Abstract
The aim of this study was to determine amphotericin B (AmB) permeation across lipid bilayer membranes mounted on Transwell® and to observe the phagocytosis of the AmB and the AmB-lipid formulations by alveolar macrophage (AM) cell lines using a fluorescence microscope. The lipid bilayer membranes were prepared from phospholipid and ergosterol as well as phospholipid and cholesterol in a ratio (67:33 mol%). AmB-lipid formulations were prepared from AmB incorporated with four lipid derivatives during a lyophilization process. In vitro cytotoxicity studies were carried out on kidney cells by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. The levels of nitric oxide production by AMs exposed to these AmB-lipid formulations were determined by the Griess reaction. Phagocytosis of the AmB-lipid formulations was carried out using AM cells. The lipid bilayer membranes and AmB-lipid formulations were successfully prepared. In vitro cytotoxicity results showed less toxicity to kidney cells than pure AmB, and a 1,000-fold less production of nitric oxide by NR8383 cell lines was obtained when compared to lipopolysaccharide. Permeation results were two- to fivefold higher than for pure AmB in the ergosterol containing lipid bilayer and two- to fourfold higher than AmB in the cholesterol containing compositions, both of which were enough to kill the fungi according to their MICs and MFCs. AM phagocytosed the AmB-lipid formulations. We suggest that these products especially the AmB-sodium deoxycholate sulfate are potential candidates for targeting AM cells for the treatment of invasive pulmonary aspergillosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
During the last few decades, the incidence of pulmonary fungal infections has increased significantly due to the growing number of immune-compromised patients mostly those infected with human immunodeficiency virus (HIV), or have undergone organ transplantations, or suffer from hematologic disorders and cancer (1). Aspergillus species are ubiquitous, and their spores are inevitably inhaled into the airways. The inhalation of aspergillus spores, followed by failure inhibition of the resident macrophage and neutrophils, is the first step of infection. There are many anti-fungal drugs commercially available such as voriconazole, fluconazole, itraconazole, caspofungin, and amphotericin B (AmB) (1). Among these, AmB is a drug of choice to treat cryptococcosis, histoplasmosis, and aspergillosis. However, the nephrotoxicity of AmB is a major clinical problem that can often lead to discontinuation of treatment (2). Ergosterol on the fungal cell membrane is the binding target of AmB. AmB disrupts the cell membrane structure by creating channels or pores. This causes the sodium, potassium, and hydrogen ion leakage from the fungal cells followed by cell death (3,4).
The alveolar macrophages (AMs) are the target cells for AmB as they are the first line of defense against microbial invasion as they engulf and sequester the pathogens and hopefully destroy them (5). The AmB can facilitate this process. The AMs are a type of phagocytotic leukocytes that are found in small airways of the lungs. Nitric oxide (NO), one of their inhibitory excretions, is a free radical that is produced by various cells in the lungs. NO is produced by the enzyme iNOS that plays an important role in defense against airborne pathogens or in tissue damage associated with inflammatory processes in the lungs (6). AMs are active producers of cytokines and leukotrienes and have important pro-inflammatory roles in the alveolus. The delivery systems that directly target the drugs to the AM are therefore an attractive approach for delivering drugs to the lungs of immunocompromised patients with fungal infections. This provides rapid access of the drug to the infected AM, to quickly combat microbial infections (7).
Lipid bilayer membrane is a fundamental and vital part of cells. It controls the molecular transport across cellular boundary. Therefore, lipid bilayer membranes are key aspects of drug research in relation to (i) the interactions of drugs with membrane receptors and (ii) permeation of cell membranes (8) The different types of lipids that constitute the lipid membrane as well as the external thermodynamic conditions such as temperature, pH, degree of hydration, and ionic strength are all major determinants of the behavior of the macroscopic phase and their associated physical properties. The temperature, acyl chain length, cholesterol content, and the drug properties are some of the parameters that can affect lipid bilayer permeability. During our study, all relevant parameters were kept constant, as much as possible, such as temperature with all experiments were carried out at room temperature, and the acyl chain length of lipid bilayer membrane formations was the same for all experiments (phospholipid and ergosterol/cholesterol concentration was constant at 67:33 mol%), and the pure drug AmB or AmB-lipid formulation concentration was also fixed at 50 μg of AmB in 5 mL phosphate buffer solution (pH 7.4). In this work, different lipid drug carriers were used to formulate the AmB-lipid dry power formulations in the mole ratio of 1:2. We determined the relationships between the drug and the different lipid drug carrier formulations through permeability studies in a lipid bilayer membrane.
