Abstract
Eflornithine is a recommended treatment against late-stage gambiense human African trypanosomiasis, a neglected tropical disease. Standard dosing of eflornithine consists of repeated intravenous infusions of a racemic mixture of L- and D-eflornithine. Data from three clinical studies, (i) eflornithine intravenous monotherapy, (ii) nifurtimox-eflornithine combination therapy, and (iii) eflornithine oral monotherapy, were pooled and analyzed using a time-to-event pharmacodynamic modeling approach, supported by in vitro activity data of the individual enantiomers. Our aim was to assess (i) the efficacy of the eflornithine regimens in a time-to-event analysis and (ii) the feasibility of an L-eflornithine-based therapy integrating clinical and preclinical data. A pharmacodynamic time-to-event model was used to estimate the total dose of eflornithine, associated with 50% reduction in baseline hazard, when administered as monotherapy or in the nifurtimox-eflornithine combination therapy. The estimated total doses were 159, 60 and 291 g for intravenous eflornithine monotherapy, nifurtimox-eflornithine combination therapy and oral eflornithine monotherapy, respectively. Simulations suggested that L-eflornithine achieves a higher predicted median survival, compared to when racemate is administered, as treatment against late-stage gambiense human African trypanosomiasis. Our findings showed that oral L-eflornithine-based monotherapy would not result in adequate efficacy, even at high dose, and warrants further investigations to assess the potential of oral L-eflornithine-based treatment in combination with other treatments such as nifurtimox. An all-oral eflornithine-based regimen would provide easier access to treatment and reduce burden on patients and healthcare systems in gambiense human African trypanosomiasis endemic areas.

Graphical abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Human African trypanosomiasis (HAT), also known as sleeping sickness, is recognized by the World Health Organization as a neglected tropical disease (1). HAT is a fatal parasitic disease unless treated. HAT, spread via the tsetse fly, is caused by either the Trypanosoma brucei gambiense or Trypanosoma brucei rhodesiense strains (2). However, the Trypanosoma brucei gambiense causes 98% of the total HAT cases (3). For gambiense HAT (g-HAT), 51 million people in sub-Saharan Africa are estimated to live in areas at risk of being infected, and over five million people live in areas with moderate or higher risk of infection (3). Eflornithine is a recommended treatment against late-stage g-HAT, i.e., when the parasites have also infected the central nervous system (4, 5). Eflornithine was initially developed for oncology indications and was later discovered as an effective antitrypanosomal therapy (6, 7). It is included in World Health Organization’s model list of essential medicines (8). Currently, only an intravenous racemic mixture of L- and D-eflornithine is a recommended treatment administered as monotherapy over 14 days, or as a combination with oral nifurtimox (NECT) for 7 days (5, 9,10,11,12). An oral eflornithine-based treatment alternative would improve treatment access for patients and reduce the demand on healthcare resources. We have previously progressed the understanding of the enantioselective pharmacokinetics of eflornithine both preclinically and clinically (13,14,15). Recently, we also established the enantioselective in vitro antitrypanosomal activity where L-eflornithine showed a nine-fold greater antitrypanosomal potency compared to D-eflornithine (16). The present study aimed to integrate current knowledge on enantioselective pharmacokinetics and potency, along pharmacodynamic time-to-event modeling of eflornithine treatment success or failure in published clinical cohorts. Simulation framework was set up to evaluate the feasibility of potential clinical approaches to oral L-eflornithine treatment.
MATERIALS AND METHODS
Pharmacodynamic Time-to-Event Modeling Approach
Data Set
Individual treatment outcome data (cure or treatment failure) and eflornithine dosing information were collected from three previously published clinical studies with late-stage g-HAT patients (Table I) (n = 1248 across the three studies). In study 1, racemic eflornithine was administered intravenously as monotherapy (17); in study 2, intravenous racemic eflornithine was combined with oral nifurtimox in the NECT regimen (18); and in study, 3 racemic eflornithine was administered orally as monotherapy (19). Successful treatment was defined as (i) no parasite in cerebrospinal fluid, lymph or blood or (ii) if patients’ self-assessments were considered at good health at the follow-up visit. Treatment failures were defined either as disease-related death or as recurrent infection. The studies included only confirmed late-stage g-HAT patients and were all conducted in endemic areas in Central or Western Africa.
