Abstract
Encapsulating genetic material into biocompatible polymeric microparticles is a means to improving gene transfection while simultaneously decreasing the tendency for inflammatory responses; and can be advantageous in terms of delivering material directly to the lungs via aerosolization for applications such as vaccinations. In this study, we investigated the advantages of using polymeric microparticles carrying the luciferase reporter gene in increasing transfection efficiency in the readily transfectable HEK293 cell line and the difficult to transfect RAW264.7 cell line. The results indicated that there was a limit to the ratio of nitrogen in polyethylenimine (PEI) to phosphate in DNA (N/P ratio) beyond which further increases in transgene expression no longer, or only marginally, occurred. Microparticles encapsulating PEI:DNA nanoplexes induced cellular toxicity in a dose-dependent manner. PEGylation increased transgene expression, likely related to enhanced degradation of particles. Furthermore, intra-tracheal instillation in rats allowed us to investigate the inflammatory response in the lung as a function of PEGylation, porosity, and size. Porosity did not influence cell counts in bronchoalveolar lavage fluid in the absence of PEG, but in particles containing PEG, non-porous particles recruited fewer inflammatory cells than their porous counterparts. Finally, both 1 μm and 10 μm porous PLA-PEG particles recruited more neutrophils than 4 μm particles. Thus, we have shown that PEGylation and lack of porosity are advantageous for faster release of genetic cargo from microparticles and a reduced inflammatory response, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Vaccines are a powerful tool to prevent life-threatening infections. Vaccination has resulted in the eradication of smallpox (1), near eradication of polio (2), and H1N1 influenza viruses, which caused both the Spanish flu and Swine flu epidemics (3). Vaccines have also reduced the number of cases of liver cancer caused by hepatitis B (4), and cervical cancer caused by the human papillomavirus (HPV) (5,6). Both the hepatitis B vaccine and the HPV vaccine require repeated administration to establish immunity to the viruses. An alternative method of stimulating the immune system to fight infections is gene delivery, such as with plasmid DNA (pDNA). Although this option was proposed in 1990 using DNA encapsulated into liposomes, several challenges remain 30 years later for translating pDNA-based vaccines to clinical settings, and no DNA-based vaccines have yet been approved for human use (3,7).
One such translational challenge is effective gene delivery to the target site. DNA readily undergoes enzymatic degradation, which can be mitigated by implementing protective mechanisms. One such mechanism is polymeric encapsulation with biocompatible polymers, which is beneficial despite reduced nuclear entry (8,9,10,11,12,13,14,15,16). For example, the use of polyethylenimine (PEI) as a complexing agent imparts a positive charge on the DNA, which enhances cellular uptake (8,13,14,17,18,19). Further protections from degradation include using polymeric microparticles, which can also assist in pulmonary delivery due to their size. These polymeric microparticles are often developed from polymers found in FDA-approved devices and formulations, such as poly(lactic-co-glycolic-acid) (PLGA), or poly(lactic acid) (PLA) (20,21,22). Delivering these particles directly to the lungs is advantageous for treating conditions specific to the lungs, such as asthma or cystic fibrosis, because the lungs are a rich site for antigen-presenting cells and blood exchange. However, since the lungs are also a primary site for airborne pathogens, they also contain a robust defense system to remove xenobiotics from the body.
Several parameters can help with reducing this xenobiotic response within the lung, including tailoring the size and/or composition of the microparticles. Particle size may be tailored by changing the overall diameter of spherical particles, the morphology of particles, or by varying the porosity of particles which changes the effective diameter, also known as the aerodynamic diameter (23,24). The polymeric composition may be altered by including co-polymers, notably by using poly(ethylene glycol) (PEG). PEG is a hydrophilic and widely biocompatible polymer that enhances pulmonary absorption and retention via reduced phagocytic clearance (20,25,26).
In this study, PLGA, PLA, and PLA-PEG microparticles were loaded with pDNA nanoplexes and delivered to lung and kidney cells in vitro and to lung cells in vivo via intra-tracheal instillation in rats. In cell culture studies, a relationship between microparticle concentration and cell death was established, as well as the effect of time and dose on transgene expression of the luciferase reporter gene. The goal of the in vivo studies was to determine the extent to which microparticles elicited an immunogenic response, which is indicative of their proportional presumptive harm to the lungs. Total cell and neutrophil counts from the bronchoalveolar lavage fluid of rats indicated there was inflammation induced by microparticle exposure. Taken together, these results support the notion that polymeric microparticles can be developed as an effective genetic-based vaccine but with some degree of inflammatory response to the polymers comprising the microparticles.
MATERIALS AND METHODS
Materials
The PLA-PEG co-polymers used in this study have been previously described (23). PLGA monomers of D,L-lactide/glycolide at a 50:50 molar ratio and inherent viscosity of 0.47 dL/g were purchased from Absorbable Polymers International (Pelham, AL). Poly(vinyl alcohol) (PVA, Mw 30–70 kDa), reagent grade dichloromethane (DCM), ethyl acetate (EA), 88% hydrolyzed and branched PEI (Mw 25 kDa), and DNA from herring sperm were purchased from Sigma-Aldrich (St. Louis, MO). Cellgro was purchased from Fisher Scientific, Inc. (Hampton, NH), 0.9% sterile saline was purchased from Baxter, and Diff-Quik stain was purchased from Dade-Behring, Inc. (Deerfield, IL).
