Abstract
In chemistry, rate processes are defined in terms of rate constants, with units of time−1, and are derived by differential equations from amounts. In contrast, when considering drug concentrations in biological systems, particularly in humans, rate processes must be defined in terms of clearance, with units of volume/time, since biological volumes, which are highly dependent on drug partition into biological tissues, cannot be easily determined. In pharmacology, pharmacokinetics, and in making drug dosing decisions, drug clearance and changes in drug clearance are paramount. Clearance is defined as the amount of drug eliminated or moved divided by the exposure driving that elimination or movement. Historically, all clearance derivations in pharmacology and pharmacokinetics have been based on the use of differential equations in terms of rate constants and amounts, which are then converted into clearance equations when multiplied/divided by a hypothesized volume of distribution. Here, we show that except for iv bolus dosing, multiple volumes may be relevant. We have recently shown that clearance relationships, as well as rate constant relationships, may be derived independent of differential equations using Kirchhoff’s Laws from physics. Kirchhoff’s Laws may be simply translated to recognize that when two or more rate-defining processes operate in parallel, the total value of the overall reaction parameter is equal to the sum of those rate-defining processes. In contrast, when two or more rate-defining processes operate in series, the inverse of the total reaction parameter is equal to the sum of the inverse of those rate-defining steps.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ever since the field of clinical pharmacology began evaluating drug concentrations in humans to characterize the pharmacokinetics of drugs and make drug dosing decisions, the equations utilized have been developed based on differential equations for first-order rate processes. Here, we present the proposition that although differential equation derivations are appropriate for chemical reactions in a fixed-volume beaker, they may misrepresent or fail to adequately characterize human pharmacokinetic processes for which the individual rate processes can occur in biological regions with differing volumes of drug distribution. In pharmacokinetics, the observed rate of elimination is a function of both clearance and varying volumes of distribution for the different processes in the body, but in chemistry, the observed rate of elimination is only a function of rate constants since all reactions occur in a fixed-volume beaker. We also demonstrate that Kirchhoff’s Laws may simplify the approach to defining chemical reactions and that Kirchhoff’s Laws for in-series processes are in fact consistent with routinely used mean residence time concepts in pharmacokinetics, but that the implications of these analyses have not been recognized.
As we previously detailed (1), rates of reaction are derived and defined in chemistry in terms of rate constants and driving force amounts following linear force-flow relations, as given in Eq. 1
where J is some sort of flux or current, f is the driving force or impetus causing that flux, and K is a coefficient of proportionality that determines the magnitude of the flux response to the input force. We see this relationship for Fick’s Law of diffusion, Ohm’s Law for electric current, heat transfer relationships, and drag force on falling objects. Applied to chemical rates of reaction
where the rate constants, k, have units of time−1 and amounts, A, have units of mass. Even if the chemistry reaction is carried out in a solution, where concentrations are measured, we can easily convert this to an amount by multiplying the concentration by the volume of fluid in which the reaction is measured. The rate of the reaction can be defined using differential equations that include the rate constants and the amounts driving the reaction. In contrast, for in vivo pharmacology and pharmacokinetics, the equivalent of Eqs. 1 and 2 is
where clearance, CL, has units of volume per time and concentration has units of mass per volume. Clearance is defined as the amount of drug eliminated or moved divided by the drug exposure driving that elimination or movement over all time (2). For an intravenous bolus dose of drug, clearance may be calculated using Eq. 4
where \({AUC}_{0\to \infty }\) is the area under the systemic concentration time curve over all time following the bolus dose.
Clearance is the most important pharmacokinetic parameter as it defines the dosing rate for drugs in patients to achieve efficacy and minimize toxicity. At any \(i\) th time point, the rate of elimination (Relim, i) equivalent of Eq. 4 is given by
where Ci is the measured concentration at the \(i\) th time point. Historically, clearance parameters are determined by deriving the relevant rate of elimination processes from drug amounts using differential equations, often solving the equations at steady state so that the rate of elimination in the differential equation may be set to zero. The resulting equations are then multiplied by a volume of distribution term to convert the rate constants into clearances. In other words, this approach is exemplified by first using Eq. 2 to relate the rate of elimination to drug amount (dose) but then is converted to a clearance by multiplying the rate constant, and dividing the amount, by volume of drug distribution (Eq. 3). This approach is useful in pharmacokinetics and pharmacology, where concentrations of drug in systemic fluids are measured rather than amounts. Until now, this was the only methodology available to derive clearance relationships. However, in this manuscript, we show why this frequently leads to invalid equations due to assuming a single volume of distribution for the various pharmacokinetic processes.