In order to enhance AmB effectiveness and reduce toxicity, different lipid derivative carriers such as sodium deoxycholate sulfate (SDCS) and potassium deoxycholate (KDC) were also introduced. Two other lipids, sodium deoxycholate (SDC) and sodium cholate (SC), were chosen for use as lipid carriers. SDC was used as a control. In the present work, we hypothesized that some of these AmB-lipid derivative formulations could improve drug safety, enhance the drug permeability through lipid bilayer membranes, and target the AM. The recent research also indicated that liposome-based AmB formulation could lead to a lysosomal storage disease. The AmB-liposome accumulation in reticulo-endothelial system and phagocytotic cells can occur. It may rapidly release large amount of free AmB and lead to toxicity problem (9).
The safety of the administered AmB-lipid formulations in the airways was also determined to ensure that they did not induce nitric oxide in the airways at toxic levels and caused no toxicity to kidney cell lines. The targeting of the AM was carried out by demonstrating the phagocytosis of nanoparticles using the fluorescence microscope.
MATERIALS AND METHOD
Materials
AmB was obtained from Ambalal Sharabhai Enterprises Pvt. Ltd., Vadodara, India. Deoxycholic acid, cholic acid, sodium cholate, sodium deoxycholate, and ergosterol were from Sigma-Aldrich, St. Louis, USA. Sodium dihydrogen phosphate dihydrate and disodium hydrogen phosphate dihydrate were from Ajax Finechem Pty Ltd, NSW, Australia. Dimethylsulfoxide (DMSO) was from Riedel-de Haëan, Seelze, Germany. Polyamide membranes with a pore size of 0.22 μm were from Sartorius, Gottingen, Germany. All chemicals were used as received without further purification.
Preparation of Dry Powder AmB-Lipid Formulations (AmB-KDC, AmB-SDC, AmB-SDCS, and AmB-SC)
A mixture of AmB (250 mg) and KDC (220 mg) in a 1:2 (mol ratio) was prepared in distilled water (30 mL) and stirred for a few minutes. Potassium hydroxide solution (2.7 mL, 0.2 M) was then added slowly dropwise, at room temperature to obtain a clear yellowish-colored solution. The pH of the solution was adjusted by adding phosphoric acid (0.2 M) to obtain a pH of 7.4 for an in situ phosphate buffer. The final volume of the solution was adjusted to 50 mL by adding distilled water. The solution was lyophilized in a freeze dryer (Dura-Dry™ MP, FTS Systems Inc., NY, USA), and a caked yellowish dry powder was obtained. A similar methodology to that used for deoxycholic acid, and AmB was employed to prepare the sodium deoxycholate (AmB-SDC), sodium deoxycholate sulfate (AmB-SDCS), potassium deoxycholate (AmB-KDC), and sodium cholate (AmB-SC) formulations.
1H-NMR Spectroscopy
The 1H-NMR spectra of AmB, SDC, and AmB-SDC were measured on a Varian Unity Inova 500 MHz NMR spectrometer (Varian, Inc., CA, USA) using DMSO as solvent and tetramethylsilane (TMS) as internal standard.