Plasmid Expansion and Extraction
Plasmid DNA was used to form nanoplexes. The VR1255 plasmid encoding firefly luciferase driven by the cytomegalovirus (CMV) promoter was used for these studies. Plasmids were transformed in Escherichia coli DH5α and amplified in Terrific Broth media at 37°C overnight in a rotary shaker at 300 rpm (New Brunswick Scientific Classic C24, New Brunswick, NJ). The pDNA from the expanded plasmid was isolated and purified using Qiagen Giga plasmid purification kit (QIAGEN, Hilden Germany) by following the manufacturer’s protocol. The concentration and purity of the pDNA were discerned by measuring the optical density (OD) at 260 nm and 280 nm in a microplate spectrophotometer (Spectramax Plus 384, Molecular Devices, San Jose, CA). The purity was obtained from the OD280/OD260 and the final concentration from OD260.
Nanoplex Preparation
Nanoplexes were prepared as previously published (13,23). Briefly, PEI and herring sperm DNA or pDNA were added in a nitrogen/phosphate (N/P) ratio of 15:1 in 1 mL of 0.25% PVA solution. The sample was vortexed for 30 s and allowed to sit at room temperature for 30 min to complete complexation.
Microsphere Preparation
The double emulsion solvent evaporation method was used to form microspheres. For non-porous microspheres, the primary emulsion consisting of an oil phase (3% w/v PLA-PEG or 0.75% PLGA, 7% w/v DCM, and 3% v/v EA) and water phase (nanoplexes in PVA and water) was sonicated (Sonics & Materials Inc., Newtown, CT) for 10 s. This solution was added to a 22 G needle and injected into a 2% PVA solution at room temperature. This resultant double emulsion was homogenized (T 25 Digital ULTRA-TURRAX®, IKA Works, Inc., Wilmington, NC) for 10 s at 7500 rpm with dispersed phase to continuous phase (DP/CP) ratio of 5. Microspheres were stirred slowly overnight and were subsequently washed thrice in ultrapure water and ultimately concentrated to 1 × 1010–2 × 1010 number concentration in a 0.9% sodium chloride solution.
The preparation method for porous microspheres differed in that the secondary emulsion contained 1% PVA and 1% sucrose rather than 2% PVA, and the DP/CP ratio was either 2 or 10 for 10 μm and 4 μm particles, respectively. Microspheres of 1 μm diameter were prepared with 0.5% w/v polymer and DP/CP equal to 1. The primary emulsion was instantaneously poured into a 2% PVA solution and homogenized at 10,000 rpm for 10 s. These were stirred for 5 min and placed on a hotplate for 3 h for solvent evaporation. Washing and concentration methods were the same for both porous and non-porous particles.
Cell Culture
Human embryonic kidney (HEK293) cells and murine macrophage (RAW264.7) cell lines were obtained from American Type Culture Collection (ATCC, Manasssas, VA). Cells were maintained in T75 flasks in an incubator at 37°C and 5% CO2; media used was Dulbecco’s Modified Essential Medium (DMEM, Life Technologies, Carlsbad, CA) supplemented with 10% v/v fetal bovine serum (FBS, Atlanta Biologicals, Flower Branch, GA), and 100 U/mL penicillin/100 μg/mL streptomycin (Invitrogen, Carlsbad, CA), hereon referred to as “complete media.”
Cytotoxicity In Vitro
Cytotoxicity of 4 μm, porous PLA-PEG particles was assessed with the MTT (3,[4,5-dimethylthiazol-2-y]-2, 5-diphenyl tetrazolium bromide) assay (Promega, Madison, WI). Cells were seeded in a 96-well tissue culture plate at a density of 1 × 104 cells/well. Cells were allowed to grow overnight prior to incubating with 200 μL of complete media containing microspheres at varying concentrations. After 4, 12, or 24 h of incubation, the media was replaced with 100 μL of fresh media. The MTT solution, suspended in 1X DPBS (Gibco, Waltham, MA) was added to each well and incubated for 2 h. Cells were lysed with 100 μL of 20% v/v sodium dodecyl sulfate (SDS) in 50% v/v DM at pH 4.7 overnight. The absorbance of the lysate at 550 nm was measured in a microplate spectrophotometer (Spectramax Plus 384, Molecular Devices), and the resultant values were compared with the control, which contained no microspheres.
Transfection Efficiency In Vitro
Cells were seeded in 12-well tissue culture plates at 1 × 105 cells/well and allowed to grow overnight. Microspheres (4 μm, porous PLA-PEG) were added into complete media at an equivalent dose of 1 μg DNA/well. Nanoplex transfection (i.e., without microsphere encapsulation) was achieved via seeding cells in 24-well plates at a density of 1 × 105 cells/well. The total DNA concentration was 0.2 μg/well. Nanoplexes were dosed to cells in serum-free media, then after 4 h, the media was replaced with complete media. Cells were allowed to grow for an additional 44 h (48 h total) prior to assessing luciferase expression. Cells were lysed with 200 μL lysis buffer (Promega) and subjected to three freeze-thaw cycles prior to centrifugation at 11,856 × g for 5 min. Luciferase was quantified using a luminometer (Lumat LB 9507, EG&G Berthold, Oak Ridge, TN). The luciferase assay (Promega) was mixed with cell supernatant (100 μL/20 μL, respectively) for 10 s. The total protein concentration in cell extract was measured using the Pierce BCA protein assay kit (Thermo Fisher Scientific) and used to normalize the luciferase activity.
Animals
Male Sprague Dawley rats (100–124 g weight) were purchased from Harlan Laboratories (Indianapolis, IN). Animals were quarantined in HEPA-filtered Thoren caging units at the Pulmonary Toxicology Facility at The University of Iowa for 12 days prior to initiating the experiment. Rats were supplied with food and water ad libitum and kept on a 12-h light-dark cycle. The animal protocol was approved by the Institutional Animal Care and Use Committee and complied with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
In Vivo Inflammation Measurements
Rats were exposed to polymeric microspheres by intra-tracheal instillation. Initially, animals were anesthetized with 5% isoflurane for 5 min or until the eyelid closure reflex was lost, using a precision vaporizer (Fortec Tec 3). Then during intubation and exposure to particles, animals were kept under anesthesia with 3% isoflurane. A 100 μL aliquot of particle suspension for one of 6 particle types (Table I), or of 0.9% sterile saline solution (control), was administered to each rat.
