Abstract
Itraconazole is a potent inhibitor of cytochrome P450 3A4 (CYP3A4), associated with numerous drug-drug interactions (DDI). PUR1900, a dry powder formulation of itraconazole for oral inhalation, results in high lung and low systemic exposure. This project used physiologically based pharmacokinetic (PBPK) modeling to assess the DDI potential of inhaled PUR1900, using midazolam as a “victim drug.” The basic and mechanistic static models evaluated the DDI potential of PUR1900, assuming 5 mg of midazolam coadministration at steady-state itraconazole exposure. Subsequently, Simcyp® PBPK simulation software and pharmacokinetic data from a Phase 1 clinical trial with PUR1900 (NCT03479411) were used to optimize an existing itraconazole PBPK model. The model was applied to investigate the potential for CYP3A4 DDI when 5 mg of midazolam is co-administered with inhaled PUR1900 at a steady state in a virtual healthy population at PUR1900 doses up to 40 mg per day. The basic static and mechanistic static models suggested a strong likelihood for DDI with inhaled PUR1900. The PBPK model was consistent with PUR1900 Phase 1 trial data. The geometric mean Cmax and AUC ratios of midazolam at a maximum dose of 40 mg PUR1900 were 1.14 and 1.26, respectively, indicating a minimal likelihood of DDI with inhaled PUR1900. The low systemic exposure of itraconazole when administered as PUR1900 results in minimal to no CYP3A4 inhibition, reducing the concern of drug-drug interactions. As the risk of CYP3A4 DDI is predicted to be significantly lower when itraconazole is administered via oral inhalation as PUR1900, it is likely that PUR1900 can be safely used for the treatment of pulmonary fungal infections in patients taking pharmaceuticals currently contraindicated with oral itraconazole.
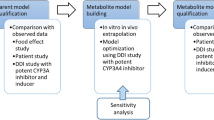
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Itraconazole is a triazole fungicidal with a broad spectrum of activity. Its mechanism of action involves inhibition of the conversion of lanosterol to ergosterol, disrupting fungal cell membrane synthesis (1). The clinical use of oral itraconazole is limited by unpredictable and variable pharmacokinetics, poor tolerability (2), cardiac adverse effects (3, 4), and concerns related to drug-drug interactions (DDI) (5). The DDI potential of itraconazole is related to its activity as a potent inhibitor of the cytochrome P450 3A4 (CYP3A4) isoenzyme (6, 7). The impact on the CPY3A4 pathway alters the metabolism and consequently the plasma concentrations of other drugs metabolized by this pathway (5). Co-administration of a long list of drugs and drug classes with itraconazole is currently contraindicated due to the potential for DDI. The package insert for itraconazole lists over 40 contraindicated drugs and another 256 drugs for which special precautions should be taken (8, 9).
Pulmatrix is developing PUR1900, a dry powder formulation of itraconazole for oral inhalation for the treatment of allergic bronchopulmonary aspergillosis (ABPA) in subjects with asthma and cystic fibrosis (CF). Aspergillus (A.) fumigatus can colonize or infect the airways of patients with asthma and CF and lead to a complex hypersensitivity reaction. ABPA has a prevalence of up to 15% in people with cystic fibrosis (10) and an estimated 1.5% of patients in the general population with asthma (11). Although there is no approved treatment for ABPA, oral itraconazole is commonly prescribed and has been shown to be efficacious (12,13,14). However, the major challenge of itraconazole use is that, because of its potent inhibition of CYP3A4, numerous drugs used in the treatment of exacerbations of asthma or maintenance therapies for CF cannot be used safely with oral itraconazole. In a phase 1 study (NCT03479411) with inhaled itraconazole (PUR1900), high and consistent lung exposure with substantially lower systemic itraconazole exposure was achieved following inhaled delivery relative to oral dosing (15). This limited systemic exposure may be beneficial for patients for whom oral itraconazole is contraindicated.
In order to determine the DDI potential of a maximum 40 mg dose of orally inhaled itraconazole, we used data from previously published systemic exposure following an inhaled dose of 35 mg itraconazole (15). Using these data, we applied a basic static model, a mechanistic static model, and a physiologically based pharmacokinetic (PBPK) model of itraconazole and OH-itraconazole, the primary metabolite of itraconazole, to evaluate the potential risk of PUR1900 as “perpetator” of CYP3A4 DDIs using midazolam as a “victim” drug.
Methods
This was an in silico study using pre-existing data, and no ethical committee approval was required. The methods and results of the PUR1900 Phase 1 clinical study used for static equation calculation and model development are summarized in Hava et al.(15).
