–5. https://doi.org/10.1002/psb.1015.
Prausnitz M, Langer R. Transdermal drug delivery Nat biotechnol. 2008;26:1261–8. https://doi.org/10.1038/nbt.1504.
Jeong WY, Kwon M, Choi HE, Kim KS. Recent advances in transdermal drug delivery systems: a review. Biomater Res. 2021;25:24. https://doi.org/10.1186/s40824-021-00226-6.
PubChem Compound Summary for CID 129211, Tamsulosin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/129211. Accessed 31 Jan 2022.
Franco-Salinas G, de la Rosette JJ, Michel MC. Pharmacokinetics and pharmacodynamics of tamsulosin in its modified-release and oral controlled absorption system formulations. Clin Pharmacokinet. 2010;49(3):177–88. https://doi.org/10.2165/11317580-000000000-00000.
Ma X, Audett J, Soni PL, Singh N, Bailey SE. Inventors. Transdermal drug delivery system for the administration of tamsulosin, and related compositions and methods of use. U.S. Patent US 5,843,472 A, 1998.
Wang Z, Itoh Y, Hosaka Y, Kobayashi I, Nakano Y, Maeda I, et al. Novel transdermal drug delivery system with polyhydroxyalkanoate and starburst polyamidoamine dendrimer. J Biosci Bioeng. 2003;95(5):541–3. https://doi.org/10.1016/S1389-1723(03)80059-2.
Singh P, Lee ES, Jain AK. Inventors. Transdermal administration of tamsulosin. U.S. Patent US 9610253 B2, 4 April 2017.
Almehmady AM, Elsisi AM. Development, optimization, and evaluation of tamsulosin nanotransfersomes to enhance its permeation and bioavailability. JDDST. 2020;57:101667. https://doi.org/10.1016/j.jddst.2020.101667.
Ciríaco SL, Carvalho IPS, Alves Terceiro Neto J, de Sousa Lima Neto J, DHB d O, Cunha APGP, et al. Development of microemulsion of tamsulosin and dutasteride for benign prostatic hyperplasia therapy. Colloids Surf B Biointerfaces. 2020;185:110573. https://doi.org/10.1016/j.colsurfb.2019.110573.
Assaf SM, Sallam AS, Ghanem AM. Design and evaluation of transdermal delivery system containing tamsulosin hydrochloride. JDDST. 2019;51:524–34. https://doi.org/10.1016/j.jddst.2019.03.023.
Gao Y, Liang J, Liu J, Xiao Y. Double-layer weekly sustained release transdermal patch containing gestodene and ethinylestradiol. Int J Pharm. 2009;377(1–2):128–34. https://doi.org/10.1016/j.ijpharm.2009.05.017.
Davis DA, Martins PP, Zamloot MS, Kucera SA, Williams RO 3rd, Smyth HDC, Warnken ZN. Complex drug delivery systems: controlling transdermal permeation rates with multiple active pharmaceutical ingredients. AAPS PharmSciTech. 2020;21(5):165. https://doi.org/10.1208/s12249-020-01682-4.
Abitec announces two lipid enhancers for drug delivery. Available online: https://www.abiteccorp.com/en/news-and-events/news/abitec-announces-two-lipid-enhancers-for-drug-delivery/. Accessed 31 Jan 2022.
Gwak HS, Chun IK. Effect of vehicles and penetration enhancers on the in vitro percutaneous absorption of tenoxicam through hairless mouse skin. Int J Pharm. 2002;236(1–2):57–64. https://doi.org/10.1016/s0378-5173(02)00009-1.
Cho YA, Gwak HS. Transdermal delivery of ketorolac tromethamine: effects of vehicles and penetration enhancers. Drug Dev Ind Pharm. 2004;30(6):557–64. https://doi.org/10.1081/ddc-120037486.
Theobald F, Rubenacher R. Inventors. LTS Lohmann Therapie Systeme GmbH and Co KG, Assignee. Transmittal therapeutic systems containing steroid hormones and propylene glycol monocaprylate. U.S. Patent US 20050118244 A1, 2 June 2005.
Cho CW, Kim DB, Cho HW, Shin SC. Enhanced controlled transdermal delivery of ambroxol from the EVA matrix. Indian J Pharm Sci. 2012;74(2):127–32. https://doi.org/10.4103/0250-474X.103844.
Haque T, Talukder MMU. Chemical enhancer: a simplistic way to modulate barrier function of the stratum corneum. Adv Pharm Bull. 2018;8(2):169–79. https://doi.org/10.15171/apb.2018.021.
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C, et al. DDSolver: an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010;12(3):263–71. https://doi.org/10.1208/s12248-010-9185-1.