The Cytotoxicity Assay on Kidney Cells
The cytotoxicity of AmB was studied by an in vitro test using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. Kidney cells (293T/17) were distributed in 96-well plates at a density of 1 × 105 cells/well in 100 μL complete medium and allowed to attach overnight. After 24 h at 37°C and an atmosphere of 5% CO2 and 95% humidity, the medium (100 μL) was replaced with medium containing various concentrations of the drug formulations or an equivalent concentration of AmB (1 to 8 μg/mL). After incubation for 24 h, 50 μL of a solution of MTT at 1.25 mg/mL (Invitrogen, USA) was added and incubated for a further 4 h at 37°C in a similar atmosphere and covered with an aluminum foil. The solutions were then removed from the 96-well plates, and 100 μL of DMSO was added to dissolve the formazan crystals. The optical densities (OD) were measured at 570 nm using a microplate reader (Biohit BP 800, Helsinki, Finland). Control cells were incubated with the medium without the AmB. Four wells were used for each concentration and time point. The percentage of surviving cells was calculated from the following formula: (ODtreated / ODcontrol) × 100. Three independent experiments were done. The number of viable cells in the treated well was compared to those in the untreated well and estimated as a percentage viability.
Determination of Nitric Oxide Released from an Alveolar Macrophage Response to AmB-Lipid Formulations
AM NR8383 cells were added to 96-well plates at an optical cell density of 1 × 105 cells/well, and after 24 h, the supernatant was collected and placed in a separate 96-well plate for detection of nitric oxide. This test was carried out with the AmB-lipid formulations (AmB-SDCS, AmB-SDC, AmB-KDC, and AmB-SC) and pure AmB. Lipopolysaccharide (LPS), a known NO activator, was used as a positive control. The NO released by NR8383 cells after being challenged with either AmB or the reconstituted AmB-lipid formulated dry powders in the concentration ranges of 1–32 μg/mL or 15–1,000 ng/mL for LPS. The NO production was detected by the Griess test. This measurement relied on the diazotization reaction of the Griess reagent and NO that developed pink color. The Griess reagent was prepared by mixing 1% sulfanilamide, 0.1% N-(1-naphthyl)-ethylenediamine dihydrochloride, and 2.5% phosphoric acid in water. Equal volumes of cell supernatant (100 μL) and Griess reagent (100 μL) were mixed. After 10 min, the absorbance was measured using a microplate reader (Biohit BP 800, Helsinki, Finland) at 450 nm. The NO concentration was calculated from a sodium nitrite standard curve (10,11).
Determination of AmB Permeation Across a Lipid Bilayer
Preparation of the Lipid Bilayer Membrane
Lipid bilayers were prepared by dissolving l-α-phosphatidylcholine 67 mol% and ergosterol 33 mol% in 30 mL of chloroform in a 100-mL round-bottomed flask suitable for uniform mixing (12). The solvent was removed under reduced pressure using a rotary evaporator (Eyela, Tokyo Rikakikai Co. Ltd., Tokyo, Japan) at 55°C until it formed a dried cake. The dried cake was transferred to a petri dish and further heated at 40°C for 48 h on a hotplate to completely remove the solvent, and a dry powder mixture was obtained. The dried powder was transferred into a vial with 6 mL of distilled water and kept in a water bath (50°C) for 1 h for hydration. The hydrated suspension (1,000 μL) was loaded onto each Transwell® (Corning Inc., NY, USA) and dried at 40°C for 48 h (Fig. 1). The dried lipid membrane on the Transwell® was prepared in an Ussing chamber system (Insert for 2300 Easy Mount Diffusion Chambers, Physiologic Instruments, Harvard Apparatus Companies, CT, USA).
Formation of Lipid Bilayer Membrane in the Ussing Chamber
The lipid bilayer Transwell® was fitted into the Ussing chamber. Phosphate buffer solution (10 mM, pH 7.4) 5 mL was added to both chambers and left for 1 h to completely hydrate and stabilize the membrane on the Transwell®.