Basic Static Model of Reversible Inhibition
The basic and mechanistic static equations have been described in the FDA guidance for in vitro drug interaction studies (16) For PUR1900, the ratio of the intrinsic clearance value of a probe substrate in the absence and in the presence of itraconazole (R1) was calculated using the observed Cmax of itraconazole and OH-itraconazole, respectively, after 14 days of 35 mg of PUR1900 QD (15).
Calculation of the ratio of the intrinsic clearance value of a probe substrate in the absence and in the presence of an inhibitor in the gut (R1,gut) was required for PUR1900, as itraconazole and OH-itraconazole are inhibitors of CYP3A4. Equation input values are listed in Table I.
An R1 ≥1.02 or R1,gut ≥ 11 indicates that a clinically significant drug-drug interaction may exist and requires further investigation (16).
Mechanistic Static Model of Reversible Inhibition
The area under the plasma concentration-time curve ratio (AUCR) for reversible inhibitors was calculated according to the FDA guidance for in vitro drug interaction studies (16).
As a worst-case scenario, it was assumed that all of the inhaled dose was swallowed and subsequently delivered to the gut.
A weak, moderate, or strong DDI is defined as a calculated AUCR (weak: ≥ 1.25-fold, but < 2.00-fold; moderate: ≥ 2.00-fold, but < 5.00-fold; strong: ≥ 5.00-fold) (16).
PBPK Modelling
Study Design and Setup
To achieve the modelling objectives, this step in the investigation consisted of two parts, model optimization and application. Some of the key factors relating to each step are indicated below. Model optimization and application were performed using Simcyp (2019, Version 19 Release 2, Certara, Sheffield, UK). Data assembly and plotting were performed using RStudio (Version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria). The virtual North European Caucasian population (physiological parameters including liver volume and blood flows, enzyme abundances) within Simcyp was used for all simulations (17). Except for demographic data, all parameter values for the healthy volunteer (HV) population are the same as those used for the Caucasian population.
Model Optimization
To simulate the plasma concentration-time profiles of itraconazole and OH-itraconazole after the inhaled administration of 35 mg PUR1900 (QD for 14 days), the Simcyp V19 itraconazole oral solution PBPK model was adapted to include absorption of itraconazole through the lung as well as the gut. The model assumes first-order absorption from the lungs to the systemic circulation. The structural model is shown in Supplemental Figure A. The trial design used for the optimization of first-order inhalation parameters was based on the study described in Hava et al. (15) in which subjects received PUR1900 35 mg QD for 14 days. That study measured itraconazole and OH-itraconazole data as summarized in Supplemental Tables A and B.
For the PBPK model development, ten virtual trials of six subjects, aged 21 to 58 years (33.3% female), were generated to assess variability across groups. The population of the virtual trial was selected to match the clinical study subjects. A range of values was tested for the proportion of dose inhaled, the fraction of itraconazole absorbed from the lung (Fa,1), and the first-order rate constant of itraconazole absorption from the lung (ka,1). These parameters were optimized to best fit the observed plasma concentration-time profiles and PK parameters of itraconazole and OH-itraconazole after multiple dose administration of PUR1900 on study day 14, after 35 mg PUR1900 (QD for 14 days). Briefly, the proportion of dose inhaled and Fa,1 was optimized to match the itraconazole AUC0–24h on study day 14. Then, ka,1 was optimized to capture Cmax. Once the simulated multiple dose and Cmax were within 0.8 to 1.25 of the observed values, the absorption parameters were further optimized to best predict the OH-itraconazole concentration-time profiles. Intestinal absorption, distribution, and elimination parameters of itraconazole and OH-itraconazole were unchanged from the verified itraconazole and OH-itraconazole models, assuming itraconazole follows linear kinetics even at low doses. This model assumes no metabolism of itraconazole to OH-itraconazole in the lung.
The first-order inhalation parameters were manually optimized by comparing the simulated profiles of PUR1900 to observed data. The first-order inhalation parameters used to simulate the plasma concentration profile of PUR1900 are shown in Table II.
Model Application
The CYP3A4 inhibition potential of PUR1900 was predicted using a representative virtual healthy population consisting of ten virtual trials of ten healthy subjects (50% female), aged 20 to 50 years. The victim drug (midazolam) was administered as a single dose of 5 mg without administration of PUR1900, then again on day 14 of daily administration of PUR1900 35 mg. The virtual DDI trials were repeated with the same virtual trial design and study population, with 40 mg of PUR1900 administered daily for 14 days.