Bronchoalveolar lavage (BAL) fluid and lungs were collected 4 h after instillation to assess pulmonary inflammation. Animals were euthanized with isoflurane and exsanguinated through the heart. The trachea was exposed, cannulated with a 23 G catheter and lungs were washed 3 times with sterile 0.9% sodium chloride (5 mL each time). The recovered fluid was centrifuged (800 x g for 5 min at 4°C) and the cell pellet resuspended in Cellgro media, the total cell count in the pellet was determined using a hemocytometer. BAL cell types were ascertained by cytospinning and counting after Diff-Quik staining.
Statistical Analysis
Statistical analysis was performed in the GraphPad Prism software (GraphPad Software, San Diego, CA) using means, standard deviations, and n = 3 for cell counts. A two-way analysis of variance (ANOVA) with Tukey’s post-test was conducted for relative cell viability. A one-way ANOVA with Tukey’s post-test was run on cell counts. Multiple comparisons were conducted to determine statistically significant differences between specific groups. Significant differences are denoted by * (p < 0.05), ** (p < 0.01), *** (p < 0.001), **** (p < 0.0001), or “n.s.” for no significance.
RESULTS
Cytotoxicity of Microparticles
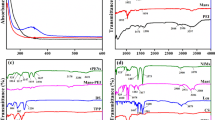
Blank porous PLA-PEG microparticles were administered to the readily transfectable cell line, HEK293, in vitro. Changes in the relative cell viability were used to indicate which incubation times and/or microparticle concentrations affected proliferation rates. Cell viability was assessed using the MTT assay at 4, 12, and 30 h after administering blank microparticles (Fig. 1). Dose did not have a significant effect on viability 4 h after administration; however, higher doses (12.5 and 25 mg/mL) significantly decreased cell viability at 30 h compared with the lower doses (Table S1). There was also a significant decrease in cell viability from 4 to 12 h for particles administered at both 12.5 mg/mL (p < 0.05) and 25 mg/mL (p < 0.01).
Encapsulated nanoplexes (N/P 15) reduced relative cell viability in a dose-dependent manner for both HEK293 and RAW264.7 cells (Fig. 2). When compared with blank microparticles in HEK293 cells (Fig. 1), it was apparent that loaded microparticles were less tolerated by HEK293 cells than blank microparticles according to the MTT assay.
Transgene Expression
Luciferase expression was used as a marker for successful gene transfection in both HEK293 and RAW264.7 cells. Changes in luciferase expression were noted as a function of the N/P ratio used for the unencapsulated nanoplexes to determine if the N/P ratio influenced transgene expression. Luciferase expression increased with increasing N/P ratios in both cell lines (Fig. 3). These increases occurred primarily from N/P 0 to N/P 10, whereupon luciferase expression tapered off. A statistically significant increase in luciferase expression compared with the control (N/P 0; pDNA only) was noted in HEK293 cells at N/P 20 (p < 0.001). In contrast, although RAW264.7 cells followed the same trend, there were no statistically significant differences in luciferase expression compared to the control (Fig. 3).
Luciferase expression in HEK293 (black bars) and RAW264.7 (gray bars) cells for free PEI:pDNA nanoplexes (i.e., no microparticle encapsulation) after 48 h of transfection. All reported values are the mean and standard deviation for n = 3. Statistical significance was calculated using ordinary two-way ANOVA, comparing each value to the control (N/P 0) data set
A broader range of N/P ratios were tested from N/P 0 to N/P 25 (HEK293) and N/P 0 to N/P 30 (RAW264.7) to elucidate changes in luciferase expression as a function of the N/P ratio. These data indicated that there was an increase in luciferase expression from N/P 0 to N/P 2 in HEK293 cells, and a tapering after N/P 5 (Figure S1). In RAW264.7 cells (Figure S2), luciferase expression increased from N/P 0 to N/P 4 and tapered after N/P 8.
Nanoplexes encapsulated in porous PLA or porous PLA-PEG microparticles were also effective at inducing luciferase expression in HEK293 (Fig. 4A) and RAW264.7 cells (Fig. 4B). Luciferase expression was measured every 48 h, for up to 144 h. For both PLA and PLA-PEG microparticles in HEK293 cells, luciferase expression significantly increased as a function of time from 96 to 144 h (p < 0.0001) (Table S2). In contrast, significant increases in luciferase expression were observed from 48 to 96 h (p < 0.01) in RAW264.7 cells for both types of microparticles as well as from 96 to 144 h in PLA microparticles (p < 0.0001) and PLA-PEG microparticles (p < 0.01). In HEK293 cells, the addition of PEG to the microparticles significantly increased luciferase expression (p < 0.0001). In contrast, in RAW264.7 cells, only one time point (96 h) showed significant differences.
Luciferase expression in HEK293 (a) and RAW264.7 (b) cells following transfection with PEI:pDNA loaded porous microparticles for both PLA (black bars) and PLA-PEG (white bars). Microparticles were added at a concentration of 3 mg/mL (1 μg DNA). All reported values are the mean and standard deviation for n = 3 trials. Statistical analysis was performed using a two-way ANOVA with comparisons between PLA and PLA-PEG at each time point. Significant differences are denoted by ****p < 0.00001 or n.s. for no significance
Differential Cell Counts Following Intra-tracheal Instillation
Particles were administered via intra-tracheal instillation to ensure deposition within the lung. The effects of altering the microparticle material (PLGA versus PLA-PEG), the porosity of particles (porous versus non-porous), and the size of porous particles (1 μm, 4 μm, 10 μm) on differential cell counts in the BAL fluid were assessed (Fig. 5).