Ussing Chambers Permeation Across Lipid Bilayer Model
The Ussing chamber is suitable for our experimental design in both shape and size, with a charge induced by formulations of the AmB-lipid in a solution form. Its basic principle was applied to measure the short-circuit current as an indicator of the net ion transport taking place across the lipid bilayer membrane (from the left to the right chamber). In the Ussing chamber, electrodes were placed on both sides of the lipid bilayer membrane to record the potential differences (PD) across the lipid bilayer. A set of two other electrodes allowed for the injection of a current (short-circuit current or Isc) to nullify the PD. The intensity of the current to be injected was monitored by an electric clamp apparatus. The Ussing chamber system was filled with the experimental phosphate buffer (10 mM, pH 7.4) 5 mL in both chambers, and the experiment was performed at room temperature (37°C). Some modifications were made to this instrument to perform our study. Instead of a biological membrane, we applied a preformed lipid bilayer membrane in the Transwell® to act as the membrane that was tested for AmB permeability or AmB-lipid formulations (13).
Collection of Samples from the Ussing Chamber
Before addition of the AmB suspension into the Ussing chamber system, first, we confirmed that there was no leakage from the chambers after grease had been applied to the two half chambers, when the electrodes were inserted into the Transwell® holes to assist with making them airtight and leak proof. After confirming this, we started the test for permeability. First of all, 50 μL of the drug solution or the AmB-lipid formulations (equivalent to AmB 1,000 μg/mL) was added to the left chamber and the initial current was recorded, and then after every 15 min, the current was recorded and 1 mL of sample was withdrawn from the right chamber, and the reduced volume was compensated with 1 mL of phosphate buffer solution in the right chamber until the 2-h period for collecting samples was completed. All experiments were performed at 37°C and in triplicate. The collected sample solutions were quantified for AmB by the high-performance liquid chromatography (HPLC) method to determine the percentage cumulative AmB permeation from the left chamber to right chamber. The drug contents assay was carried out using a standard HPLC method (Waters, Singapore). For the HPLC conditions, acetate buffer (20 mM, pH at 7.2) and acetonitrile (60:40 v/v) at a flow rate of 1 mL/min were used as the mobile phase. The microbondapak C18 column (Phenomenex®, USA) (150 × 4.6 mm i.d., 5 μm) was the stationary phase. UV detection was at a wavelength of 405 nm.
Phagocytosis of the Reconstituted AmB-Lipid Formulations by Macrophage Cells
The AmB-lipid dry powder formulations (AmB-SDCS) were reconstituted with distilled water to obtain 1 mg/mL of AmB. Quantum dot nanoparticles were employed for particle imaging. Lumidot® 640 (20 μg/mL) (Lumidot®, Sigma-Aldrich, St. Louis, USA) was added to the reconstituted AmB-SDCS in a volume ratio 1:2. The mixture was sonicated for 5 min, and reconstitution was observed with a fluorescence microscope. One hundred microliters of NR8383 cells (104 cells/mL) was cultured in each well of a 96-well plate and allowed to grow and adhere overnight at 37°C, in a 5% CO2 and 95% humidity incubator. The AmB-lipid reconstituted dry powder formulation AmB-SDCS stained with Lumidot® 640 (50 μL) was added to 104 cells/mL of the AM. Phagocytosis of anti-fungal nanoparticulate by AM NR8383 cells was observed with a fluorescence microscope (Olympus, BX61, Olympus, Tokyo, Japan).
Statistical Analysis
The data were compared using Student’s t test for independent samples. All statistical comparisons were calculated using the SPSS software version 16.09 (SPSS Inc., Chicago, IL). A significant of level of p value < 0.05 was considered statistically significant.
RESULTS AND DISCUSSION
Molecular Interaction of AmB and SDCS
The interaction between AmB and SDCS was mainly by inter-molecular hydrogen bonding that was clearly indicated by the 1H-NMR data (Fig. 2). The hydrogen bondings occurred at the 9 and 15 hydroxyls of AmB and the 3- and 12-hydroxyls of SDCS. The chemical shifts of the hydroxyl protons at C9 and C15 of AmB shifted from 3.47 to 3.51 ppm and from 3.95 to 3.78 ppm, respectively. The AmB-AmB interaction could be by either hydrogen bonding or hydrophobic interactions. The overall molecular interaction leads to the formation of micelles.