Pharmacodynamic Time-to-Event Model Development
The pharmacodynamic modeling was performed using NONMEM v7.4 (ICON Development Solutions, Ellicott City, MD, USA) (20). Piraña v2.9.8, Rstudio v1.3.1093, the R software v4.1.1 (The R foundation for Statistical Computing), Perl-speaks-NONMEM (PsN) v4.8.1 (Department of Pharmaceutical Biosciences, Uppsala University, Uppsala, Sweden) (21) and Xpose v4.7.1 (22, 23) were used for model assessments, diagnostics, and visualization of results. Pharmacodynamic model parameters were obtained using the Laplacian estimation method. The objective function value (OFV) calculated by NONMEM is proportional to -2log likelihood of the data for the specific model. The drop in objective function value (ΔOFV) was assumed to be χ2 distributed. Model discrimination between nested (hierarchical) models was determined by likelihood ratio testing based on ΔOFV. ΔOFV > 3.84 was considered as a statistically significant improvement of the model with P < 0.05 for one degree of freedom. Model diagnostics were done by evaluating the Kaplan-Meier curve in a visual predictive check (n = 1,000) and bootstrap (n = 1,000) to resample the included clinical studies and obtain confidence intervals of the parameter estimates. The time-to-event analysis was performed with an assumed Weibull hazard distribution. The shape parameter was fixed to 1 for the clinical trial with orally administered racemic eflornithine, as data were too limited to allow for estimation of this parameter. Total eflornithine dose in each clinical study was assumed to be the driving factor of effect and was included as a time constant effect in the model; i.e., the probability of a specific pharmacodynamic outcome was dependent on total eflornithine dose in grams (Table I). Outcome was implemented by interval censoring (treatment failure events) or right censoring at the end of 12 months of study follow-up (successful treatment). Patients lost to follow-up were right censored at the time of their last follow-up visit (24). The time-to-event analysis was performed using a survival function (S(t)), based on the baseline hazard (φ) and the shape factor of the Weibull function (γ), according to (Eq. 1). The probability (p(t)) of an event was calculated by a probability density function (Eq. 2).
The inhibitory effect of eflornithine treatment was implemented as a sigmoidal maximum inhibition response (Imax) on the baseline hazard, i.e., dose-response model (Eq. 3).
The parameters estimated in this model were BASE, representing baseline hazard for event; ID50, representing the dose associated with 50% reduction in baseline hazard; and DOSE, representing the total eflornithine dose administered in each study to estimate the time-to-event (Table I). Model parameters Imax and sigmoidicity factor (n) were both fixed to 1, assuming full inhibition was possible with a fixed slope. The baseline hazard, Weibull shape and ID50 parameters were estimated separately for each clinical trial, since attempts to estimate these in a pooled modeling approach failed (i.e., incorporating all data from the three studies and deriving a global parameter estimate).
Enantioselective Potency Prediction
After dosing of racemic eflornithine intravenously, the steady-state concentrations of L-eflornithine and D-eflornithine have been shown to be similar (13, 15), whereas oral dosing resulted in approximately 50% lower steady-state concentrations of L-eflornithine compared to that of D-eflornithine, i.e., a 1:2 L-eflornithine:D-eflornithine plasma exposure ratio (13,14,15). However, in vitro susceptibility data from a previous publication showed that L-eflornithine has higher antitrypanosomal activity compared to D-eflornithine (16). The original data from this in vitro study are freely accessible from the Swedish National Data Service (SND-ID: 2021-45) database (25). The enantiospecific potencies of L-eflornithine, D-eflornithine, and the 1:2 L-eflornithine:D-eflornithine concentration ratio associated with oral administration were estimated from these data using a mathematical modeling approach in the software Phoenix v8.3 (Certara, Princeton, NJ, USA). Potencies were estimated using an inhibitory Imax model that considers the competitive interaction for two ligands (L-eflornithine and D-eflornithine) acting on the same target with same mode of action (26, 27) (Eq. 4). E0 represents the effect, measured as relative fluorescence in the AlamarBlue serial drug dilution assay (28), at zero drug concentration and when measured background fluorescence in the assay was taken into consideration (i.e., media without parasites). CL-eflornithine and CD-eflornithine correspond to the separate incubation concentrations. IC50L-eflornithine and IC50D-eflornithine correspond to the estimated L-eflornithine (5.5 μM) and D-eflornithine (49.6 μM) potencies.