Porosity influenced the cell counts for the PLA-PEG microparticles but did not for the PLGA microparticles. In particular, there were no differences between the numbers of macrophages, neutrophils, or total cells (Fig. 5) for 4 μm PLGA particles that were porous or non-porous. However, for 4 μm PLA-PEG particles, non-porous particles generally had lower cell counts, particularly in neutrophils and total cells (Fig. 5). Comparing porous particles of difference sizes revealed that exposure to 1 μm and 10 μm PLA-PEG microparticles resulted in the recruitment of similar numbers of macrophages (Fig. 5); however, 1 μm porous PLA-PEG recruited more neutrophils (Fig. 5) and total cells (Fig. 5) than the 10 μm particles. Furthermore, both 1 μm and 10 μm particles recruited more cells than the 4 μm particles. Thus, confirming that the particle size is an important factor in the immune response to particle administration in the lung.
DISCUSSION
Genetic material (DNA/RNA) does not easily cross the cell membrane because of charge repulsion (27). Generally, charge repulsion is overcome by complexing DNA or RNA with a positively charged polymer, such as PEI (28,29,30). Once complexed, there is a net positive charge that can facilitate cell binding and uptake and then escape from endosomal compartments through a mechanism known as the proton sponge effect (28,31,32). However, positively charged polymers kill many of the cells that get transfected above a certain N/P ratio (33,34). Microparticles may offer a protective barrier to cell death by prolonging the release profile of the positively charged material. Encapsulation into microparticles also protects the DNA from degradation and slows release (23,35,36).
The microparticles used within this study have been previously characterized (23). Successful polymerization of PLA and mPEG was confirmed using 1H NMR spectroscopy, and the size of all microparticles was determined using ImageJ and scanning electron microscopy (SEM). The SEM images also confirmed the presence of pores in the particles. Porosity was further confirmed through aerodynamic diameter measurements. An aerodynamic diameter of 1–5 μm, which was observed for these particles, is suitable for deposition in the airways (20). The encapsulation efficiency of the PEI-pDNA within the microparticles was quantified to be ~80–90% using UV absorbance, and the release of PEI-pDNA from the microparticles was determined over 340 h (2 weeks) with incubation at 37°C. The resultant cumulative release was ~90% (23).
HEK293 cells were used in this study because they proliferate rapidly and can be transfected more readily than other cell types (37). RAW264.7 murine macrophages are more difficult to transfect and serve as a model for pulmonary uptake and phagocytosis. The overall trends that were observed in the HEK293 cells and the RAW264.7 macrophages were similar. The relative cell viability of cells cultured with blank microparticles was investigated in only the HEK293 cells, because they were expected to have a more sensitive response than the RAW264.7 macrophages. Although there was a decrease in the relative cell viability at the lower time points, viability increased again by 30 h for low concentrations of the microparticles (Fig. 1). It was assumed that unencapsulated PEI-pDNA would induce stronger cytotoxic responses than the encapsulated microparticle formulations, consistent with prior studies (13,38). PEI is a cationic polymer, whereas PLGA is a negatively charged, hydrophilic polymer. Previous investigations have quantified the zeta potential of PLGA with and without cationic conjugation, which confirm that the microparticles alone are negatively charged, but the charge becomes positive once nanoplexes (or dendriplexes) are introduced (13,15,38). When nanoplexes were encapsulated into the microparticles, there was a decrease in relative cell viability that was concentration-dependent (Fig. 2). Complete monolayer coverage for these particles within the wells was calculated to occur at 12.5 mg/mL, thus suggesting that the observed differences in viability at high concentrations may have been cytotoxicity caused by a physical phenomenon (disruption of the cell membrane) rather than an intracellular cytotoxic response, such as apoptosis. PEI may induce cell death via apoptosis promoted by mitochondrial damage (39). Microparticles can lower the observed toxicity compared with free PEI-pDNA (15), which may also be a result of apoptosis (40). Therefore, it is possible that in these experiments, both apoptosis and necrosis were mechanisms of the observed decrease in cell viability.
We previously reported that ∼50% of the pDNA (0.5 μg) was released from PLA-PEG particles after 9 days (216 h) (23). In the present study, transgene expression was observed in both HEK293 and RAW264.7 cell lines after as little as 48 h (Fig. 4), which may be a result of surface nanoplexes from incomplete encapsulation and enhanced release rates caused by cell enzymes in vitro compared with the benchtop investigation. At the earliest time point of 48 h, this effect was not observable in RAW264.7 cells (Fig. 4B), likely because these cells are more difficult to transfect than HEK293 cells. The increased transgene expression at longer time points can be explained by the sustained release of the cargo (Fig. 4). With the additional knowledge that luminescence, and therefore the luciferase signal, decreases overtime, we would not expect such observations in the absence of continued release over the 6-day (144 h) period for nanoplexes encapsulated into microparticles which is consistent with the concept that nanoplexes were undergoing sustained release.
Differences in luciferase expression between PLA and PLA-PEG in HEK293 cells demonstrated that the addition of PEG increased release rates in accordance with previously reported data (23). There were likely two key effects of PEG in this study: 1) PEG recruits more water than the hydrophobic PLA, thus increasing the hydrolysis reaction necessary to break down PLA and speeding degradation (41), and 2) PEG alters protein affinity for the particle surface, resulting in lower availability (42). These properties of PEG may be responsible for the noted differences in luciferase expression upon PEGylation, particularly increased expression in both HEK293 and RAW264.7 cells in vitro (Fig. 4).