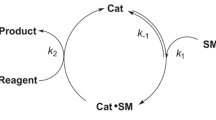
The primary sites for drug elimination of small molecules in the body are the liver and the kidney, although other elimination sites are possible, such as the lung for volatile compounds and macrophages for macromolecules, such as antibodies. In the kidney, there are several renal elimination processes that occur independent of each other, in parallel. In contrast, in the liver, there are several hepatic elimination processes that occur in series. We asked: can clearance rates for each elimination process be simply combined into total net clearance rates independent of any mechanistic model, allowing clearance in the kidney and liver to be determined without solving differential equations? We accomplished this using Kirchhoff’s Laws (1). If this is possible, we further asked: can we also derive the chemical rates of reaction without solving differential equations?
Theory and Practice
Application of Kirchhoff’s Laws to Eliminate the Need for Solving Differential Equations
More than a century and a half ago, Gustav Kirchhoff presented publications concerning applications of Ohm’s Laws for electric currents. His work has been identified as Kirchhoff’s Laws and their application to electrical processes in parallel and in series designated as Kirchhoff’s Loop Rules that can be found in elementary Physics textbooks (3, 4). Here, we reference book material that can be downloaded for free on-line (openpress.usask.ca/physics155/). Application of the first Law demonstrates that when two electrical resistors are in parallel, the total conductance (the inverse of resistance) is equal to the sum of the individual conductances. Application of the second Law demonstrates that when two resistors are in series, the inverse of the total conductance is equal to the sum of the inverse conductance for each resistor. Applications of Kirchhoff’s Laws are consistent with Eq. 1 as stated above. We reasoned that processes in pharmacology, pharmacokinetics, and chemistry also are consistent with Eq. 1 and that Kirchhoff’s Laws are applicable to deriving the kinetic relationships both for rate constants (Eq. 2) and clearances (Eq. 3) independent of differential Eqs. (1). Thus, there is now a way to derive clearance equations independent of the differential equation-based process, which has been followed since clearance was first recognized as the defining parameter in drug dosing a half-century ago. That is, it is now no longer necessary to derive the kinetic relationship in terms of rate constants and amounts, set the differential equation equal to zero at steady state, and then multiply the rate constant by a volume of distribution term and divide the amount by volume of distribution, to define clearance. Furthermore, for chemistry reactions, it is not necessary to derive the kinetic relationships and define the rate constants for first-order processes using differential equations.
As we report (1), the application of Kirchhoff’s Laws to clearance can be summarized in Eq. 6 for parallel processes and Eq. 7 for processes in series.
Equations 6 and 7 allow derivation of total clearance in Eq. 3. However, Kirchhoff’s Laws may also be applied to rate constants (and the total rate constant in Eq. 2) and can be derived via Eqs. 8 and 9, independent of solving differential equations for first-order processes.
A rate-defining process is a parameter that describes an elimination or movement process for which it is possible under certain conditions that the total clearance or total rate constant may be equal to this value. For example, a rate-defining clearance process for hepatic elimination could be hepatic blood flow, i.e., the rate at which drug arrives to the liver is the maximum value that hepatic elimination can be. Thus, for a very high hepatic clearance (CLH) drug, total CLH would equal hepatic blood flow. To exemplify a rate-defining rate constant process, for a series of chemical reactions occurring in a beaker, the elimination rate constant for the parent drug could be the minimum value rate-defining process for all subsequent metabolic steps. In contrast, basolateral hepatic efflux transport cannot be a rate-defining process since it is not possible for clearance or rate of elimination to be solely equal to this parameter.
Application of Kirchhoff’s Laws to Determine Rate Constants for In-Series Metabolic Steps
We now examine a hypothetical drug metabolism scenario where the drug (\(D\)) is metabolized to a first metabolite (\(M1\)) and partially excreted unchanged in the urine, which is then further metabolized to a second in-series metabolite (\(M2\)) and partially excreted in the urine, which is then further metabolized in series to a third metabolite (\(M3\)).

The advantage of utilizing Kirchhoff’s Laws for describing the rate of \(M2\) elimination is that the coefficient of proportionality (the measured elimination rate constant for \(M2\)) is determined based on the measured outcome and the rate-determining driving force parameters (the individual rate constants). Thus, for the in-series metabolism scenario pictured above
Assuming that the values for overall elimination of the drug and the metabolites by metabolism plus urinary excretion are kd = 0.07 h−1, km1 = 0.12 h−1, and km2 = 0.42 h−1, the measured \(M2\) elimination rate constant according to Eq. 10 will be 0.040 h−1. Therefore, if we wanted to predict the measured rate of the reaction (mass/time) for the elimination of \(M2\) in Eq. 2, it would be 0.040 multiplied by the amount of drug \(D\) we added to the beaker that reaches \(M2\). Prior to this publication, how would we have estimated this parameter? We demonstrate in the Appendix the process we would follow. That is, derive the differential equation for the measured concentrations of \(M2\) (CM2) as a function of time. We carried out the derivation using Laplace transforms. We then solved the equation for CM2 as a function of time. We then determined the mean residence time of \(M2\); the inverse of which would be the measured rate of elimination of \(M2\). This value is 0.040 h−1, the same value reached here using Kirchhoff’s Laws. As far as we can tell, we are the first to recognize that Kirchhoff’s Laws can be used to simply define measured reaction rates for in-series processes without carrying out the derivation in the Appendix.
