Abstract
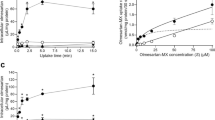
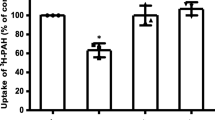
Organic anion transporter 3 (OAT3) plays an important role in the disposition of various anionic drugs which impacts the pharmacokinetics and pharmacodynamics of the therapeutics, thus influencing the pharmacological effects and toxicity of the drugs. In this study, we investigated the effect of insulin on the regulation of OAT3 function, expression, and SUMOylation. We demonstrated that insulin induced an increase in OAT3 transport activity through a dose- and time-dependent manner in COS-7 cells. The insulin-induced elevation in OAT3 function was blocked by PKA inhibitor H89, which correlated well with OAT3 protein expression. Moreover, both PKA activator Bt2-cAMP-induced increase and insulin-induced increase in OAT3 function were blocked by PKB inhibitor AKTi1/2. To further investigate the involvement of SUMOylation, we treated OAT3-expressing cells with insulin in presence or absence of H89 or AKTi1/2 followed by examining OAT3 SUMOylation. We showed that insulin enhanced OAT3 SUMOylation, and such enhancement was abrogated by H89 and AKTi1/2. Lastly, insulin increased OAT3 function and SUMOylation in rat kidney slice. In conclusion, our investigations demonstrated that insulin regulated OAT3 function, expression, and SUMOylation through PKA/PKB signaling pathway.

Graphical abstract









Similar content being viewed by others
References
You G. Structure, function, and regulation of renal organic anion transporters. Med Res Rev. 2002;22(6):602–16. https://doi.org/10.1002/med.10019.
Dantzler WH, Wright SH. The molecular and cellular physiology of basolateral organic anion transport in mammalian renal tubules. Biochim Biophys Acta. 2003;1618(2):185–93. https://doi.org/10.1016/j.bbamem.2003.08.015.
Srimaroeng C, Perry JL, Pritchard JB. Physiology, structure, and regulation of the cloned organic anion transporters. Xenobiotica. 2008;38(7-8):889–935. https://doi.org/10.1080/00498250801927435.
VanWert AL, Gionfriddo MR, Sweet DH. Organic anion transporters: discovery, pharmacology, regulation and roles in pathophysiology. Biopharm Drug Dispos. 2010;31(1):1–71. https://doi.org/10.1002/bdd.693.
Ahn SY, Nigam SK. Toward a systems level understanding of organic anion and other multispecific drug transporters: a remote sensing and signaling hypothesis. Mol Pharmacol. 2009;76(3):481–90. https://doi.org/10.1124/mol.109.056564.
Wang L, Sweet DH. Renal organic anion transporters (SLC22 family): expression, regulation, roles in toxicity, and impact on injury and disease. AAPS J. 2013;15(1):53–69. https://doi.org/10.1208/s12248-012-9413-y.
Zhang J, Wang H, Fan Y, Yu Z, You G. Regulation of organic anion transporters: role in physiology, pathophysiology, and drug elimination. Pharmacol Ther. 2020;217:107647. https://doi.org/10.1016/j.pharmthera.2020.107647.
Terada T, Inui K. Gene expression and regulation of drug transporters in the intestine and kidney. Biochem Pharmacol. 2007;73(3):440–9. https://doi.org/10.1016/j.bcp.2006.10.010.
Gareau JR, Lima CD. The SUMO pathway: emerging mechanisms that shape specificity, conjugation and recognition. Nat Rev Mol Cell Biol. 2010;11(12):861–71. doi: nrm3011 [pii]. https://doi.org/10.1038/nrm3011.
Gill G. SUMO and ubiquitin in the nucleus: different functions, similar mechanisms? Genes Dev. 2004;18(17):2046–59. https://doi.org/10.1101/gad.1214604.
Ulrich HD. The fast-growing business of SUMO chains. Mol Cell. 2008;32(3):301–5. https://doi.org/10.1016/j.molcel.2008.10.010.
Yang Y, He Y, Wang X, Liang Z, He G, Zhang P, et al. Protein SUMOylation modification and its associations with disease. Open Biol. 2017;7(10):170167. https://doi.org/10.1098/rsob.170167.
Wang H, Zhang J, You G. Activation of protein kinase A stimulates SUMOylation, expression, and transport activity of organic anion transporter 3. AAPS J. 2019;21(2):30. https://doi.org/10.1208/s12248-019-0303-4.
Karnieli E, Zarnowski MJ, Hissin PJ, Simpson IA, Salans LB, Cushman SW. Insulin-stimulated translocation of glucose transport systems in the isolated rat adipose cell. Time course, reversal, insulin concentration dependency, and relationship to glucose transport activity. J Biol Chem. 1981;256(10):4772–7.
Kono T, Suzuki K, Dansey LE, Robinson FW, Blevins TL. Energy-dependent and protein synthesis-independent recycling of the insulin-sensitive glucose transport mechanism in fat cells. J Biol Chem. 1981;256(12):6400–7.
Proud CG. Regulation of protein synthesis by insulin. Biochem Soc Trans. 2006;34(Pt 2):213–6. https://doi.org/10.1042/BST20060213.