In the in vivo model, the effects of porosity and particle size were investigated to determine an optimal microparticle for limiting the inflammatory response in the lungs. Intra-tracheal instillation was chosen for microparticle delivery because it ensures that all particles are deposited directly into the lungs prior to systemic distribution (43,44). This reduces the likelihood that particles will be eliminated by the complex defense mechanisms associated with pulmonary delivery, and increases overall delivery efficiency (43,45,46). Furthermore, highly porous particles of large geometric diameter have favorable diameters to allow for deposition in the lung (23,47).
In the BAL collected from treated rats, differences were noted in the number of total cells and neutrophils (Fig. 5). In the inflammatory response, neutrophils are often the “first responders” to xenobiotics, and therefore their abundance 4 h after administration was expected (48). At later time points, it is likely that the inflammatory response would shift away from neutrophils towards macrophages. These macrophages release responsive cytokines and digest the foreign microparticles as part of the inflammatory response (49). Cellular recruitment may be a direct result of the release of PEI, as several groups have reported that PEI itself could elicit an immune response (50). However, PLGA microparticles have also been demonstrated to recruit immune cells in mice (16,24), and have been shown to be phagocytosed by antigen presenting cells (14).
The trends in cell counts indicate that particle porosity influences neutrophil recruitment for PLA-PEG, but not for PLGA particles (Fig. 5); however, these differences were not statistically significant. Porosity influences the aerodynamic diameter of particles, which is the effective diameter for aerosolized particles. Greater porosity results in lower density and corresponds to a smaller aerodynamic diameter, which effectively means that the particles behave as smaller than their true size during delivery (21,47,51). That said, the actual particle size and PEG density are still important for cellular uptake (42). Given the observed differences in neutrophil recruitment between porous 4 μm PLA-PEG microparticles and non-porous 4 μm PLA-PEG microparticles (Fig. 5), it is possible that fewer porous particles were delivered to the target site as they have a larger potential to reach deeper within than lung than their non-porous counterparts. Alternatively, the interaction of PEG with the lungs may limit the inflammatory response, in this case cellular recruitment (52). This may also explain why PEGylated particles have longer retention times and reduced clearance (25).
These observations further support the idea that microparticle diameter influenced neutrophil recruitment following particle administration. Neutrophils are often the “first-line” of defense in that they release the cytokines that signal for inflammation and other defensive responses in the lungs. Such changes in neutrophil recruitment indicated that the porous 4 μm PLA-PEG are the least inflammatory of the PEGylated particles investigated here.
Recently, the first mRNA-based vaccines were approved for emergency use in response to the SARS-CoV-2 global pandemic. At present, four countries have approved the vaccine, including the UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) (53), and the US Food and Drug Administration (FDA) (54), in addition to approval from Bahrain and Canada. This novel vaccine differs from the formulations presented in this study in two key ways: 1) mRNA and pDNA operate with different mechanisms (55), and 2) the recently approved vaccines use lipid carriers rather than synthetic polymers. Lipid-based particles may be formed from a diverse panel of organic compounds, with the primary component being amphiphilic phospholipids. These particles have been used for both DNA and RNA, with effective complexation via electrostatic interactions, similarly to how PEI-pDNA nanoplexes were formed. Furthermore, these particles protect the genetic material from degradation and increase the likelihood of cellular uptake, again, similar to PEI-pDNA nanoplexes. There was existing evidence that mRNA vaccines were promising, including success in cancers, infectious diseases, and viral diseases (56,57,58). The mRNA vaccines work by entering host cells where their cargo is translated into protein in the cytoplasm that is subsequently processed and presented in a form which can activate the immune system, specifically T cells (59). For pDNA vaccines, the plasmid DNA needs to enter the nucleus to produce the protein that will then elicit an immune response through antigen-presenting cells, such as dendritic cells (60). There remain no DNA vaccines approved for human use in the USA, but these have had success in veterinary medicine (61,62). As such, it is possible that these vaccines will be the next major milestone for human immunizations.
CONCLUSION
Gene delivery to the lungs can be achieved using polymeric microparticles, which protect genetic material from degradation. Additionally, these particles can be carefully designed such that they are suitable for deposition within the pulmonary region, allowing them to release their cargo directly to the target site over time. In this work, we showed that RAW264.7 murine macrophages, which are difficult to transfect, have transgene expression from 48 to 144 h albeit at much lower levels than HEK293 cells. Furthermore, using PEGylated particles in place of PLA particles enhances transfection with one likely cause being the accelerated degradation of the microparticles. Finally, intra-tracheal instillation of microparticles in rats revealed that 4 μm porous PEGylated microparticles recruited fewer neutrophils and macrophages than 1 μm or 10 μm porous PLA-PEG microparticles. For PLGA particles, porosity did not influence cell recruitment in the BAL fluid, but for PLA-PEG microparticles, non-porous microparticles yielded lower cellular recruitment than porous microparticles. These studies have demonstrated that polymeric microparticles encapsulating PEI:pDNA nanoplexes are suitable for transfecting cells in vitro, and that 4 μm, non-porous PLA-PEG microparticles recruited the lowest number of inflammatory cells in vivo. Further investigations are necessary to determine the ability of these microparticles to be delivered in a patient-compliant model, such as an aerosol inhaler. These results, combined with prior investigations, indicate that deposition in the deep lung is achievable for future delivery applications.
References
Breman JG, Arita I, Unit SE, Organization WH. The confirmation and maintenance of smallpox eradication. Geneva, Switzerland: World Health Organization; 1980.