Application of Kirchhoff’s Laws to In-Series Rate-Defining Steps for In Vivo Hepatic Clearance
A major advance in our application of Kirchhoff’s Laws to hepatic clearance (1) was the recognition that for hepatic elimination, the in-series rate-defining clearance processes could be (a) clearance entering, which is hepatic blood flow (QH) and (b) clearance leaving, which is hepatic clearance, i.e., the product of the fraction unbound to blood proteins (fuB) and the sum of the intrinsic ability of the liver to metabolize and to excrete unbound drug into the bile, independent of blood flow (CLint). As we point out in Pachter et al. (1), the CLint term is the sum of two parallel elimination processes (CLint metabolism + CLint biliary excretion). Thus, in a general approach
where CLentering is hepatic blood flow and CLleaving is metabolism of unbound drug
Solving Eq. 12 gives
For the past 50 years in the pharmacokinetic literature, Eq. 13 had previously been considered as the well-stirred model of hepatic elimination, based on the differential equation and steady-state derivation of Rowland, Benet, and Graham (5) for hepatic blood flow and intrinsic clearance plus the addition of the protein binding term by Wilkinson and Shand (6). Here, Eq. 13 was derived making no assumptions related to the mechanistic characteristics of hepatic elimination. It is organ model independent. Based on this recognition, we now understand why all steady-state isolated perfused rat liver clearance data, the only experimental studies that directly test the various hepatic disposition models, appear to preferentially fit what was previously believed to be the well-stirred model (7). It is because, in fact, Eq. 13 is a model-independent relationship and not the well-stirred model of hepatic disposition as the field has regarded it to be. Even in early 2022, we (8) also continued to mistakenly consider Eq. 13 to be the well-stirred model, since we had participated in the initial steps of its derivation (5). Therefore, there appears to be no value to predicting whole body clearance values utilizing different mechanistic models of hepatic organ elimination (e.g., parallel tube, dispersion, well-stirred), as is presently employed in some physiologically based pharmacokinetic (PBPK) approaches. To clarify, this manuscript is not questioning nor debating the pros and cons of the various hepatic disposition models. The thesis of this manuscript is focused on the methodologies employed to analyze pharmacokinetic data and obtain correct measures of pharmacokinetic parameters, i.e., the differential equation approach versus the approach presented here based on Kirchhoff’s Laws. The derivation of Eq. 13, independent of differential equations, is an excellent example of the advantage of the Kirchhoff’s Law approach.
Adding Rate Defining Basolateral Transport to Hepatic Clearance: The Extended Clearance Equation
In Pachter et al. (1), we noted that previously Eq. 13 had been commonly used in clearance predictions when hepatic metabolism was the only relevant process, although assuming it was the well-stirred model; however, the incorrect hepatic clearance equation was being employed when the possibility of basolateral transporters could be the rate-defining process. This is an area of strong interest, since lipid-lowering statins (HMG CoA reductase inhibitors) and other large molecular weight acids are found to be substrates of organic anion transporting polypeptides (OATPs) and inhibition of these transporters can significantly affect the pharmacokinetics of such drugs. Thus, when basolateral transporters are clinically significant, there are two entering clearances in series in Eq. 11, and Eq. 12 equivalent becomes
where PSinflux is basolateral influx clearance and PSefflux is basolateral efflux clearance. Kirchhoff never considered simultaneous reversible steps in his derivations, and one may ask why the difference in basolateral transport is assumed in Eq. 14, rather than separating out the two processes? Recall in the above discussion following Eq. 9 that Kirchhoff’s Laws applied to pharmacology, pharmacokinetics, and chemistry hold for combining rate-defining processes. Thus, we cannot ignore PSefflux, as it will certainly affect hepatic clearance, but it cannot be a rate-defining process by itself, as it is a negative parameter, and drug has to enter the liver prior to being effluxed out. Therefore, the rate-defining basolateral hepatic transport process is the difference between influx and efflux clearances. Of course, if basolateral transporters are not clinically relevant, then Eq. 14 reverts to Eq. 12. This is true since passive diffusion into and out of an organ is never a rate-defining process. There are no experimental studies where a diffusion rate constant or clearance has been identified as a rate-defining process. However, more frequently when basolateral transporters are relevant, it is assumed that the hepatic blood flow entering clearance is much larger than the other two processes, so under such conditions Eq. 14 would ignore the blood flow process, resulting in Eq. 15
which when solved for CLH yields
Equation 16 is the correct extended clearance concept equation, rather than the equation universally reported in the literature (e.g., references 9,10,11,12,13,14). When CLint is much larger than \(({PS}_{\mathrm{influx}}-{PS}_{\mathrm{efflux}})\), the difference in basolateral transporter clearances becomes rate defining and when CLint is much smaller than \(({PS}_{\mathrm{influx}}-{PS}_{\mathrm{efflux}})\), CLint becomes rate defining. In the presently employed equation found throughout the literature, there are two erroneous outcomes: (a) PSefflux must be zero for transporters to become the rate-defining process, and (b) it is impossible for CLint to become the rate-defining process independent of basolateral transporter clearances, as we previously detailed (1).