Results
Calculation of the R Value for the Basic Model of Reversible Inhibition
R1 was calculated for PUR1900 using the observed maximum concentration of itraconazole and OH-itraconazole following multiple inhaled doses of PUR1900 (35 mg QD) for 14 days. R1 was calculated to be 1.35. Because this value exceeded the cutoff value of 1.02 specified by the FDA guidance document (16), further investigation of DDI liability was required. Additionally, R1,gut was calculated to be greater than the threshold value of 11, indicating that additional assessment of DDI liability was required (16). Based on these results, a mechanistic static model was applied to further investigate the CYP3A4 inhibition potential of PUR1900.
Calculation of AUCR for the Mechanistic Static Equation
AUCR of midazolam was calculated for PUR1900 using the observed maximum concentration of itraconazole and OH-itraconazole following multiple simulated inhaled doses of PUR1900 (35 mg QD) for 14 days. To calculate the worst-case scenario, it was assumed that all itraconazole absorption occurred through the gut. The AUCR of midazolam was calculated to be 5.36, further indicating a risk of PUR1900 as a perpetrator of CYP3A4 DDIs. Based on these results, a PBPK model was developed to further understand the CYP3A4 inhibition potential of PUR1900.
PBPK Model Optimization and Application
Simulated itraconazole and OH-itraconazole plasma concentration data are based on the manually optimized proportion of dose inhaled, (Fa,1), and (ka,1) parameters of PUR1900. Individual mean trial concentrations and the mean concentration-time profiles for the total virtual population (n = 60) were simulated. The simulated profiles of PUR1900 and OH-itraconazole after 14 days of dosing with 35 mg/day of PUR1900 were comparable to the clinical data as shown in Fig. 1. In addition, the predicted geometric mean Cmax and AUC0–24h values for itraconazole on day 14 were within 0.81- and 0.96-fold, respectively, of the observed values (Table III). The predicted mean Cmax and AUC0–24h values for OH-itraconazole on day 14 were within 1.47- and 1.68-fold, respectively, of the observed values (Table IV).
Log-linear a itraconazole and b OH-itraconazole simulated and observed mean plasma concentration-time profiles after multiple oral dose of 35 mg QD PUR1900 for 14 days in healthy subjects. Depicted are simulated (lines) and observed data (circles; mean of n = 6 individuals; Hava et al. 2020). The gray lines represent the 5th and 95th percentiles and the solid black line the mean data for the simulated population (n = 60)
For model application, plasma concentration-time profiles of midazolam following a single oral dose of 5 mg in the absence of PUR1900 and on the 14th day of 14 days of dosing of PUR1900 (35 mg daily or 40 mg daily) to healthy subjects were simulated. The mean simulated plasma concentrations of itraconazole and OH-itraconazole after 14 days of 40 mg daily dosing of PUR1900 are presented in Fig. 2. Mean simulated plasma midazolam concentrations following a single oral dose of 5 mg in the absence of PUR1900 and on the 14th day of 14 days of dosing of PUR1900 (35 mg daily or 40 mg daily) to healthy subjects are shown in Fig. 3. The predicted geometric mean Cmax and AUC0–inf values and corresponding geometric mean ratios for midazolam in the presence and absence of PUR1900 are shown in Table V. The threshold for a weak DDI (AUCR and CmaxR < 1.25) was not met when midazolam was coadministered with 35 mg daily of PUR1900. At the higher dose of 40 mg daily PUR1900, a weak DDI is predicted (AUCR ≥ 1.25 but < 2).
Log-linear a itraconazole and b OH-itraconazole simulated mean plasma concentration-time profiles after multiple oral dose of 40 mg QD PUR1900 for 14 days in healthy subjects. Depicted are simulated (lines). The gray lines represent the 5th and 95th percentiles, and the solid black line the mean data for the simulated population (n = 100)
Simulated log-linear plasma concentration-time profiles of a single 5 mg dose of midazolam, co-administered with steady state a) 35 mg and b) 40 mg of PUR1900 in healthy subjects. Depicted are simulated midazolam plasma concentration-time profiles in the absence of PUR1900 (solid line) and on the 14th day of 14 days of dosing of PUR1900 (dashed line). The lines represent the mean data for the simulated population (n = 100)
Discussion
Itraconazole is an effective treatment for ABPA in patients with asthma and CF (12, 13); however, the high risk of DDI when itraconazole is orally administered with CYP3A4 substrates limits its clinical use. Alternative formulations such as PUR1900, an inhaled formulation of itraconazole, allow for high exposure of itraconazole in the lungs, while minimizing the exposure in the gut and liver.