Greene SA, Ahmed J, Datta SD, Burns CC, Quddus A, Vertefeuille JF, et al. Progress toward polio eradication - worldwide, January 2017-March 2019. MMWR Morb Mortal Wkly Rep. 2019;68(20):458–62. https://doi.org/10.15585/mmwr.mm6820a3.
Kumar A, Meldgaard TS, Bertholet S. Novel platforms for the development of a universal influenza vaccine. Front Immunol. 2018;9:600. https://doi.org/10.3389/fimmu.2018.00600.
Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–83. https://doi.org/10.1016/j.jhep.2018.12.001.
Saslow D, Castle PE, Cox JT, Davey DD, Einstein MH, Ferris DG, et al. American Cancer Society Guideline for human papillomavirus (HPV) vaccine use to prevent cervical cancer and its precursors. CA Cancer J Clin. 2007;57(1):7–28. https://doi.org/10.3322/canjclin.57.1.7.
Bryan JT. Developing an HPV vaccine to prevent cervical cancer and genital warts. Vaccine. 2007;25(16):3001–6. https://doi.org/10.1016/j.vaccine.2007.01.013.
Wolff JA, Malone RW, Williams P, Chong W, Acsadi G, Jani A, et al. Direct gene transfer into mouse muscle in vivo. Science. 1990;247(4949 Pt 1):1465–8. https://doi.org/10.1126/science.1690918.
Al-Dosari MS, Gao X. Nonviral gene delivery: principle, limitations, and recent progress. AAPS J. 2009;11(4):671–81. https://doi.org/10.1208/s12248-009-9143-y.
Wongrakpanich A, Morris AS, Geary SM, Joiner MA, Salem AK. Surface-modified particles loaded with CaMKII inhibitor protect cardiac cells against mitochondrial injury. Int J Pharm. 2017;520(1-2):275–83. https://doi.org/10.1016/j.ijpharm.2017.01.061.
Wafa EI, Geary SM, Goodman JT, Narasimhan B, Salem AK. The effect of polyanhydride chemistry in particle-based cancer vaccines on the magnitude of the anti-tumor immune response. Acta Biomater. 2017;50:417–27. https://doi.org/10.1016/j.actbio.2017.01.005.
Morris AS, Sebag SC, Paschke JD, Wongrakpanich A, Ebeid K, Anderson ME, et al. Cationic CaMKII inhibiting nanoparticles prevent allergic asthma. Mol Pharm. 2017;14(6):2166–75. https://doi.org/10.1021/acs.molpharmaceut.7b00114.
Ahmed KK, Geary SM, Salem AK. Surface engineering tumor cells with adjuvant-loaded particles for use as cancer vaccines. J Control Release. 2017;248:1–9. https://doi.org/10.1016/j.jconrel.2016.12.036.
Intra J, Salem AK. Fabrication, characterization and in vitro evaluation of poly(D,L-lactide-co-glycolide) microparticles loaded with polyamidoamine-plasmid DNA dendriplexes for applications in nonviral gene delivery. J Pharm Sci. 2010;99(1):368–84. https://doi.org/10.1002/jps.21840.
Abbas AO, Donovan MD, Salem AK. Formulating poly(lactide-co-glycolide) particles for plasmid DNA delivery. J Pharm Sci. 2008;97(7):2448–61. https://doi.org/10.1002/jps.21215.
Zhang XQ, Intra J, Salem AK. Conjugation of polyamidoamine dendrimers on biodegradable microparticles for nonviral gene delivery. Bioconjug Chem. 2007;18(6):2068–76. https://doi.org/10.1021/bc070116l.
Zhang XQ, Dahle CE, Baman NK, Rich N, Weiner GJ, Salem AK. Potent antigen-specific immune responses stimulated by codelivery of CpG ODN and antigens in degradable microparticles. J Immunother. 2007;30(5):469–78. https://doi.org/10.1097/CJI.0b013e31802fd8c6.
Intra J, Salem AK. Characterization of the transgene expression generated by branched and linear polyethylenimine-plasmid DNA nanoparticles in vitro and after intraperitoneal injection in vivo. J Control Release. 2008;130(2):129–38. https://doi.org/10.1016/j.jconrel.2008.04.014.
Kim N, Jiang D, Jacobi AM, Lennox KA, Rose SD, Behlke MA, et al. Synthesis and characterization of mannosylated pegylated polyethylenimine as a carrier for siRNA. Int J Pharm. 2012;427(1):123–33. https://doi.org/10.1016/j.ijpharm.2011.08.014.
Jiang D, Salem AK. Optimized dextran-polyethylenimine conjugates are efficient non-viral vectors with reduced cytotoxicity when used in serum containing environments. Int J Pharm. 2012;427(1):71–9. https://doi.org/10.1016/j.ijpharm.2011.10.032.
Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew ML, et al. Large porous particles for pulmonary drug delivery. Science. 1997;276(5320):1868–71. https://doi.org/10.1126/science.276.5320.1868.
Alipour S, Montaseri H, Tafaghodi M. Inhalable, large porous PLGA microparticles loaded with paclitaxel: preparation, in vitro and in vivo characterization. J Microencapsul. 2015;32(7):661–8. https://doi.org/10.3109/02652048.2014.944949.
Lassalle V, Ferreira ML. PLA nano- and microparticles for drug delivery: an overview of the methods of preparation. Macromol Biosci. 2007;7(6):767–83. https://doi.org/10.1002/mabi.200700022.
Terry TL, Givens BE, Rodgers VGJ, Salem AK. Tunable properties of Poly-DL-Lactide-monomethoxypolyethylene glycol porous microparticles for sustained release of polyethylenimine-DNA polyplexes. AAPS PharmSciTech. 2019;20(1):23. https://doi.org/10.1208/s12249-018-1215-9.