It is important to recognize that \({PS}_{\mathrm{influx}}\) and \({PS}_{\mathrm{efflux}}\) are the summation of both passive and active permeability clearances. If there is no active transport, or under the very unlikely condition that active transport in both directions is equal, or if \({PS}_{\mathrm{efflux}}\) is greater than \({PS}_{\mathrm{influx}}\), these cannot be rate-defining processes for clearance and thus they would not be included in Kirchhoff’s Law derivation. Thus, both in the liver and in the kidney (\({CL}_{\mathrm{secretion}}-{CL}_{\mathrm{reabsorption}})\), the difference must be positive for these parameters to be rate defining. One should also recognize that in vitro attempts to predict changes in membrane permeability will always be measures of the differences in the permeability clearances, rather than the individual permeability clearances themselves.
Rate Defining vs. Rate Limiting
In Pachter et al. (1), we described the use of Kirchhoff’s Laws in terms of “rate-limiting processes,” where we now refine the nomenclature to “rate-defining processes.” We do this because rate-limiting processes may be viewed as the upper and lower limits of the overall relationship. Thus, for Eq. 12, we may view hepatic blood flow (QH) as the upper limit of hepatic clearance, which it is. Correspondingly, we may then view hepatic metabolism (fuB·CLint) as the lower limit of hepatic clearance, which it is not. It is well recognized that hepatic clearance is not greater than QH; however, it may not be well recognized that hepatic clearance will often be less than fuB·CLint. For example, if QH is 1500 ml/min and fuB·CLint is 750 ml/min, CLH calculated by Eq. 13 will be 500 ml/min as also recently detailed (15). Therefore, hepatic metabolism (fuB·CLint) should be considered a rate-defining process, rather than a rate-limiting process.
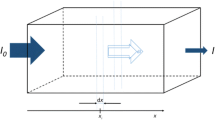
Kirchhoff’s Laws vs. Differential Equation Derivations of Clearance Following Oral Dosing
The marked advantage of Kirchhoff’s Laws is that the equations are directly derived in terms of the parameter of relevance, here organ clearance. This is in contrast to the traditional way in which pharmacokinetic relationships have been historically derived using differential equations that consider amounts and rate constants, which are then converted to concentrations/clearances by dividing/multiplying by volume of distribution. This difference between the Kirchhoff’s Laws’ approach and the traditional differential equation approach can be exemplified by analyzing oral absorption. Consider first-order absorption (absorption rate constant ka) into a 1-compartment body model (disposition rate constant kd) where bioavailability is F and all drug is eliminated by renal processes unchanged so that clearance has no effects on first pass gut and liver elimination process. Solving the differential equation for the amount of drug in the systemic circulation (Asystemic circulation) as a function of time, t, gives
Converting Eq. 17 into a concentration (C) relationship by dividing by the systemic volume of distribution (V) yields
Integrating Eq. 18 over all time to determine the area under the curve (AUC) and dividing the available oral dose by this area yield Eq. 19 that has been universally taught and believed to be the clearance after oral dosing.
Thus, based on the resulting equation from the differential equation approach, our field teaches that after oral dosing the absorption process has no effect on the measured clearance (it is identical to the clearance determined following iv bolus dosing). This is believed to be true independent of the value of F and true independent of the clearance affecting hepatic (and gut) bioavailability.