Treatment Outcome Simulations
The developed pharmacodynamic time-to-event model was used to simulate outcome scenarios for treatment with L-eflornithine. All simulations were performed with a constant total L-eflornithine dose at 333 g, i.e., similar to the total dose administered in study 3 and shown to be tolerated by late-stage g-HAT patients. This corresponds to 100 to 125 mg/kg doses, four times daily, administered in study 3. To determine the clinical ID50 parameter for L-eflornithine in the simulations, the ID50 parameter associated with racemic eflornithine was adjusted for the derived in vitro potency using Eq. 4 to delineate the individual contributions from L-eflornithine and D-eflornithine. The study-dependent parameters, i.e., Weibull shape and baseline hazard, were fixed in the simulations.
RESULTS
Pharmacodynamic Modeling Results
The final pharmacodynamic model described the time-to-event (treatment failure) adequately for g-HAT patients in the three clinical studies. Estimated baseline hazards were 0.035, 0.026 and 0.077 month−1 for study 1 with intravenous eflornithine, study 2 with intravenous eflornithine combined with oral nifurtimox and study 3 with oral eflornithine, respectively. Estimated ID50 values were 159, 60 and 291 g for study 1, study 2, and study 3, respectively (Table II). Kaplan-Meier curves of observed clinical trial data overlaid with 95% confidence intervals obtained from simulations (n = 1,000) with the final pharmacodynamic model showed highest survival for NECT and lowest survival for the oral eflornithine monotherapy (Fig. 1).
Visual predictive check of final pharmacodynamic model for a intravenous racemic eflornithine monotherapy, b intravenous racemic eflornithine in combination with oral nifurtimox (NECT), and c oral racemic eflornithine monotherapy. Black lines show the Kaplan-Meier curve for observed data and gray areas are the 95% confidence intervals obtained from 1,000 simulations with the pharmacodynamic time-to-event model. Note the different y-axis scale in Fig. 1c
Enantioselective Potency Prediction
The adjustment of ID50 was based on the in vitro 50% inhibitory concentration (IC50) ratio between L-eflornithine (16) using freely accessible data from the Swedish National Data Service (SND-ID: 2021-45) database (25) and predicted IC50 for the 1:2 L-eflornithine:D-eflornithine plasma exposure ratio observed in late-stage g-HAT patients after oral dosing of racemic eflornithine (14) (Fig. 2). Additional model fits for L-eflornithine and D-eflornithine are provided in the supplementary material (Fig. S1, Table SI). The predicted IC50 for the 1:2 L-eflornithine:D-eflornithine plasma exposure ratio was 13.4 μM derived from Eq. 4 based on the experimental in vitro IC50 values for L-eflornithine and D-eflornithine at 5.5 μM and 49.6 μM, respectively (16). The mathematical model was also able to estimate in vitro efficacy for racemic eflornithine, i.e., at 1:1 ratio for L-eflornithine and D-eflornithine (Fig. 2), when compared to data from the literature (16, 25).
a Predicted in vitro efficacy for racemic eflornithine (dashed turquoise line) with gray area showing 5th to 95th percentiles of experimental data from a previous study (16) shown here for visual assessment of model performance. b Predicted in vitro efficacy for the 1:2 L-eflornithine:D-eflornithine plasma exposure ratio (dashed purple line) to retrieve a potency estimate for racemic eflornithine after oral administration. Predictions were made with a mathematical modeling approach using experimental in vitro data from a previous study (16) for L-eflornithine (dashed green line) and D-eflornithine (solid red line). Data were accessed from the Swedish National Data Service (SND-ID: 2021-45) database (25)
Additional model fits for L-eflornithine and D-eflornithine are provided in the supplementary material (Fig. S1). The predicted IC50 for the 1:2 L-eflornithine:D-eflornithine plasma exposure ratio was 13.4 μM derived from Eq. 4 based on the experimental in vitro IC50 values for L-eflornithine and D-eflornithine at 5.5 μM and 49.6 μM, respectively (16).