Experience the unmatched predictability of Strat-M™ membrane. Available online: https://dicsa.es/assets/downloads/2018-13609_Strat-M_membrane_product_brochure_MRK_Web_DP.pdf. Accessed 31 Jan 2022.
Pan TL, Wang PW, Aljuffali IA, Hung YY, Lin CF, Fang JY. Dermal toxicity elicited by phthalates: evaluation of skin absorption, immunohistology, and functional proteomics. Food Chem Toxicol. 2014;65:105–14. https://doi.org/10.1016/j.fct.2013.12.033.
Flaten GE, Palac Z, Engesland A, Filipović-Grčić J, Vanić Ž, Škalko-Basnet N. In vitro skin models as a tool in optimization of drug formulation. Eur J Pharm Sci. 2015;75:10–24. https://doi.org/10.1016/j.ejps.2015.02.018.
Li J, Lee IW, Shin GH, Chen X, Park HJ. Curcumin-Eudragit® E PO solid dispersion: a simple and potent method to solve the problems of curcumin. Eur J Pharm Biopharm. 2015;94:322–32. https://doi.org/10.1016/j.ejpb.2015.06.002.
Uchida T, Kadhum WR, Kanai S, Todo H, Oshizaka T, Sugibayashi K. Prediction of skin permeation by chemical compounds using the artificial membrane, Strat-M™. Eur J Pharm Sci. 2015;67:113–8. https://doi.org/10.1016/j.ejps.2014.11.002.
Beriro DJ, Cave MR, Wragg J, Thomas R, Wills G, Evans F. A review of the current state of the art of physiologically-based tests for measuring human dermal in vitro bioavailability of polycyclic aromatic hydrocarbons (PAH) in soil. J Hazard Mater. 2016;305:240–59. https://doi.org/10.1016/j.jhazmat.2015.11.010.
Simon A, Amaro MI, Healy AM, Cabral LM, de Sousa VP. Comparative evaluation of rivastigmine permeation from a transdermal system in the Franz cell using synthetic membranes and pig ear skin with in vivo-in vitro correlation. Int J Pharm. 2016;512(1):234–41. https://doi.org/10.1016/j.ijpharm.2016.08.052.
Haq A, Goodyear B, Ameen D, Joshi V, Michniak-Kohn B. Strat-M® synthetic membrane: permeability comparison to human cadaver skin. Int J Pharm. 2018;547(1–2):432–7. https://doi.org/10.1016/j.ijpharm.2018.06.012.
Salamanca CH, Barrera-Ocampo A, Lasso JC, Camacho N, Yarce CJ. Franz diffusion cell approach for pre-formulation characterisation of ketoprofen semi-solid dosage forms. Pharmaceutics. 2018;10(3):148. https://doi.org/10.3390/pharmaceutics10030148.
Acknowledgements
The authors would like to acknowledge the Target Chemicals, Jordan, for donating Eudragit® RL and Al Taqaddom Pharmaceuticals Industries, Jordan, for providing tamsulosin hydrochloride.
Funding
This research was funded by the Jordan University of Science and Technology grant number 20200116.
Author information
Authors and Affiliations
Contributions
Conceptualization, Assaf S.M., and Sallam A.A.; Methodology, Assaf S.M., Khalil E.A., and Sallam A.A.; validation, Assaf S.M., Ghanem A.M., and Sallam A.A.; formal analysis, Ghanem A.M.; investigation, Ghanem A.M. and Alhaj, S.A.; resources, Ghanem A.M. and Alhaj S.A.; data curation, Assaf S.M., Ghanem A.M., and Sallam A.A.; writing – original draft preparation, Assaf S.M.; Writing – Review & Editing, Assaf S.M., Ghanem A.M., Sallam A.A.; visualization, Ghanem A.M.; supervision, Assaf A.A., Sallam A.A., and Khalil E.A.; project administration, Assaf S.M. and Sallam A.A.; funding acquisition, Assaf S.M.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
SEM images of the Strat-M membrane: (A) before permeation study and after (B) one week and (C) two weeks of the permeation study at 2500x magnification power. (GIF 86 kb)
ESM 2
Two-week in vitro permeation profiles of TMS from P9 after storing at 5 °C (refrigerated), 30 °C/ 60% RH (30 degrees), and 40 °C/ 75% RH (40 degrees), through Strat-M® membrane into phosphate buffer (pH 6.8) at 32 ± 1 oC, compared with its permeation from a freshly prepared patch (mean ± RSD, n=3). (GIF 12 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Assaf, S.M., Ghanem, A.M., Alhaj, S.A. et al. Formulation and Evaluation of Eudragit® RL Polymeric Double Layer Films for Prolonged-Release Transdermal Delivery of Tamsulosin Hydrochloride. AAPS PharmSciTech 23, 210 (2022). https://doi.org/10.1208/s12249-022-02358-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-022-02358-x