The Safety of AmB-Lipid Formulations to Kidney Cells
The toxicity of the AmB-lipid formulations (AmB-SDC, AmB-SDCS, AmB-KDC, and AmB-SC) on kidney cells was estimated at different AmB concentrations from 1 to 8 μg/mL by the MTT reduction assay after 24 h of exposure (Fig. 3). The incidence of nephrotoxicity of conventional AmB deoxycholate has been reported to be 49–65% (14). This toxicity test was carried out in vitro on human kidney cells (293T/17) (Fig. 3). The percentage viability of kidney cells was over 90% after challenging with AmB or AmB-lipid formulations at 1 μg/mL. A slight decrease of viability to around 83% at 2 μg/mL AmB was observed. However, at 4 and 8 μg/mL of pure AmB, a dramatic cell death was observed. The AmB-lipid formulations (AmB-SDC, AmB-SDCS, AmB-SC, and AmB-KDC) provided some protection of the kidney cells to AmB. Viability after treatment with 4 μg/mL was higher than 80% except for AmB-SDC. For the AmB-SDCS, AmB-SC, and AmB-KDC formulations, viability was higher than 80% at 8 μg/mL, and the AmB-SDC at these concentrations was slightly less toxic than pure AmB (Table I). Unlike the lipid bilayers, these micelles were not rigid vesicles. The AmB-micelles were in a dynamic equilibrium between the free AmB and the micellized AmB. The more stable micelles lead to lower levels of free AmB. Thus, the release of AmB from micelles may be faster than from the AmBisome® or the AmB entrapped in lipid vesicles (15,16). However, there was an interaction between the AmB and the lipids that could retard the release of AmB (17). In this case, it was possible that AmB-SDCS, AmB-SC, and AmB-KDC lipid formulations can form more stable micelles than AmB-SDC and reduced the free AmB. Spectrofluorometry was performed to determine the bound/free AmB in the AmB-SDCS system. The fluorescence intensity ratio between the different excitation and emission wavelengths represents the relative amount of free AmB in that system (18). The ratio of the AmB-associated micelle to the monomeric free AmB of the AmB-SDCS in isotonic dextrose solution was shown to be 14:1. In contrast, the ratio of the self-associated AmB to the monomeric free AmB of the pure AmB in isotonic dextrose solution was about 5:1 (Table II). This observation was also seen using the dimethylformamide solvent. It indicated that the more stable micelle system decreased the release of free AmB and formation of soluble aggregates occurred. Therefore, the AmB-SDCS resulted in a lower toxicity as a similar observation in the AmB nanomicelle formulation (19). These lipid formulations certainly seem to be less toxic than pure AmB. In the overall toxicity studies of the AmB-lipid formulations with the kidney cell lines (293T/17), no toxicity was observed up to 8 μg/mL of AmB.
Nitric Oxide Release from the Alveolar Macrophage Response to AmB-Lipid Formulations
The NO is an inflammatory indicator (20). Observing the NO released release from AM could indicate the toxicity of the AmB-lipid formulation. The NO released from the AM exposed to the AmB-lipid formulations was much lower than that with LPS (Fig. 4). The AM NR8383 cells were stimulated by LPS to produce a 1,000-fold greater amount of NO than any of the concentration of the AmB-lipid formulations (1–32 μg/mL of AmB). Davidson et al. reported that the safety level of NO was less than 80 μM (21), while NO release of all formulation at the concentration of 32 μg/ml AmB-equivalence did not exceed 25 μM (Table II). It was indicated that the AmB-lipid formulations at concentrations of AmB 1–32 μg/mL did not trigger the harmful NO release from the AM cell lines. This evidence implied that the AmB-lipid formulation was safe for inhalation delivery.