Predicted Survival for Oral L-eflornithine as Monotherapy
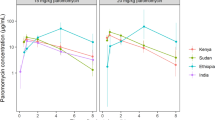
Simulations were performed using the final pharmacodynamic time-to-event model, with the drug efficacy adjusted for enantiomer difference in in vitro potency, to predict survival after treatment with oral L-eflornithine monotherapy. Estimated ID50 for study 3 with oral racemic eflornithine monotherapy at 291 g in the pharmacodynamic model was decreased by 2.46-fold (13.4 μM/5.5 μM) to 118 g in the simulations for oral L-eflornithine monotherapy assuming an unchanged oral bioavailability for L-eflornithine when administered as an enantiopure formulation (Supplementary material Table SII). The predicted survival at 12 months was higher for an L-eflornithine treatment with median (95% CI) survival at 80% (64 to 92%) at a total dose of 333 g (corresponding to 100 to 125 mg/kg administered four times daily) compared to oral racemic eflornithine monotherapy at 68% (48 to 84%) using the estimated pharmacodynamic model parameters from study 3 (19) (Fig. 3). The predicted 95% CI in survival ranged between 64 and 99% when assessed by the three simulated scenarios at a total L-eflornithine dose of 333 g.
Median predicted survival (%) in the studies for intravenous racemic eflornithine monotherapy (black diamond), intravenous racemic eflornithine in combination with oral nifurtimox (black triangle) and oral racemic eflornithine monotherapy (black square) at 12 months. Median predicted survival (%) for oral L-eflornithine monotherapy at 333 g total dose (green squares) at 12 months. Error bars represent the 95% confidence interval for the simulated scenarios (n = 1,000). The gray shaded area cover the predictions based on the NECT study
DISCUSSION
The observed event-free proportion of patients in the two included intravenous eflornithine studies was above 96% at the 12-month follow-up (Fig. 1), demonstrating the efficacy of these treatments against late-stage g-HAT. For the oral eflornithine study population, the overall observed event-free proportion of patients was 76% at the end of the 12-month follow-up period. This is indicative of a sub-therapeutic treatment and/or a high risk of infection in the endemic area where the study was performed. The antiparasitic in vitro efficacy of eflornithine is enantioselective (16), and the proportion of L- and D-eflornithine enantiomers influences the treatment success to a great extent. Due to enantioselective absorption, oral administration of racemic eflornithine results in 33/66 proportion of the L- and D-eflornithine enantiomers, while intravenously administered racemic eflornithine give a 50/50 ratio.
The developed pharmacodynamic time-to-event model adequately estimated the survival (absence of death or reinfection) for the three different clinical studies analyzed in the present study, based on the model selection criteria set out. The time-to-event analysis demonstrated that NECT was slightly superior to intravenous eflornithine monotherapy, while both NECT and intravenous monotherapy were superior to oral eflornithine monotherapy against late-stage g-HAT. This is in line with previous findings (9). In the oral monotherapy study with the highest probability of an event per time unit (BASE), the observed overall survival decreased to 80% or lower in four months (Fig. 1), which indicated high recurrent infection rates in this study population. As observed in Fig. 1 and shown by simulations with oral L-eflornithine monotherapy (Fig. 3), the predicted median survival after 12-month follow-up is higher (80%) compared to oral racemic eflornithine monotherapy (68%). However, due to the low sample size in study 3 (n = 25), the 95% confidence intervals are wide and overlap when predicted from this study, suggesting that L-eflornithine might not be an efficacious oral monotherapy treatment.
In the oral monotherapy study with racemic eflornithine, the oral bioavailability of the more active L-eflornithine enantiomer (16) was too low to render adequate drug exposure and cure the late-stage g-HAT patients (14). In preclinical studies, the oral bioavailability for L-eflornithine, when dosing racemic mixture, was 26–47% (13, 15), and similar absolute bioavailability for the more active L-eflornithine enantiomer is plausible in late-stage g-HAT patients (14). The 1:2 ratio of absorbed L-eflornithine and D-eflornithine in the systemic circulation after oral dosing appears to be conserved across preclinical and clinical studies. On the other hand, the drug concentration ratio in cerebrospinal fluid to plasma was similar for L-eflornithine and D-eflornithine in late-stage g-HAT patients, indicative of a non-stereoselective uptake mechanism to the central nervous system (14). However, the lower exposure of L-eflornithine in plasma would translate to lower concentrations in the cerebrospinal fluid compared to D-eflornithine. For an enantiopure formulation with L-eflornithine, a higher L-eflornithine concentration in the cerebrospinal fluid is expected at equimolar doses of racemic mixture, as the proportions of L- and D-eflornithine in the systemic circulation are 100/0, respectively, instead of 33/66.