Joshi VB, Adamcakova-Dodd A, Jing X, Wongrakpanich A, Gibson-Corley KN, Thorne PS, et al. Development of a poly (lactic-co-glycolic acid) particle vaccine to protect against house dust mite induced allergy. AAPS J. 2014;16(5):975–85. https://doi.org/10.1208/s12248-014-9624-5.
Qie Y, Yuan H, von Roemeling CA, Chen Y, Liu X, Shih KD, et al. Surface modification of nanoparticles enables selective evasion of phagocytic clearance by distinct macrophage phenotypes. Sci Rep. 2016;6:26269. https://doi.org/10.1038/srep26269.
Liu Y, Hardie J, Zhang X, Rotello VM. Effects of engineered nanoparticles on the innate immune system. Semin Immunol. 2017;34:25–32. https://doi.org/10.1016/j.smim.2017.09.011.
Frohlich E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int J Nanomedicine. 2012;7:5577–91. https://doi.org/10.2147/IJN.S36111.
Khorsand B, Nicholson N, Do AV, Femino JE, Martin JA, Petersen E, et al. Regeneration of bone using nanoplex delivery of FGF-2 and BMP-2 genes in diaphyseal long bone radial defects in a diabetic rabbit model. J Control Release. 2017;248:53–9. https://doi.org/10.1016/j.jconrel.2017.01.008.
Atluri K, Seabold D, Hong L, Elangovan S, Salem AK. Nanoplex-mediated codelivery of fibroblast growth factor and bone morphogenetic protein genes promotes osteogenesis in human adipocyte-derived mesenchymal stem cells. Mol Pharm. 2015;12(8):3032–42. https://doi.org/10.1021/acs.molpharmaceut.5b00297.
Kasturi SP, Sachaphibulkij K, Roy K. Covalent conjugation of polyethyleneimine on biodegradable microparticles for delivery of plasmid DNA vaccines. Biomaterials. 2005;26(32):6375–85. https://doi.org/10.1016/j.biomaterials.2005.03.043.
Akinc A, Thomas M, Klibanov AM, Langer R. Exploring polyethylenimine-mediated DNA transfection and the proton sponge hypothesis. J Gene Med. 2005;7(5):657–63. https://doi.org/10.1002/jgm.696.
Benjaminsen RV, Mattebjerg MA, Henriksen JR, Moghimi SM, Andresen TL. The possible “proton sponge” effect of polyethylenimine (PEI) does not include change in lysosomal pH. Mol Ther. 2013;21(1):149–57.
Fischer D, Bieber T, Li Y, Elsasser HP, Kissel T. A novel non-viral vector for DNA delivery based on low molecular weight, branched polyethylenimine: effect of molecular weight on transfection efficiency and cytotoxicity. Pharm Res. 1999;16(8):1273–9. https://doi.org/10.1023/a:1014861900478.
Deng R, Yue Y, Jin F, Chen Y, Kung HF, Lin MC, et al. Revisit the complexation of PEI and DNA - how to make low cytotoxic and highly efficient PEI gene transfection non-viral vectors with a controllable chain length and structure? J Control Release. 2009;140(1):40–6. https://doi.org/10.1016/j.jconrel.2009.07.009.
Loira-Pastoriza C, Todoroff J, Vanbever R. Delivery strategies for sustained drug release in the lungs. Adv Drug Deliv Rev. 2014;75:81–91. https://doi.org/10.1016/j.addr.2014.05.017.
Rytting E, Nguyen J, Wang X, Kissel T. Biodegradable polymeric nanocarriers for pulmonary drug delivery. Expert Opin Drug Deliv. 2008;5(6):629–39. https://doi.org/10.1517/17425247.5.6.629.
Thomas P, Smart TG. HEK293 cell line: a vehicle for the expression of recombinant proteins. J Pharmacol Toxicol Methods. 2005;51(3):187–200. https://doi.org/10.1016/j.vascn.2004.08.014.
Zhang XQ, Intra J, Salem AK. Comparative study of poly (lactic-co-glycolic acid)-poly ethyleneimine-plasmid DNA microparticles prepared using double emulsion methods. J Microencapsul. 2008;25(1):1–12. https://doi.org/10.1080/02652040701659347.
Paul A, Eun C-J, Song JM. Cytotoxicity mechanism of non-viral carriers polyethylenimine and poly-l-lysine using real time high-content cellular assay. Polymer. 2014;55(20):5178–88. https://doi.org/10.1016/j.polymer.2014.08.043.
Shi X, Li C, Gao S, Zhang L, Han H, Zhang J, et al. Combination of doxorubicin-based chemotherapy and polyethylenimine/p53 gene therapy for the treatment of lung cancer using porous PLGA microparticles. Colloids Surf B: Biointerfaces. 2014;122:498–504. https://doi.org/10.1016/j.colsurfb.2014.07.020.
Andhariya JV, Shen J, Choi S, Wang Y, Zou Y, Burgess DJ. Development of in vitro-in vivo correlation of parenteral naltrexone loaded polymeric microspheres. J Control Release. 2017;255:27–35. https://doi.org/10.1016/j.jconrel.2017.03.396.
Walkey CD, Olsen JB, Guo H, Emili A, Chan WC. Nanoparticle size and surface chemistry determine serum protein adsorption and macrophage uptake. J Am Chem Soc. 2012;134(4):2139–47. https://doi.org/10.1021/ja2084338.
Kleemann E, Jekel N, Dailey LA, Roesler S, Fink L, Weissmann N, et al. Enhanced gene expression and reduced toxicity in mice using polyplexes of low-molecular-weight poly(ethylene imine) for pulmonary gene delivery. J Drug Target. 2009;17(8):638–51. https://doi.org/10.1080/10611860903106414.