Permeation of AmB and AmB-Lipid Formulations Across Lipid Bilayer
The percentage of the cumulative AmB that was transferred from the left chamber to right chamber in a 2-h period is shown in Fig. 5. In the AmB-lipid formulations (AmB-SDCS, AmB-SDC, AmB-SC, and AmB-KDC), the cumulative drug transferred from the left to the right chamber was 10.6%, 4.3%, 3.6%, and 5.6%, respectively, whereas AmB itself only was cumulatively transferred by only 2.0%. During the permeability study period, we measured the current. At the initial period (before addition of sample), it was 0.6 μA. After an addition of 50 μL AmB suspension into the left chamber, the current was increased to 1.1 μA at 15 min. At every 15-min interval, current was gradually increased with time and reached 1.9 μA at the end of sampling time period (2 h). In a similar way, the current of the AmB-lipid formulations was 0.3–1.5 μA. This indicated that AmB and AmB-lipid formulations had permeated across the lipid bilayer membrane from the left chamber to the right chamber due to the driving force current. AmB was insoluble in water and produced an aggregated suspension. Only AmB-soluble monomer form or the AmB-lipid derivative soluble forms were able to permeate across the membrane. Also, the AmB-lipid formulations have counter ions that interacted with the lipid bilayer and facilitated the permeation of AmB. In the case of AmB, there were no charges available to counteract the lipid bilayer membrane. AmB itself may form a complex with the lipid bilayer resulting in a low permeability. This suggestion has been supported by the work of Herec (22), who proposed that hydrogen bonding between the horizontally oriented AmB and the polar groups of the lipids made the membrane more compact and less permeable to ions. AmB-SDCS had the highest zeta potential (−45 mV) (23) and produced the highest permeability (10.6%). This was due to the replacement of a carbonyl group of the deoxycholic acid ring with the sulfate group, which developed a highly negative charge. This sulfate group has a vital role as it can interact with the lipid bilayer to facilitate the penetration of more AmB. A similar phenomenon also occurred with the other formulations. These negatively charged ions facilitated a two- to fivefold greater transfer of AmB from the formulations to cross the lipid bilayer as compared with pure AmB (Table II). The proposed process of AmB permeation was shown in Fig. 6. Although only a small amount of AmB was transferred from the left to the right chamber, it was postulated that this amount was enough to kill the fungi because the AmB-lipid formulations released available AmB to achieve the MIC (about 13.2 μg/ml against Aspergillus spp.) (24). It is possible that the AmB and lipid bilayer might form a complex channel with the lipid bilayer and therefore reduce the amount of AmB available for permeation.
Phagocytosis of Anti-fungal Reconstituted Dry Powder Particles by Macrophage Cells
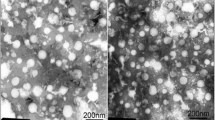
The AmB-SDCS formulation was reconstituted in distilled water and stained with Lumidot® 640. Photographs were taken in both the bright field and fluorescence mode as shown in Fig. 7a, b, respectively. For our AmB-lipid formulations (AmB-SDC, AmB-SDCS, AmB-KDC, and AmB-SC), particle sizes were 23 ± 1.4, 73 ± 0.9, 21 ± 2.7, and 31 ± 2.2 nm, respectively. The AmB-SDCS dispersed in liquid, and it had a round shape with a narrow size distribution in the bright field. The uniform nanoparticles produced a high intensity of light with stable images in the fluorescence mode.
Phagocytosis of NR 8383 cells incubated with reconstituted dry powder AmB-lipid formulation (AmB-SDCS) stained with Lumidot®640. a, b AmB-SDCS with Lumidot®640 in 2 min in bright field and fluorescence mode, respectively. c, d NR8383 cells with AmB-SDCS containing Lumidot®640 in 2 min in bright field and fluorescence mode, respectively (bar = 100 μm)
AM NR8383 cells were bright green when the cell photographs were taken in the bright field mode. To observe the phagocytosis, the AmB-SDCS formulation containing Lumidot® 640 was added to AM NR8383 cells. Photographs that were taken within 2 min in the bright field, and fluorescence mode showed that AM NR8383 cells had achieved phagocytosis (Fig. 7c, d), respectively. In the fluorescence mode, the intensity of the color was glowing and visible and produced very clear pictures to show that the AmB-SDCS had entered the cells. It indicated that AM NR8383 could phagocytose the particles stained with Lumidot® 640. These results were correlated with the size measurement after the reconstitution study. Kanchan and Panda reported that nanoparticles of 200–600 nm were efficiently phagocytosed and, in our case, nanoparticle sizes of <100 nm were efficiently phagocytosed (25). A similar result was reported by Rojanarat et al. (26). These results supported the view that AmB-SDCS lipid formulation was phagocytosed by AM NR8383 cells.