In line with current treatment recommendations for eflornithine monotherapy, dosing 400 mg/kg/day dosed every 6 h for 14 days resulted in a curative treatment outcome (12). A shorter treatment period for intravenous eflornithine monotherapy of 7 days was not feasible due to an unacceptable rate of treatment failure (29). Intravenous monotherapy has been studied with less frequent dosing at 400 mg/kg/day dosed every 12 h (30). This regimen gave total eflornithine concentration in cerebrospinal fluid below the suggested clinical cut-off value at 50 μmol/L and lower frequency of successful treatment. Total eflornithine doses higher than administered in the monotherapy studies have been associated with more side effects (31, 32). For instance, higher eflornithine concentrations in the cerebrospinal fluid have been associated with convulsions (30, 33). If adverse effects such as vomiting, diarrhea, and/or nausea after oral administration are equally driven by the enantiomers, equimolar doses of racemic or L-eflornithine could be tolerable for late-stage g-HAT patients. However, tolerability would need to be assessed in future clinical studies. In late-stage g-HAT patients, the majority of drug related side effects for racemic eflornithine was reversible by decreasing the dose or treatment discontinuation (33). Moreover, fewer major adverse events (fever, neutropenia, hypertension, diarrhea or infections) were observed for the NECT regimen compared to eflornithine monotherapy (9, 34, 35). Whether systemic and/or local gastrointestinal dose-limiting side effects observed in late-stage g-HAT patients after administration of oral racemic eflornithine can be attributed to L-eflornithine, D-eflornithine or total eflornithine dose is yet to be determined.
Currently, NECT is the only drug combination to treat late-stage g-HAT. This regimen is non-inferior to intravenous monotherapy despite less frequent dosing and shorter treatment duration of racemic eflornithine, i.e., potentiating the clinical efficacy of eflornithine (9). The higher in vitro efficacy for L-eflornithine in combination with the nifurtimox-dependent potentiation is clinically relevant to investigate further in a prospective clinical study. For parasitic disease in general, combination treatments have been successfully used to manage emerging drug resistance, and the need of drug combinations will potentially increase since the risk for drug resistance development in parasites is lower when two or more drugs with different mechanisms of action are combined compared to monotherapy (36). Recent advances with fexinidazole (37, 38), an approved all-oral therapy against g-HAT for patients with leukocyte count <100 per μL in the cerebrospinal fluid, and acoziborole that is investigated in clinical studies are promising (39). Future drug combination strategies with, for instance, fexinidazole, eflornithine, nifurtimox, and/or potentially acoziborole might be needed to decrease the potential risk for drug resistance development against g-HAT treatments.
The present study is not without limitations. Firstly, the baseline hazard in the pharmacodynamic model would preferably be determined from a placebo cohort living in an area with risk of infection. No placebo data were available in the studies nor the literature, likely due to ethical considerations. Attempts to estimate overall baseline hazard, Weibull shape, and ID50 parameters for all treatment arms failed, as the parameter estimation precision in the pharmacodynamic model was poor. Therefore, the baseline hazard, Weibull shape, and ID50 parameters for each study were estimated separately. Secondly, the Weibull distribution shape parameter for oral racemic eflornithine was fixed to 1, as the limited data did not allow estimation of this parameter. The limited oral eflornithine data available from only 25 patients resulted in relatively uncertain parameter estimates and survival predictions, as evident in the wide confidence intervals derived. More data in the orally dosed cohort may have improved the precision of the pharmacodynamic model and allowed an overall baseline hazard, Weibull shape, and ID50 parameter estimation. Predictions made in the simulated scenarios were made with assumptions regarding studied populations and generalizability from the three clinical studies included to develop the pharmacodynamic time-to-event model as well as the predicted in vitro potency for the 1:2 L-eflornithine:D-eflornithine plasma exposure ratio. Thirdly, a pharmacokinetic-pharmacodynamic exposure-response model that link exposure variables or dynamic concentrations to outcome, instead of the developed dose-response model, would provide a greater understanding of this relationship. Unfortunately, no individual patient pharmacokinetic data were available. Lastly, a confirmatory external data set from a clinical study would be desirable to validate the pharmacodynamic model predictions in the present study for L-eflornithine.