Hara K, Tsujimoto H, Tsukada Y, Huang CC, Kawashima Y, Tsutsumi M. Histological examination of PLGA nanospheres for intratracheal drug administration. Int J Pharm. 2008;356(1-2):267–73. https://doi.org/10.1016/j.ijpharm.2007.12.041.
Vila A, Gill H, McCallion O, Alonso MJ. Transport of PLA-PEG particles across the nasal mucosa: effect of particle size and PEG coating density. J Control Release. 2004;98(2):231–44. https://doi.org/10.1016/j.jconrel.2004.04.026.
Blank F, Fytianos K, Seydoux E, Rodriguez-Lorenzo L, Petri-Fink A, von Garnier C, et al. Interaction of biomedical nanoparticles with the pulmonary immune system. J Nanobiotechnology. 2017;15(1):6. https://doi.org/10.1186/s12951-016-0242-5.
Yang Y, Bajaj N, Xu P, Ohn K, Tsifansky MD, Yeo Y. Development of highly porous large PLGA microparticles for pulmonary drug delivery. Biomaterials. 2009;30(10):1947–53. https://doi.org/10.1016/j.biomaterials.2008.12.044.
Rosales C. Neutrophil: a cell with many roles in inflammation or several cell types? Front Physiol. 2018;9:113. https://doi.org/10.3389/fphys.2018.00113.
Geissmann F, Manz MG, Jung S, Sieweke MH, Merad M, Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327(5966):656–61. https://doi.org/10.1126/science.1178331.
Sheppard NC, Brinckmann SA, Gartlan KH, Puthia M, Svanborg C, Krashias G, et al. Polyethyleneimine is a potent systemic adjuvant for glycoprotein antigens. Int Immunol. 2014;26(10):531–8. https://doi.org/10.1093/intimm/dxu055.
Musante CJ, Schroeter JD, Rosati JA, Crowder TM, Hickey AJ, Martonen TB. Factors affecting the deposition of inhaled porous drug particles. J Pharm Sci. 2002;91(7):1590–600. https://doi.org/10.1002/jps.10152.
Suk JS, Xu Q, Kim N, Hanes J, Ensign LM. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev. 2016;99(Pt A):28–51. https://doi.org/10.1016/j.addr.2015.09.012.
Mahase E. Covid-19: UK approves Pfizer and BioNTech vaccine with rollout due to start next week. BMJ. 2020;371:m4714. https://doi.org/10.1136/bmj.m4714.
Tanne JH. Covid-19: FDA panel votes to approve Pfizer BioNTech vaccine. BMJ. 2020;371:m4799. https://doi.org/10.1136/bmj.m4799.
Givens BE, Naguib YW, Geary SM, Devor EJ, Salem AK. Nanoparticle-based delivery of CRISPR/Cas9 genome-editing therapeutics. AAPS J. 2018;20(6):108. https://doi.org/10.1208/s12248-018-0267-9.
Alameh M-G, Weissman D, Pardi N. Messenger RNA-based vaccines against infectious diseases. Berlin, Heidelberg: Springer Berlin Heidelberg. p. 1-35.
Jackson NAC, Kester KE, Casimiro D, Gurunathan S, DeRosa F. The promise of mRNA vaccines: a biotech and industrial perspective. NPJ Vaccines. 2020;5:11. https://doi.org/10.1038/s41541-020-0159-8.
Mascola JR, Fauci AS. Novel vaccine technologies for the 21st century. Nat Rev Immunol. 2020;20(2):87–8. https://doi.org/10.1038/s41577-019-0243-3.
Zhang NN, Li XF, Deng YQ, Zhao H, Huang YJ, Yang G, et al. A Thermostable mRNA vaccine against COVID-19. Cell. 2020;182(5):1271–83 e16. https://doi.org/10.1016/j.cell.2020.07.024.
Tejeda-Mansir A, Garcia-Rendon A, Guerrero-German P. Plasmid-DNA lipid and polymeric nanovaccines: a new strategic in vaccines development. Biotechnol Genet Eng Rev. 2019;35(1):46–68. https://doi.org/10.1080/02648725.2018.1560552.
Ingolotti M, Kawalekar O, Shedlock DJ, Muthumani K, Weiner DB. DNA vaccines for targeting bacterial infections. Expert Rev Vaccines. 2010;9(7):747–63. https://doi.org/10.1586/erv.10.57.
Fruk L, Franck CO, Fanslau L, Popov AB, Tyagi P. Biopolymer-based carriers for DNA vaccine design. Angew Chem Int Ed Eng. 2020. https://doi.org/10.1002/anie.202010282.
Acknowledgements
Histology was performed in the Central Microscopy Research Facility (CMRF) at the University of Iowa. In vivo studies were conducted in laboratory facilities supported by the Environmental Health Sciences Research Center funded by NIH P30 ES005605.
Funding
A.K.S acknowledges support from the NIH P30 CA086862 grant and the Lyle and Sharon Bighley Chair of Pharmaceutical Sciences. T.L.T. acknowledges support from the Department of Education GAANN Fellowship program. B.E.G. acknowledges funding support from the Alfred P. Sloan Foundation, the University of Iowa Graduate College, and the National GEM Consortium. V. G. J. R. acknowledges support from the Jacques S. Yeager, Sr. endowment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editors: Xiuling Lu and Aliasger K Salem
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Terry, T.L., Givens, B.E., Adamcakova-Dodd, A. et al. Encapsulating Polyethyleneimine-DNA Nanoplexes into PEGylated Biodegradable Microparticles Increases Transgene Expression In Vitro and Reduces Inflammatory Responses In Vivo. AAPS PharmSciTech 22, 69 (2021). https://doi.org/10.1208/s12249-021-01932-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-01932-z