CONCLUSIONS
Lipid bilayer membranes that were successfully prepared and mounted in an Ussing chamber Transwell®, acted as semipermeable membranes. The in vitro permeability study of the AmB-lipid formulations was carried out using Ussing chamber that these formulations were two- to fivefold more permeable than pure AmB. A similar observation was that lipid membranes prepared from phospholipid and cholesterol (67:33 mol%) were two- to fourfold more permeable for AmB present in the formulations than pure AmB. Here, although two different lipid membrane compositions were observed, AmB-SDCS had the highest permeability in both cases. An in vitro kidney cell toxicity study showed that they were less toxic than free AmB. They were also successfully phagocyted by AM. Therefore, we concluded that they were suitable for the treatment of pulmonary aspergillosis by targeting AM. Among the four AmB-lipid formulations, SDS-lipid formulation was less toxic and had a higher permeability in comparison with the other three formulations.
REFERENCES
Limper AH, Knox KS, Sarosi GA, Ampel NM, Bennett JE, Catanzaro A, et al. An official American Thoracic Society statement: treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med. 2011;183:96–128.
Laniado-Laborín R, Cabrales-Vargas MN. Amphotericin B: side effects and toxicity. Rev Iberoam Micol. 2009;26:223–7.
Kirchgessner M. Amphotericin B. J Exot Pet Med. 2008;17:54–6.
Moen MD, Lyseng-Williamson KA, Scott LJ. Liposomal amphotericin B: a review of its use as empirical therapy in febrile neutropenia and in the treatment of invasive fungal infections. Drugs. 2009;69:361–92.
Andrade F, Rafel D, Videira M, Ferreira D, Sosnik A, Sarmento B. Nanotechnology and pulmonary delivery to overcome resistance in infectious diseases. Adv Drug Deliv Rev. 2013;65:1816–27.
Ialenti A, Ianaro A, Moncada S, Di Rosa M. Modulation of acute inflammation by endogenous nitric oxide. Eur J Pharmacol. 1992;211:177–82.
Vyas SP, Quraishi S, Gupta S, Jaganathan KS. Aerosolized liposome-based delivery of amphotericin B to alveolar macrophages. Int J Pharm. 2005;296:12–25.
Mouritsen OG, JØrgensen K. A new look at lipid-membrane structure in relation to drug research. Pharm Res. 1998;15:1507–19.
Michot JM, Gabuwa C, Fourn E, Maigne G, Teicher E, Angoulvant A, et al. Very prolonged liposomal amphotericin B use leading to a lysosomalstorage disease. Int J Antimicrob Agents. 2014;43:566–9.
Huttunen K, Ruotsalainen M, Iivanainen E, Torkko P, Katila ML, Hirvonen MR. Inflammatory responses in RAW 264.7 macrophages caused by mycobacteria isolated from moldy houses. Environ Toxicol Pharmacol. 2000;8:237–44.
Punturee K, Wild CP, Vinitketkumneun U. Thai medicinal plants modulate nitric oxide and tumor necrosis factor in J774.2 mouse macrophages. J Ethnopharmacol. 2004;95:183–9.
Ostroumova OS, Efimova SS, Chulkov EG, Schagina LV. The interaction of dipole modifiers with polyene-sterol complexes. PLoS ONE. 2012;7:e 45135. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0045135.
Liuqin H, Yulong Y, Tiejun L, Rulin H, Mingyong X, Zhenlong W, et al. Use of the Ussing chamber technique to study nutrient transport by epithelial tissues. Front Biosci. 2013;18:1266–74.