CONCLUSION
The time-to-event analysis showed that NECT was similar to intravenous eflornithine monotherapy, and both were superior to oral eflornithine monotherapy against late-stage g-HAT. The oral bioavailability of the more active enantiomer, L-eflornithine, when dosed as an oral racemic mixture was too low for successful treatment. The developed model predicted a higher survival after oral L-eflornithine monotherapy compared to oral racemic eflornithine monotherapy. Oral L-eflornithine, administered at a total dose of 333 g equal to 100 to 125 mg/kg doses four times daily for a late-stage g-HAT patient with 51 kg bodyweight, may achieve a median survival of 80% or higher. A potential future clinical study could investigate the maximum tolerated dose and minimum effective concentration of L-eflornithine in plasma and/or cerebrospinal fluid to establish an optimal oral dosing frequency and treatment duration. The oral L-eflornithine treatment could also be combined with nifurtimox and/or possibly other g-HAT treatments such as fexinidazole. Modeling and simulation presented here show that the potential for an oral eflornithine-based treatment for late-stage g-HAT would require an efficacy improvement beyond oral L-eflornithine monotherapy at a high dose, and further research is warranted to determine if a future oral late-stage g-HAT treatment with L-eflornithine-based combinations would be feasible or not.
References
WHO. Accelerating Work to overcome the global impact of neglected tropical diseases: A roadmap for implementation. WHO Executive Summary. 2012.
Kennedy PG. Human African trypanosomiasis of the CNS: current issues and challenges. J Clin Invest. 2004;113(4):496–504. https://doi.org/10.1172/JCI21052.
Franco JR, Cecchi G, Priotto G, Paone M, Diarra A, Grout L, Simarro PP, Zhao W, Argaw D. Monitoring the elimination of human African trypanosomiasis at continental and country level: Update to 2018. PLoS Negl Trop Dis. 2020;14(5):e0008261. https://doi.org/10.1371/journal.pntd.0008261.
Kennedy PG. Human African trypanosomiasis: in and out of Africa. Neurology. 2006;66(7):962–3. https://doi.org/10.1212/01.wnl.0000208221.55385.55.
Nightingale SL. From the Food and Drug Administration. Jama. 1991;265(10):1229.
Coyne PE Jr. The eflornithine story. J Am Acad Dermatol. 2001;45(5):784–6. https://doi.org/10.1067/mjd.2001.117853.
Bacchi CJ, Nathan HC, Hutner SH, McCann PP, Sjoerdsma A. Polyamine metabolism: a potential therapeutic target in trypanosomes. Science (New York, NY). 1980;210(4467):332-4.
WHO. WHO model list of essential medicines, 16th list March 2009. 2009;Available from www.who.int/medicines/publications/essentialmedicines/en/, Accessed Jan 7, 2022.
Priotto G, Kasparian S, Mutombo W, Ngouama D, Ghorashian S, Arnold U, Ghabri S, Baudin E, Buard V, Kazadi-Kyanza S, Ilunga M, Mutangala W, Pohlig G, Schmid C, Karunakara U, Torreele E, Kande V. Nifurtimox-eflornithine combination therapy for second-stage African Trypanosoma brucei gambiense trypanosomiasis: a multicentre, randomised, phase III, non-inferiority trial. Lancet. 2009;374(9683):56–64. https://doi.org/10.1016/S0140-6736(09)61117-X.
Checchi F, Piola P, Ayikoru H, Thomas F, Legros D, Priotto G. Nifurtimox plus Eflornithine for late-stage sleeping sickness in Uganda: a case series. PLoS Negl Trop Dis. 2007;1(2):e64. https://doi.org/10.1371/journal.pntd.0000064.
Priotto G, Kasparian S, Ngouama D, Ghorashian S, Arnold U, Ghabri S, Karunakara U. Nifurtimox-eflornithine combination therapy for second-stage Trypanosoma brucei gambiense sleeping sickness: a randomized clinical trial in Congo. Clin Infect Dis. 2007;45(11):1435–42. https://doi.org/10.1086/522982.
WHO. WHO interim guidelines for the treatment of gambiense human African trypanosomiasis. 2019.
Jansson R, Malm M, Roth C, Ashton M. Enantioselective and nonlinear intestinal absorption of eflornithine in the rat. Antimicrob Agents Chemother. 2008;52(8):2842–8. https://doi.org/10.1128/AAC.00050-08.
Jansson-Lofmark R, Na-Bangchang K, Bjorkman S, Doua F, Ashton M. Enantiospecific reassessment of the pharmacokinetics and pharmacodynamics of oral eflornithine against late-stage Trypanosoma brucei gambiense sleeping sickness. Antimicrob Agents Chemother. 2015;59(2):1299–307. https://doi.org/10.1128/AAC.04101-14.