Previous studies have documented the systemic and pulmonary pharmacokinetics of oral itraconazole in adults and children (18). PUR1900 has been shown to achieve lung exposures that would be considered therapeutic for the treatment of pulmonary aspergillosis, after a single inhaled dose of 20 mg PUR1900 (15). While itraconazole is typically given with a corticosteroid, a study published in 2018 showed that itraconazole monotherapy is often effective in controlling acute ABPA (19). These studies demonstrate that itraconazole is an important tool in the treatment of ABPA.
Due to their extensive metabolism by CYP3A4, a number of CF-related treatments, including medications containing elexacaftor, ivacaftor, and tezacaftor (Trikafta®) (20), should not be used with oral itraconazole (21). Significant dosage adjustments are also recommended with other CFTR modulators such as Symdego®, Orkambi®, and Kalydeco®. Patients with CF are susceptible to numerous bacterial lung infections as well, and certain antibiotics must be used with caution in the presence of itraconazole.
This study used static DDI models and PBPK models to evaluate the extent of CYP3A4 inhibition as a result of inhaled itraconazole via PUR1900. Static models showed a risk that PUR1900 may cause a DDI when coadministered with a sensitive CYP3A4 substrate such as midazolam. Static models for DDI assessment are limited as they do not account for time-dependent changes in drug concentration. Additionally, the assumption that all of the inhaled itraconazole is absorbed through the gut used in the mechanistic static model is conservative to account for a worst-case scenario. In contrast, PBPK models simulate the plasma concentration-time profiles in virtual subjects and allow for absorption through both the gut and lungs (22).
Using PBPK techniques, we sought to evaluate the impact of inhaled itraconazole on the metabolism of midazolam. By adapting the existing oral PBPK model for itraconazole and OH-itraconazole within the Simcyp compound library, which have undergone robust verification with clinical DDI data, there is high confidence in the model predictions for PUR1900. Despite pharmacologic concentrations of itraconazole (the “perpetrator” drug) in the tissues of the lungs, there is minimal itraconazole exposure in the intestines and liver. As a result, there was minimal impact predicted on the metabolism of midazolam (the “victim” drug), despite the over-prediction of the primary active metabolite, OH-itraconazole.
The clinical implications of being able to administer itraconazole safely along with these disease-modifying drugs are clear. These results imply that itraconazole can be safely and effectively administered via an inhaled formulation even in patients taking one or more contraindicated drugs. This should improve the treatment possibilities for vulnerable patients maintained on medications that are contraindicated in the presence of oral itraconazole.
Limitations of this study are that this was an in silico simulation study, and such results must be verified in vivo. In addition, the subjects involved in the PBPK testing were otherwise healthy. However, the relative impact on CYP3A4 function should not be appreciably affected. Specifically, patients with ABPA should have a similar response of the cytochrome P450 system to itraconazole as healthy controls. In fact, Hava et al. (15) reported similar pharmacokinetics in patients with asthma compared to normal controls. Further testing is warranted with older and younger patients with underlying disease, particularly pulmonary disorders. Specific monitoring of blood levels of other victim drugs, including CFTR modulators, co-administered with PUR1900 would be helpful.
Conclusion
The minimal systemic exposure following orally inhaled itraconazole, dosed as PUR1900 dry powder formulation, results in less CYP3A4 inhibition. This is reflected in the weak interaction with midazolam. This can be extrapolated to other CYP3A4 substrates and reduces the concern of drug-drug interactions with PUR1900. It is likely that inhaled itraconazole can be safely used for the treatment of pulmonary fungal infections in patients concurrently treated with pharmaceuticals that are metabolized by CYP3A4.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Odds FC. Itraconazole — a new oral antifungal agent with a very broad spectrum of activity in superficial and systemic mycoses. J Dermatol Sci. 1993;5(2):65–72.
Grant SM, Clissold SP. Itraconazole Drugs. 1989;37(3):310–44.
Fung SL, Chao CH, Yew WW. Cardiovascular adverse effects during itraconazole therapy. Eur Respir J. 2008;32(1):240–240.
Teaford HR, Saleh OMA, Villarraga HR, Enzler MJ, Rivera CG. The many faces of itraconazole cardiac toxicity. Mayo Clinic Proc. 2020;4(6):588–544.
Brüggemann RJM, Alffenaar JWC, Blijlevens NMA, Billaud EM, Kosterink JGW, Verweij PE, et al. Clinical relevance of the pharmacokinetic interactions of azole antifungal drugs with other coadministered agents. Clin Infect Dis. 2009;48(10):1441–58.