Now, let us examine the Kirchhoff’s Laws derivation for oral absorption in terms of clearance measures. Rewriting Eq. 11
where CLleaving for our 1-compartment body model is CLiv bolus, which equals kd·V, and CLentering would be clearance from the gut, a parameter that is never measured but could be envisioned as the product of the absorption rate constant (determined from the inverse of the mean absorption time) and the volume of distribution of drug in the gut (which is frequently taken to be 250 ml for all drugs in bottom-up attempts to predict first pass gut metabolism or intestinal drug-drug interactions). But let us leave CLentering as CLgut so that Eq. 20 becomes
that when solved gives
There are important considerations for Eq. 22. First, it demonstrates that the clearance measured after oral dosing is not the iv bolus clearance unless CLgut > > CLiv bolus, which is unlikely to be true in many cases. Yes, the absorption rate constant will most frequently be greater than the disposition rate constant, but we are comparing clearances, not rate constants, and we suspect that the volume of distribution in the systemic circulation will be markedly greater than the volume of distribution of drug in the gut. Yet, it is well known that the absorption rate constant can be less than the elimination rate constant in the well-recognized flip-flop models. Also, in the derivation of Eq. 19 using differential equations, we are not required to make any assumption about bioavailability (F) since CLafter oral dosing is known if we also give an iv bolus dose. The value of bioavailability does not affect the value of clearance. However, this is not true for the Kirchhoff’s Laws derivation, since even when we have given an iv bolus dose to determine CLiv bolus, we cannot determine CLgut unless we know F. Therefore, what is the difference between the differential equation derivation and the Kirchhoff’s Laws derivation? We carried out the differential equation derivation in terms of rate constants and then converted the systemic amount to systemic concentration by the systemic volume of distribution, not recognizing that the absorption rate constant from the gut is multiplied by the systemic volume of distribution rather than the gut volume of distribution. Note in Eq. 18 that the concentration driving absorption is not the gut concentration but the same systemic concentration driving elimination.
The Field of Pharmacokinetics Has Been Using Approaches Consistent with Kirchhoff’s Laws for Rate Constants, but Never Recognized the Implications of These Calculations in Terms of Clearance
More than 40 years ago, Yamaoka et al. (16) recognized that the absorption-disposition model described in Eqs. 17 and 18 could be described by mean residence time concepts so that the mean residence time for drug in the systemic circulation could be given by
What was not fully appreciated or calculated, however, was that the mean residence time of drug in the systemic circulation was the inverse of the rate constant from Eq. 2 (i.e., mean residence time in the systemic circulation after oral dosing = 1/rate constant of reaction after oral dosing) that relates the rate of reaction to the amount of drug driving the reaction so that
The rate constant of reaction after oral dosing in Eq. 24 is the rate constant determined from the slope of the terminal log linear phase following oral dosing for a drug where after iv bolus dosing the terminal slope is consistent with kd. Thus, the rate of the reaction following oral dosing would only be described by the elimination constant kd if ka were much greater than kd. Converting Eq. 24 to characterize the rate of reaction in terms of clearance parameters in Eq. 3, thereby changing the ka rate constants into clearance of absorption and the kd rate constant into clearance of elimination via an iv bolus dose, yields Eq. 22. Mean residence time concepts for in-series steps are inherently defined by Kirchhoff’s Laws. Thus, the field has been using Kirchhoff’s Laws concepts in pharmacokinetics for approximately the same time period as the importance of clearance in defining pharmacokinetic processes has been recognized. The field just had never previously used Kirchhoff’s Laws to define clearance relationships as we do here.
Discussion
In this paper, we show how rates of reactions for first-order processes can be determined independent of differential equation derivations when (a) amounts drive the reaction and the coefficient of proportionality is a rate constant (Eq. 2) as is applicable in chemistry and (b) when concentrations drive the reaction and the coefficient of proportionality is a clearance (Eq. 3) as is applicable in pharmacology and pharmacokinetics and in choosing and adjusting drug dosing. We accomplish this by applying Kirchhoff’s Laws for rate-defining processes that are either in parallel or in series as we recently demonstrated (1). Reviewers have asked us to stress that in the present manuscript we are only considering first-order processes. We will address non-first-order and saturable systems in a future publication, but the great majority of pharmacokinetic theory and evaluations are consistent with first-order processes. We characterize a rate-defining process as either a rate constant or a clearance that under certain conditions could potentially singly predict the relationships between the rate of reaction and the driving force for that reaction in Eqs. 2 and 3, even when other processes are known to be operational. For example, hepatic drug elimination could be affected by hepatic blood flow, by transport at the basolateral hepatocyte membrane, and by elimination by hepatic metabolism and/or biliary excretion. For certain drugs, it is possible that each of these processes may effectively singly describe elimination if the other processes are significantly larger. The coefficients of proportionality (an overall system rate constant in Eq. 2 and an overall system clearance in Eq. 3) are derived by summing parallel rate-defining processes (Eqs. 6 and 8) and by summing the inverse of the rate-defining in-series processes that is equal to the inverse of the overall system value for in-series processes (Eqs. 7 and 9).
We also showed that although we first identified the universal application of Kirchhoff’s Laws to solving the coefficients of proportionality for first-order reactions in chemistry and pharmacokinetics independent of differential equation derivations; in fact, the process had been unknowingly utilized in pharmacokinetics for at least four decades in mean residence time calculations (see above). This identification of the unrecognized long-term use of Kirchhoff’s Laws to define rate constants as inverse mean residence time parameters provides the clue as to why Kirchhoff’s Laws may be used under non-steady-state conditions. It is generally believed that Kirchhoff’s Laws are only applicable to steady-state conditions (3, 4). However, it is well recognized in chemical kinetics and pharmacokinetics that for linear systems the integration of amounts or concentrations following the time course of a reaction or a single dose of a drug over all time will yield the same measure as obtained at steady state, where n is the number of doses and τ is the dosing interval. For example,
Thus, we believe that the reason Kirchhoff’s Laws appear to be valid for single-dose drug pharmacokinetics and chemical reactions is that the parameters are a function of integration over all time, which is equivalent to steady-state conditions when those parameters are determined.
