Abstract
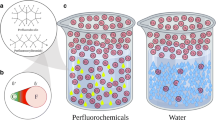
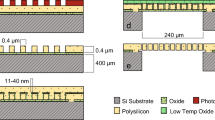
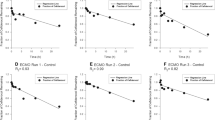
Extracorporeal membrane oxygenation (ECMO) is a life-saving cardiopulmonary bypass device used on critically ill patients with refractory heart and lung failure. Patients supported with ECMO receive numerous drugs to treat critical illnesses and the underlying diseases. Unfortunately, most drugs prescribed to patients on ECMO lack accurate dosing information. Dosing can be variable in this patient population because the ECMO circuit components can adsorb drugs and affect drug exposure substantially. Propofol is a widely used anesthetic in ECMO patients and is known to have high adsorption rates in ECMO circuits due to its high hydrophobicity. In an attempt to reduce adsorption, we encapsulated propofol with Poloxamer 407 (Polyethylene-Polypropylene Glycol). Size and polydispersity index (PDI) were characterized using dynamic light scattering. Encapsulation efficiency was analyzed using High performance liquid chromatography. Cytocompatibility of micelles was analyzed against human macrophages and the formulation was finally injected in an ex-vivo ECMO circuit to determine the adsorption of propofol. Size and PDI of micellar propofol were 25.5 ± 0.8 nm and 0.08 ± 0.01, respectively. Encapsulation efficiency of the drug was 96.1 ± 1.3%. Micellar propofol demonstrated colloidal stability at physiological temperature for a period of 7 days, and was cytocompatible with human macrophages. Micellar propofol demonstrated a significant reduction in adsorption of propofol in the ECMO circuit at earlier time points compared to free propofol (Diprivan®). We observed 97 ± 2% recovery of the propofol from the micellar formulation after an infusion. These results demonstrate the potential of micellar propofol to reduce drug adsorption to ECMO circuit.
Graphical Abstract







Similar content being viewed by others
References
Buck ML. Pharmacokinetic changes during extracorporeal membrane oxygenation: implications for drug therapy of neonates. Clin Pharmacokinet. 2003;42:403–17.
Sherwin J, Heath T, Watt K. Pharmacokinetics and dosing of anti-infective drugs in patients on extracorporeal membrane oxygenation: a review of the current literature. Clin Ther. 2016;38:1976–94.
Watt K, Li JS, Benjamin DK, Cohen-Wolkowiez M. Pediatric cardiovascular drug dosing in critically ill children and extracorporeal membrane oxygenation. J Cardiovasc Pharmacol. 2011;58:126–32.
Palmgrén JJ, Mönkkönen J, Korjamo T, Hassinen A, Auriola S. Drug adsorption to plastic containers and retention of drugs in cultured cells under in vitro conditions. Eur J Pharm Biopharm. 2006;64:369–78.
Preston TJ, Hodge AB, Riley JB, Leib-Sargel C, Nicol KK. In vitro drug adsorption and plasma free hemoglobin levels associated with hollow fiber oxygenators in the extracorporeal life support (ECLS) circuit. J Extra Corpor Technol. 2007;39:234–7.
Preston TJ, Ratliff TM, Gomez D, Olshove VE, Nicol KK, Sargel CL, Chicoine LG. Modified surface coatings and their effect on drug adsorption within the extracorporeal life support circuit. J Extra Corpor Technol. 2010;42:199–202.
Unger JK, Kuehlein G, Schroers A, Gerlach JC, Rossaint R. Adsorption of xenobiotics to plastic tubing incorporated into dynamic in vitro systems used in pharmacological research--limits and progress. Biomater. 2001;22:2031–7.
Ahsman MJ, Hanekamp M, Wildschut ED, Tibboel D, Mathot RA. Population pharmacokinetics of midazolam and its metabolites during venoarterial extracorporeal membrane oxygenation in neonates. Clin Pharmacokinet. 2010;49:407–19.
Ahsman MJ, Wildschut ED, Tibboel D, Mathot RA. Pharmacokinetics of cefotaxime and desacetylcefotaxime in infants during extracorporeal membrane oxygenation. Antimicrob Agents Chemother. 2010;54:1734–41.
Harthan AA, Buckley KW, Heger ML, Fortuna RS, Mays K. Medication adsorption into contemporary extracorporeal membrane oxygenator circuits. J Pediatr Pharmacol Ther. 2014;19:288–95.
van der Vorst MM, Wildschut E, Houmes RJ, Gischler SJ, Kist-van Holthe JE, Burggraaf J, van der Heijden AJ, Tibboel D. Evaluation of furosemide regimens in neonates treated with extracorporeal membrane oxygenation. Crit Care. 2006;10:R168.
Wildschut ED, de Hoog M, Ahsman MJ, Tibboel D, Osterhaus AD, Fraaij PL. Plasma concentrations of oseltamivir and oseltamivir carboxylate in critically ill children on extracorporeal membrane oxygenation support. PLoS One. 2010;5:e10938.
Mulla H, Lawson G, von Anrep C, Burke MD, Upton DU, Firmin RK, Killer H. In vitro evaluation of sedative drug losses during extracorporeal membrane oxygenation. Perfusion. 2000;15:21–6.
Mehta NM, Halwick DR, Dodson BL, Thompson JE, Arnold JH. Potential drug sequestration during extracorporeal membrane oxygenation: results from an ex vivo experiment. Intensive Care Med. 2007;33:1018–24.