Chavanet P, Clement C, Duong M, Buisson M, D’Athis P, Dumas M, et al. Toxicity and efficacy of conventional amphotericin B deoxycholate versus escalating doses of amphotericin B deoxycholate-fat emulsion in HIV-infected patients with oral candidasis. Clin Microbiol Infect. 1997;3:455–61.
Moribe K, Maruyama K, Iwatsuru M. Encapsulation characteristics of nystatin in liposomes: effects of cholesterol and polyethylene glycol derivatives. Int J Pharm. 1999;188:193–202.
Moribe K, Maruyama K, Iwatsuru M. Molecular localization and state of amphotericin B in PEG liposomes. Int J Pharm. 1999;193:97–106.
Hac-Wydro K, Dynarowicz-Latka P. Interaction between nystatin and natural membrane lipids in Langmuir monolayers-the role of a phospholipid in the mechanism of polyenes mode of action. Biophys Chem. 2006;123:154–61.
Gruszecki WI, Gagos M, Herec M. Dimers of polyene antibiotics amphotericin B detected by means of fluoscence spectroscopy: molecular organization in solution and in lipid membrane. J Photochem Photobiol B. 2003;69:49–57.
Diaz IL, Parra C, Linarez M, Perez LD. Design of micelle nanocontainers based on PDMAEMA-b-PCL-b-PDMAEMA triblock copolymers for the encapsulation of amphotericin B. AAPS Pharm Sci. 2015. doi:10.1208/s12249-015-0298-9.
Sharma JN, Al-Omran A, Parvathy SS. Role of nitric oxide in inflammatory diseases. Inflammopharmacology. 2007;15(6):252–9.
Davidson D, Barefield ES, Kattwinkel J, Dudell G, Damask M, Straube R, et al. Inhaled nitric oxide for the early treatment of persistent pulmonary hypertension of the term newborn: a randomized, double-masked, placebo-controlled, dose–response multicenter study. The I-NO/PPHN Study Group. Pediatrics. 1998;101:325–34.
Herec M, Dziubinska H, Trebacz K, Morzycki JW, Gruszecki WI. An effect of antibiotic amphotericin B on ion transport across model lipid membranes and tonoplast membranes. Biochem Pharmacol. 2005;70:668–75.
Gangadhar KN, Adhikari K, Srichana T. Synthesis and evaluation of sodium deoxycholate sulfate as a lipid drug carrier to enhance the solubility, stability and safety of an amphotericin B inhalation formulation. J Pharm Sci. 2014;471:430–8.
Gheith S, Saghrouni F, Bannour W, Youssef YB, Khelif A, Normand A, et al. In vitro susceptibility to amphotericin B, itraconazole, voriconazole, posaconazole and caspofungin of Aspergillus spp. isolated from patients with haematological malignancies in Tunisia. Springerplus. 2014;3:19.
Kanchan V, Panda AK. Interactions of antigen-loaded polylactide particles with macrophages and their correlation with the immune response. Biomaterials. 2007;28:5344–57.
Rojanarat W, Nakpheng T, Thawithong E, Yanyium N, Srichana T. Inhaled pyrazinamide proliposome for targeting alveolar macrophages. Drug Deliv. 2012;19:334–45.
ACKNOWLEDGMENTS
This work was financially supported by the National Research University Project Grant for PhD Research Programs at the Prince of Songkla University and the PSU-NANOTEC Excellence Center on Drug Delivery System, grant no. PHA 560308S, Department of Pharmaceutical Technology, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Thailand. Also, we thank Dr. Brian Hodgson for assistance with the English language.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adhikari, K., Buatong, W., Thawithong, E. et al. Factors Affecting Enhanced Permeation of Amphotericin B Across Cell Membranes and Safety of Formulation. AAPS PharmSciTech 17, 820–828 (2016). https://doi.org/10.1208/s12249-015-0406-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-015-0406-x