Templeton I, Peng CC, Thummel KE, Davis C, Kunze KL, Isoherranen N. Accurate prediction of dose-dependent CYP3A4 inhibition by itraconazole and its metabolites from in vitro inhibition data. Clin Pharmacol Ther. 2010;88:499–505.
Templeton IE, Thummel KE, Kharasch ED, Kunze KL, Hoffer C, Nelson WL, et al. Contribution of itraconazole metabolites to inhibition of CYP3A4 in vivo. Clin Pharmacol Ther. 2008;83:77–85.
Sporanox Capsules, Package insert. 2019. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/020083s063lbl.pdf.
Pharmaceuticals, J. SPORANOX,®,(itraconazole) Oral Solution. 2009. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020657s011s018s019s021lbl.pdf.
Patterson K, Strek ME. Allergic bronchopulmonary aspergillosis. Proc Am Thor Soc. 2010;7:237–44.
Denning DW, Pleuvry A, Cole DC. Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adults. Med Mycol. 2013;51(4):361–70.
Wark PAB, Hensley MJ, Saltos N, Boyle MJ, Toneguzzi RC, Epid GDC, et al. Anti-inflammatory effect of itraconazole in stable allergic bronchopulmonary aspergillosis: a randomized controlled trial. J Allergy Clin Immunol. 2003;111:952–7.
Stevens DA, Schwartz HJ, Lee JY, Moskovitz BL, Jerome DC, Catanzaro A, et al. A randomized trial of itraconazole in allergic bronchopulmonary aspergillosis. New Engl J Med. 2000;342:756–62.
Stiefel Laboratories . NDA 22-484 - Pharmacology reviews - (itraconazole) film-coated tablets, 200mg. 2009. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022484Orig1s000PharmR.pdf.
Hava DL, Tan L, Johnson P, Curran AK, Perry J, Kramer S, et al. A phase 1/1b study of PUR1900, an inhaled formulation of itraconazole, in healthy volunteers and asthmatics to study safety, tolerability and pharmacokinetics. Brit J Clin Pharmaco. 2020;86(4):723–33.
Food and Drug Administration. Clinical drug interaction studies — cytochrome P450 enzyme- and transporter-mediated drug interactions. 2020. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-drug-interaction-studies-cytochrome-p450-enzyme-and-transporter-mediated-drug-interactions.
Howgate E, Yeo KR, Proctor N, Tucker G, Rostami-Hodjegan A. Prediction of in vivo drug clearance from in vitro data. I: impact of inter-individual variability. Xenobiotica. 2006;36(6):473–97.
Conte JE, Golden JA, Kipps J, McIver M, Zurlinden E. Intrapulmonary pharmacokinetics and pharmacodynamics of itraconazole and 14-hydroxyitraconazole at steady state. Antimicrob Agents Chemother. 2004;48:3823–7.
Agarwal R, Dhooria S, Sehgal IS, Aggarwal AN, Garg M, Saikia B, et al. A randomized trial of itraconazole vs prednisolone in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Chest. 2018;153(3):656–64.
Scotet V, L’Hostis C, Férec C. The changing epidemiology of cystic fibrosis: incidence, survival and impact of the CFTR gene discovery. Genes. 2020;11:589.
Trikafta: highlights of prescribing information. 2021. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/212273s004lbl.pdf.
Gerlowski L, Jain R. Physiologically based pharmacokinetic modeling: principles and applications. J Pharm Sci. 1983;72(10):1103–27.
Acknowledgements
The authors wish to acknowledge Edward A. Rose, M.D., MSA for his assistance with the manuscript.
Funding
This study was entirely funded by Pulmatrix Inc., as part of the commercial pharmaceutical development efforts of the company.
Author information
Authors and Affiliations
Contributions
MK, IT, AC, and KK contributed to the conceptualization and design of the work. MK and IT performed all of the modelling and data acquisition. AC and MK wrote the original draft, while IT and KK helped with the review and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
All authors are employees of either Pulmatrix (AC and KK) or Certara (MK and IT), and each has been compensated for their efforts in performing this work as part of their regular duties.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bergagnini-Kolev, M., Kane, K., Templeton, I.E. et al. Evaluation of the Potential for Drug-Drug Interactions with Inhaled Itraconazole Using Physiologically Based Pharmacokinetic Modelling, Based on Phase 1 Clinical Data. AAPS J 25, 62 (2023). https://doi.org/10.1208/s12248-023-00828-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-023-00828-z