The most important contribution in this manuscript is the recognition that the clearance of in-series processes in pharmacology and pharmacokinetics can be derived independent of differential equations. Prior to the Pachter et al. (1) publication, the only method available to derive clearance relationships was to solve the rate of drug elimination using rate constants (Eq. 2) to include all the potential relevant pharmacokinetic processes and then multiply/divide the resulting equation by the volume of distribution of drug in the fluid in which the drug concentrations are measured. This works fine in chemical reactions where all processes occur in the same volume of distribution, the fluid volume of the reaction mixture. Thus, in chemistry, there is no need to determine clearance. But in pharmacokinetics, the in vivo volumes of distribution of the parent drug and its subsequent in-series metabolites will all be different. Therefore, the differential equation approach we presently utilize will frequently not correctly quantitatively characterize the clearance that drives the in vivo processes. The organs of elimination, primarily the liver and kidney, can only remove drugs from the blood flowing to those organs. The end purpose of metabolism is to make xenobiotics more polar so that their volume of distribution will be smaller, and thus, more of the xenobiotic will be in the blood and more easily removed from the body. This is the teleological explanation for phase I and phase II metabolism, where the phase II conjugative processes make the xenobiotic substance even more polar than the phase I metabolism by adding, e.g., glucuronide and sulfate, moieties.
We point out that the differential equation and clearance derivation for the parent drug approach will only give the correct rate of reaction for the processes for an iv bolus dose of drug. This is because for an iv bolus dose there is only one rate-defining process, the clearance of parent drug from the systemic circulation. In all other pharmacokinetic scenarios, there will be clearance entering, such as absorption from an oral dose or an intramuscular or a subcutaneous dose, and even a zero order infusion. With an iv bolus dose, we assume that clearance entering is infinite so that clearance leaving of parent drug (elimination) is the only relevant process and only one volume term is of relevance. However, all other presently derived clearance equations for any in-series in vivo relationship will only be correct if the numerical values of potential rate-defining processes are so different that one does not affect the other. This is also true for parallel processes, since CLentering must always be in series with the parallel processes. In Pachter et al. (1), we used renal clearance to exemplify parallel pharmacokinetic processes.
However, there are also in-series processes related to renal elimination, since kidney blood flow (QK) can also be rate defining. The correct renal clearance equation following an iv bolus dose should include CLentering as QK.
We note that both hepatic and renal clearances may be defined by three potential rate-defining processes: (a) blood flow, (b) reversible permeability processes (PSinflux − PSefflux) in the liver and \({(CL}_{\mathrm{secretion}}-{CL}_{\mathrm{reabsorption}})\) in the kidney, and (c) unidirectional elimination processes (CLint,metabolic + CLint, biliary) in the liver and \({CL}_{\mathrm{Glomerular Filtration}}\) in the kidney. Thus, recognizing what processes are in parallel and what processes are in series, using Kirchhoff’s Laws one may immediately derive the relevant equations for CLH and CLR. Then, depending upon the values expected for each of the three processes, the equations can be modulated to eliminate one or even two of the three potential rate-defining processes. We do recognize that if extensive drug excreted into the bile is reabsorbed, the simple derivation becomes significantly more complicated, but believe this becomes a bioavailability issue, not a clearance phenomenon.
Above we stated that the most important contribution in this manuscript is the recognition that the clearance of in-series processes in pharmacology and pharmacokinetics can be derived independent of differential equations. The major relevant finding from this recognition is that the field has been misinterpreting bioavailability concepts and has incorrectly taught and believe that absorption processes have no effect on clearance measurements (i.e., Eq. 19). The field recognizes that F is the product of the fraction of the dose absorbed (Fabs), the fraction of the dose that gets through the intestinal membranes unmetabolized into the portal vein (Fgut), and the fraction of drug not metabolized nor biliary excreted during hepatic first pass (Fhepatic), which are all processes with differing driving force concentrations. The differential equation derivation assumes that all these processes are driven by F·Dose, rather than incrementally decreasing as drug reaches the hepatic vein. That is, there is a marked disconnect between the differential equation derivation and the physiology of the various first-pass processes that are inherently driven by different concentrations. This approach is further confounded, since Fhepatic is dependent on clearance itself.