Thompson KA, Goodale DB. The recent development of propofol (DIPRIVAN). Intensive Care Med. 2000;26(Suppl 4):S400–4.
Servin F, Desmonts JM, Haberer JP, Cockshott ID, Plummer GF, Farinotti R. Pharmacokinetics and protein binding of propofol in patients with cirrhosis. Anesthesiol. 1988;69:887–91.
Lemaitre F, Hasni N, Leprince P, Corvol E, Belhabib G, Fillâtre P, Luyt CE, Leven C, Farinotti R, Fernandez C, Combes A. Propofol, midazolam, vancomycin and cyclosporine therapeutic drug monitoring in extracorporeal membrane oxygenation circuits primed with whole human blood. Crit Care. 2015;19:40.
Kabanov AV, Alakhov VY. Pluronic block copolymers in drug delivery: from micellar nanocontainers to biological response modifiers. Crit Rev Ther Drug Carrier Syst. 2002;19:1–72.
Kwon GS. Polymeric micelles for delivery of poorly water-soluble compounds. Crit Rev Ther Drug Carrier Syst. 2003;20:357–403.
Kabanov AV, Batrakova EV, Alakhov VY. Pluronic block copolymers as novel polymer therapeutics for drug and gene delivery. J Control Release. 2002;82:189–212.
Imburgia CE, Rower JE, Green DJ, Mcknite AM, Kelley WE, Reilly CA, Watt KM. Remdesivir and GS-441524 extraction by ex vivo extracorporeal life support circuits. ASAIO J. 2022;68:1204–10.
Wright SP. Adjusted P-values for simultaneous inference. Biom. 1992;48:1005–13.
Benjamini Y, Krieger AM, Yekutieli D. Adaptive linear step-up procedures that control the false discovery rate. Biometrika. 2006;93:491–507.
He T, He J, Wang Z, Cui Z. Modification strategies to improve the membrane hemocompatibility in extracorporeal membrane oxygenator (ECMO). Adv Compos Hybrid Mater. 2021;4:847–64.
Kim SC, Kim DW, Shim YH, Bang JS, Oh HS, Wan Kim S, Seo MH. In vivo evaluation of polymeric micellar paclitaxel formulation: toxicity and efficacy. J Control Release. 2001;72:191–202.
Cabral H, Miyata K, Osada K, Kataoka K. Block copolymer micelles in nanomedicine applications. Chem Rev. 2018;118:6844–92.
Daniel JM, Bernard PA, Skinner SC, Bhandary P, Ruzic A, Bacon MK, Ballard HO. Hollow Fiber oxygenator composition has a significant impact on failure rates in neonates on extracorporeal membrane oxygenation: a retrospective analysis. J Pediatr Intensive Care. 2018;7:7–13.
Lequier L, Horton SB, McMullan DM, Bartlett RH. Extracorporeal membrane oxygenation circuitry. Pediatr Crit Care Med. 2013;14:S7–12.
Fragomeni G, Terzini M, Comite A, Catapano G. The maximal pore size of hydrophobic microporous membranes does not fully characterize the resistance to plasma breakthrough of membrane devices for extracorporeal blood oxygenation. Front Bioeng Biotechnol. 2019;7:461.
Dumortier G, Grossiord JL, Agnely F, Chaumeil JC. A review of poloxamer 407 pharmaceutical and pharmacological characteristics. Pharm Res. 2006;23:2709–28.
Fakhar-Ud-Din, Khan GM. Development and characterisation of levosulpiride-loaded suppositories with improved bioavailability in vivo. Pharm Dev Technol. 2019;24:63–9.
Alakhov V, Klinski E, Lemieux P, Pietrzynski G, Kabanov A. Block copolymeric biotransport carriers as versatile vehicles for drug delivery. Expert Opin Biol Ther. 2001;1:583–602.
Acknowledgments
This work made use of University of Utah shared facilities of the Micron Technology Foundation Inc. Microscopy Suite sponsored by the College of Engineering, Health Sciences Center, Office of the Vice President for Research, and the Utah Science Technology and Research (USTAR) initiative of the State of Utah.
Funding
This work was funded by the University of Utah Clinical and Translational Science Institute Pilot award program. It was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Conceptualization: Nitish Khurana, Till Suenner, Venkata Yellepeddi, Kevin Watt, Hamidreza Ghandehari; Methodology: Nitish Khurana, Till Suenner, Oliver Hubbard, Carina Imburgia; Formal analysis: Nitish Khurana, Till Suenner, Oliver Hubbard, Gregory Stoddard; Investigation: Nitish Khurana, Till Suenner, Oliver Hubbard, Carina Imburgia; Resources: Venkata Yellepeddi, Kevin Watt, Hamidreza Ghandehari; Writing – Original Draft: Nitish Khurana; Writing – Review and editing: Nitish Khurana, Till Suenner, Oliver Hubbard, Carina Imburgia, Venkata Yellepeddi, Kevin Watt, Hamidreza Ghandehari, Gregory Stoddard; Supervision: Nitish Khurana, Venkata Yellepeddi, Kevin Watt, Hamidreza Ghandehari; Funding acquisition: Nitish Khurana, Venkata Yellepeddi, Kevin Watt, Hamidreza Ghandehari.
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any conflict of interest to report.
Additional information
Responsible Editor: Aliasger Salem
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 224 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khurana, N., Sünner, T., Hubbard, O. et al. Micellar Encapsulation of Propofol Reduces its Adsorption on Extracorporeal Membrane Oxygenator (ECMO) Circuit. AAPS J 25, 52 (2023). https://doi.org/10.1208/s12248-023-00817-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-023-00817-2