Johansson CC, Gennemark P, Artursson P, Abelo A, Ashton M, Jansson-Lofmark R. Population pharmacokinetic modeling and deconvolution of enantioselective absorption of eflornithine in the rat. J Pharmacokinet Pharmacodyn. 2013;40(1):117–28. https://doi.org/10.1007/s10928-012-9293-x.
Boberg M, Cal M, Kaiser M, Jansson-Lofmark R, Maser P, Ashton M. Enantiospecific antitrypanosomal in vitro activity of eflornithine. PLoS Negl Trop Dis. 2021;15(7):e0009583. https://doi.org/10.1371/journal.pntd.0009583.
Priotto G, Pinoges L, Fursa IB, Burke B, Nicolay N, Grillet G, Hewison C, Balasegaram M. Safety and effectiveness of first line eflornithine for Trypanosoma brucei gambiense sleeping sickness in Sudan: cohort study. BMJ. 2008;336(7646):705–8. https://doi.org/10.1136/bmj.39485.592674.BE.
Franco JR, Simarro PP, Diarra A, Ruiz-Postigo JA, Samo M, Jannin JG. Monitoring the use of nifurtimox-eflornithine combination therapy (NECT) in the treatment of second stage gambiense human African trypanosomiasis. Res Rep Trop Med. 2012;3:93–101. https://doi.org/10.2147/RRTM.S34399.
Na-Bangchang K, Doua F, Konsil J, Hanpitakpong W, Kamanikom B, Kuzoe F. The pharmacokinetics of eflornithine (alpha-difluoromethylornithine) in patients with late-stage T.b. gambiense sleeping sickness. Eur J Clin Pharmacol. 2004;60(4):269–78. https://doi.org/10.1007/s00228-004-0759-7.
Boeckmann AJ, Sheiner LB, Beal SL. NONMEM Users Guide. Ellicott City, MD, USA: Icon Development Solutions; 1989-2009.
Lindbom L, Pihlgren P, Jonsson EN. PsN-Toolkit - A collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Prog Biomed. 2005;79(3):241–57. https://doi.org/10.1016/j.cmpb.2005.04.005.
Jonsson EN, Karlsson MO. Xpose - an S-PLUS based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput Methods Prog Biomed. 1999;58(1):51–64. https://doi.org/10.1016/s0169-2607(98)00067-4.
Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst Pharmacol. 2013;2:e50. https://doi.org/10.1038/psp.2013.24.
Holford N. A time to event tutorial for pharmacometricians. CPT Pharmacometrics Syst Pharmacol. 2013;2:e43. https://doi.org/10.1038/psp.2013.18.
Boberg M. Data on in vitro effects of eflornithine against trypanosoma parasites [Internet]. University of Gothenburg; 2021. Available from: https://doi.org/10.5878/1b50-ab56, Accessed Jan 7, 2022.
Yates JW, Ashton S, Cross D, Mellor MJ, Powell SJ, Ballard P. Irreversible inhibition of egfr: modeling the combined pharmacokinetic-pharmacodynamic relationship of osimertinib and its active metabolite AZ5104. Mol Cancer Ther. 2016;15(10):2378–87. https://doi.org/10.1158/1535-7163.MCT-16-0142.
Tuk B, van Oostenbruggen MF, Herben VM, Mandema JW, Danhof M. Characterization of the pharmacodynamic interaction between parent drug and active metabolite in vivo: midazolam and alpha-OH-midazolam. J Pharmacol Exp Ther. 1999;289(2):1067–74.
Raz B, Iten M, Grether-Buhler Y, Kaminsky R, Brun R. The Alamar Blue assay to determine drug sensitivity of African trypanosomes (T.b. rhodesiense and T.b. gambiense) in vitro. Acta Trop. 1997;68(2):139–47.
Pepin J, Khonde N, Maiso F, Doua F, Jaffar S, Ngampo S, et al. Short-course eflornithine in Gambian trypanosomiasis: a multicentre randomized controlled trial. Bull World Health Organ. 2000;78(11):1284–95.
Milord F, Loko L, Ethier L, Mpia B, Pepin J. Eflornithine concentrations in serum and cerebrospinal fluid of 63 patients treated for Trypanosoma brucei gambiense sleeping sickness. Trans R Soc Trop Med Hyg. 1993;87(4):473–7.