A major outcome of this analysis is the recognition that it is not possible to determine bioavailability following oral dosing when one only knows Doseoral and measures\({AUC}_{0\to \infty }\), since there are two unknowns, CLafter oral dosing and F, as given in Eq. 22. This finding has significant effects on the accuracy and relevance of present bioavailability measures and could explain why frequently investigators observe dose corrected measures of \(\frac{{AUC}_{0\to \infty , \mathrm{non}-\mathrm{iv\;bolus}}}{{AUC}_{0\to \infty , \mathrm{iv\;bolus}}}\) greater than 1.0 following intramuscular, subcutaneous, and oral dosing that we will address separately. However, here we present one example to illustrate the issue. Well-respected Swedish scientists from the National Board of Health and Welfare (17) reported following oral and iv bolus administration of cimetidine in 10 healthy subjects that dose corrected \(\frac{{AUC}_{0\to \infty , \mathrm{oral}}}{{AUC}_{0\to \infty , \mathrm{iv\,bolus}}}\) was 110.6%, while the dose corrected urinary excretion ratio of unchanged drug \((\frac{{\mathrm{Amount excreted unchanged}}_{\mathrm{oral}}}{{\mathrm{Amount excreted unchanged}}_{\mathrm{iv bolus }}})\) was 59.5%. The authors conclude the paper stating “The results clearly demonstrate that bioavailability studies using AUC-measurements are misleading for several drugs including cimetidine.” But now, we believe that the Kirchhoff’s Laws approach can potentially explain the results. The average bioavailability is accurately predicted from the urinary data, F = 0.595, since the urinary excretion values are independent of any model or calculated relationship. Taking the published (17) average clearance from systemic concentrations for a 100 mg iv bolus dose (45.5 L/hr) and the published average AUC0→∞ for the 400 mg oral dose (10.4 mg·hr/L), we can determine CLafter oral dosing from Eq. 22 as 22.9 L/hr. Then, using Eq. 22, CLgut can be calculated to be 46.1 L/hr. That is, the fast systemic clearance of cimetidine due to active secretion in the kidney tubule after an iv bolus dose is almost the same as the clearance of cimetidine from the gut as it is absorbed. Thus, the systemic AUC of cimetidine following oral dosing will be markedly affected by both gut clearance and systemic clearance. From the Kirchhoff’s Law’s derivation, the finding of a dose-corrected AUC ratio (oral/iv) greater than 1.0 is not an error in measurement, rather a result of believing that determining clearance via differential equations and dividing by the systemic volume of distribution is valid. We believe that the application of Kirchhoff’s Laws to calculate the overall clearance term in Eq. 3 allows the correct relationship to be determined.
Conclusions
-
Clearance relationships, as well as rate constant relationships, may be derived independent of differential equations using Kirchhoff’s Laws from physics.
-
Clearance in the liver and kidney may be derived using Kirchhoff’s Laws by appropriately considering three potential rate-defining processes: (a) blood flow, (b) reversible permeability, and (c) unidirectional elimination.
-
Prior to the recent recognition that Kirchhoff’s Laws can be applied to characterize pharmacokinetic processes (1), utilizing differential equations was the only available approach to deriving clearance equations, which relies on a volume of distribution term.
-
The traditional differential equation approach relates the rate of elimination to drug amount, but then is converted to a clearance by dividing/multiplying by volume of distribution, to convert drug amounts to concentrations and the rate constant to a clearance. This methodology assumes that a single volume of distribution governs the various pharmacokinetic processes. An assumption we will investigate in detail in our next publication.
-
The field of pharmacokinetics has been utilizing Kirchhoff’s Laws to evaluate in-series rate constant steps for decades, without recognizing it. However, the application of Kirchhoff’s Laws to in-series clearance steps had not previously been employed.
-
When calculating the overall rate constant relationships exemplified by Eq. 2, the simplified Kirchhoff’s Law approach gives the same results obtained from the multistep differential equation analysis, since differences in distribution volume for different processes are not relevant when calculating rate constants. However, for clearance relationships exemplified by Eq. 3, only Kirchhoff’s Laws may give the correct result due to the fact that differences in volumes of distribution do affect clearance determinations.
-
The approach presented here provides the pharmacokinetic community with an opportunity to analyze and interpret pharmacokinetic relationships without requiring the use of hepatic disposition models with differing degrees of complexities and assumptions and without needing to consider differences in volume of distribution for the various pharmacokinetic processes. The current approach enhances understanding of how to best analyze and interpret pharmacokinetic relationships.
Data Availability
All of the data is in the manuscript.
References
Pachter JA, Dill KA, Sodhi JK, Benet LZ. Review of the application of Kirchhoff’s Laws of series and parallel flows to pharmacology: defining organ clearance. Pharmacol Ther. 2022;239: 108278.
Benet LZ, Sodhi JK, Makrygiorgos G, Mesbah A. There is only one valid definition of clearance: critical examination of clearance concepts reveals the potential errors in clinical drug dosing decisions. AAPS J. 2021;23:67.