Van Nieuwenhove S, Schechter PJ, Declercq J, Bone G, Burke J, Sjoerdsma A. Treatment of gambiense sleeping sickness in the Sudan with oral DFMO (DL-alpha-difluoromethylornithine), an inhibitor of ornithine decarboxylase; first field trial. Trans R Soc Trop Med Hyg. 1985;79(5):692–8.
Abeloff MD, Slavik M, Luk GD, Griffin CA, Hermann J, Blanc O, Sjoerdsma A, Baylin SB. Phase I trial and pharmacokinetic studies of alpha-difluoromethylornithine--an inhibitor of polyamine biosynthesis. J Clin Oncol. 1984;2(2):124–30. https://doi.org/10.1200/JCO.1984.2.2.124.
Doua F, Boa FY, Schechter PJ, Miezan TW, Diai D, Sanon SR, et al. Treatment of human late stage gambiense trypanosomiasis with alpha-difluoromethylornithine (eflornithine): efficacy and tolerance in 14 cases in Cote d'Ivoire. Am J Trop Med Hyg. 1987;37(3):525–33.
De Koning HP. The drugs of sleeping sickness: their mechanisms of action and resistance, and a brief history. Trop Med Infect Dis. 2020;5(1). doi: https://doi.org/10.3390/tropicalmed5010014.
Yun O, Priotto G, Tong J, Flevaud L, Chappuis F. NECT is next: implementing the new drug combination therapy for Trypanosoma brucei gambiense sleeping sickness. PLoS Negl Trop Dis. 2010;4(5):e720. https://doi.org/10.1371/journal.pntd.0000720.
White NJ, Olliaro PL. Strategies for the prevention of antimalarial drug resistance: rationale for combination chemotherapy for malaria. Parasitol Today. 1996;12(10):399–401. https://doi.org/10.1016/0169-4758(96)10055-7.
Mesu V, Kalonji WM, Bardonneau C, Mordt OV, Blesson S, Simon F, et al. Oral fexinidazole for late-stage African Trypanosoma brucei gambiense trypanosomiasis: a pivotal multicentre, randomised, non-inferiority trial. Lancet. 2018;391(10116):144–54. https://doi.org/10.1016/S0140-6736(17)32758-7.
Lindner AK, Lejon V, Chappuis F, Seixas J, Kazumba L, Barrett MP, Mwamba E, Erphas O, Akl EA, Villanueva G, Bergman H, Simarro P, Kadima Ebeja A, Priotto G, Franco JR. New WHO guidelines for treatment of gambiense human African trypanosomiasis including fexinidazole: substantial changes for clinical practice. Lancet Infect Dis. 2019;20:e38–46. https://doi.org/10.1016/S1473-3099(19)30612-7.
Dickie EA, Giordani F, Gould MK, Maser P, Burri C, Mottram JC, et al. New drugs for human African Trypanosomiasis: a twenty first century success story. Trop Med Infect Dis. 2020;5(1). https://doi.org/10.3390/tropicalmed5010029.
Acknowledgements
The authors would like to acknowledge Professor Jose Ramon Franco, Department of Control and Neglected Tropical Disease, World Health Organization, for kind provision of event time points in the NECT study.
Funding
The Swedish Research Council (2016-05780) funded the project. Joel Tarning is funded by the Wellcome Trust (220211).
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work: C.A., M.B., J.T, A.A., M.A., R.J.L.
Drafting the work or revising it critically for important intellectual content: C.A., M.B., J.T, A.A., M.A., R.J.L.
Final approval of the version to be published: C.A., M.B., J.T, A.A., M.A., R.J.L.
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: C.A., M.B., J.T, A.A., M.A., R.J.L.
Corresponding author
Ethics declarations
Conflict of Interest
Although co-author C.A. and R.J.L. are employed by AstraZeneca R&D in Gothenburg, Sweden, AstraZeneca had no influence over the study. The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 117 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amilon, C., Boberg, M., Tarning, J. et al. Population Pharmacodynamic Modeling of Eflornithine-Based Treatments Against Late-Stage Gambiense Human African Trypanosomiasis and Efficacy Predictions of L-eflornithine-Based Therapy. AAPS J 24, 48 (2022). https://doi.org/10.1208/s12248-022-00693-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-022-00693-2