Ling SJ, Sanny J, Moebs W, Janzen D. Introduction to electricity, magnetism and circuits. University of Saskatchewan, Distance Education Unit, Saskatoon, 2018.
Ling SJ, Sanny J, Moebs W. University physics volume 2. OpenStax, Rice University, Houston, 2016.
Rowland M, Benet LZ, Graham GG. Clearance concepts in pharmacokinetics. J Pharmacokinet Biopharm. 1973;1:123–35.
Wilkinson GR, Shand DG. Commentary: a physiologic approach to hepatic drug clearance. Clin Pharmacol Ther. 1975;18:377–90.
Sodhi JK, Wang H-J, Benet LZ. Are there any experimental perfusion data that preferentially support the dispersion and parallel-tube models over the well-stirred model of organ elimination? Drug Metab Dispos. 2020;48:537–43.
Benet LZ, Sodhi JK. Can in vitro-in vivo extrapolation be successful? Recognizing the incorrect clearance assumptions. Clin Pharmacol Ther. 2022;111:1022–35.
Sirianni GL, Pang KS. Organ clearance concepts: new perspectives on old principles. J Pharmacokinet Biopharm. 1997;25:449–70.
Webborn PHJ, Parker AJ, Denton RL, Riley RJ. In vitro-in vivo extrapolation of hepatic clearance involving active uptake: theoretical and experimental aspects. Xenobiotica. 2007;37:1090–109.
Kusuhara H, Sugiyama Y. In vitro-in vivo extrapolation of transporter-mediated clearance in the liver and kidney. Drug Metab Pharmacokinet. 2009;24:37–52.
Caminesh G, Umehara K. Predicting human hepatic clearance for in vitro drug metabolism and transport data: a scientific and pharmaceutical perspective for assessing drug-drug interactions. Biopharm Drug Dispos. 2012;33:179–94.
Barton HA, Lai Y, Goosen TC, Jones HM, El-Kattan AF, Gossed JR, et al. Model-based approaches to predict drug-drug interactions associated with hepatic uptake transporters: preclinical, clinical and beyond. Exp Opin Drug Metab Toxicol. 2013;9:459–72.
Patelia-Vrana G, Unadkat JD. Transport and metabolism: what determines the pharmacokinetics and pharmacodynamics of drugs. Clin Pharmacol Ther. 2016;100:413–8.
Jusko WJ, Li X. Assessment of the Kochak-Benet equation for hepatic clearance for the parallel-tube model: relevance of classic clearance concepts in PK and PBPK. AAPS J. 2022;24:5.
Yamaoka K, Nakagawa T, Uno T. Statistical moments in pharmacokinetics. J Pharmacokinet Biopharm. 1979;6:547–58.
Grahnén A, von Bahr AC, Lindström B, Rosén A. Bioavailability and pharmacokinetics of cimetidine. Eur J Clin Pharmacol. 1979;16:335–40.
Benet LZ. General treatment of linear mammillary models with elimination from any compartment as used in pharmacokinetics. J Pharm Sci. 1972;61:536–40.
Funding
This work was supported by the UCSF Benet Fund for Excellence generated from individual contributions and Dr. Benet’s consultation, expert witness, and board of director fees that are made payable to the Regents of the University of California. Dr. Benet is a member of the UCSF Liver Center supported by NIH grant P30 DK026743.
Author information
Authors and Affiliations
Contributions
Leslie Z. Benet and Jasleen K. Sodhi conceived the study, derived and analyzed the equations, and wrote the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. In-series metabolic steps
Appendix. In-series metabolic steps
Characteristics
For the metabolic process

Let us assume for the scheme above that the drug and the metabolites can each be described by a one-compartment model, that intravenous bolus dosing of drug \(M1\) and \(M2\) was carried out separately, and that both plasma and urine concentrations were measured so that the following parameters could all be determined.
Solving for Concentration of M2 Using the Traditional Differential Equation Approach
The Laplace transform of the concentration of \(M2\) (18) for this metabolic process in terms of micromoles, where s is the Laplace operator, will be
Solving the Laplace transform for the micromoles of \(M2\) as a function of time
Substituting the individual values from above gives the concentration of \(M2\) (μM/L) with time as
One may now calculate the mean residence time for \(M2\), by determining area under the moment curve (AUMC) from the sum of the coefficients divided by the exponents squared, and area under the curve (AUC) from the sum of the coefficients divided by the exponents (16)
Thus, the overall measured rate constant for the elimination of \(M2\) would be the inverse of the calculated mean residence time for \(M2\) or 0.040 h−1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Benet, L.Z., Sodhi, J.K. The Uses and Advantages of Kirchhoff’s Laws vs. Differential Equations in Pharmacology, Pharmacokinetics, and (Even) Chemistry. AAPS J 25, 38 (2023). https://doi.org/10.1208/s12248-023-00801-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-023-00801-w