Guo S. Insulin signaling, resistance, and the metabolic syndrome: insights from mouse models into disease mechanisms. J Endocrinol. 2014;220(2):T1–T23. https://doi.org/10.1530/JOE-13-0327.
Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol. 2019;234(6):8152–61. https://doi.org/10.1002/jcp.27603.
Chausmer AB. Zinc, insulin and diabetes. J Am Coll Nutr. 1998;17(2):109–15. https://doi.org/10.1080/07315724.1998.10718735.
Baumgard LH, Hausman GJ, Sanz Fernandez MV. Insulin: pancreatic secretion and adipocyte regulation. Domest Anim Endocrinol. 2016;54:76–84. https://doi.org/10.1016/j.domaniend.2015.07.001.
Reidy K, Kang HM, Hostetter T, Susztak K. Molecular mechanisms of diabetic kidney disease. J Clin Invest. 2014;124(6):2333–40. https://doi.org/10.1172/JCI72271.
Lungkaphina A, Arjinajarna P, Srimaroenga C, Chatsudthipong V. Function and expression of renal organic anion transporters in experimental diabetes in mice. ScienceAsia. 2012;38:18–23. https://doi.org/10.2306/scienceasia1513-1874.2012.38.018.
Tokarz VL, MacDonald PE, Klip A. The cell biology of systemic insulin function. J Cell Biol. 2018;217(7):2273–89. https://doi.org/10.1083/jcb.201802095.
Pelis RM, Wright SH. Renal transport of organic anions and cations. Compr Physiol. 2011;1(4):1795–835. https://doi.org/10.1002/cphy.c100084.
Barros SA, Srimaroeng C, Perry JL, Walden R, Dembla-Rajpal N, Sweet DH, et al. Activation of protein kinase Czeta increases OAT1 (SLC22A6)- and OAT3 (SLC22A8)-mediated transport. J Biol Chem. 2009;284(5):2672–9. https://doi.org/10.1074/jbc.M808078200.
Lungkaphin A, Arjinajarn P, Pongchaidecha A, Srimaroeng C, Chatsudthipong L, Chatsudthipong V. Impaired insulin signaling affects renal organic anion transporter 3 (Oat3) function in streptozotocin-induced diabetic rats. PLoS One. 2014;9(5):e96236. https://doi.org/10.1371/journal.pone.0096236.
Filippa N, Sable CL, Filloux C, Hemmings B, Van Obberghen E. Mechanism of protein kinase B activation by cyclic AMP-dependent protein kinase. Mol Cell Biol. 1999;19(7):4989–5000. https://doi.org/10.1128/mcb.19.7.4989.
Anzai N, Kanai Y, Endou H. Organic anion transporter family: current knowledge. J Pharmacol Sci. 2006;100(5):411–26. https://doi.org/10.1254/jphs.crj06006x.
Duan P, Li S, You G. Angiotensin II inhibits activity of human organic anion transporter 3 through activation of protein kinase Calpha: accelerating endocytosis of the transporter. Eur J Pharmacol. 2010;627(1-3):49–55. https://doi.org/10.1016/j.ejphar.2009.10.048.
Segawa H, Kaneko I, Takahashi A, Kuwahata M, Ito M, Ohkido I, et al. Growth-related renal type II Na/Pi cotransporter. J Biol Chem. 2002;277(22):19665–72. https://doi.org/10.1074/jbc.M200943200.
Bhardwaj RK, Herrera-Ruiz D, Eltoukhy N, Saad M, Knipp GT. The functional evaluation of human peptide/histidine transporter 1 (hPHT1) in transiently transfected COS-7 cells. Eur J Pharm Sci. 2006;27(5):533–42. https://doi.org/10.1016/j.ejps.2005.09.014.
Goyal S, Vanden Heuvel G, Aronson PS. Renal expression of novel Na+/H+ exchanger isoform NHE8. Am J Physiol Renal Physiol. 2003;284(3):F467–73. https://doi.org/10.1152/ajprenal.00352.2002.
Nigam SK, Bush KT, Martovetsky G, Ahn SY, Liu HC, Richard E, et al. The organic anion transporter (OAT) family: a systems biology perspective. Physiol Rev. 2015;95(1):83–123. https://doi.org/10.1152/physrev.00025.2013.
Nigam SK. The SLC22 transporter family: a paradigm for the impact of drug transporters on metabolic pathways, signaling, and disease. Annu Rev Pharmacol Toxicol. 2018;58:663–87. https://doi.org/10.1146/annurev-pharmtox-010617-052713.
Lee IH, Dinudom A, Sanchez-Perez A, Kumar S, Cook DI. Akt mediates the effect of insulin on epithelial sodium channels by inhibiting Nedd4-2. J Biol Chem. 2007;282(41):29866–73. https://doi.org/10.1074/jbc.M701923200.
Klisic J, Hu MC, Nief V, Reyes L, Fuster D, Moe OW, et al. Insulin activates Na(+)/H(+) exchanger 3: biphasic response and glucocorticoid dependence. Am J Physiol Renal Physiol. 2002;283(3):F532–9. https://doi.org/10.1152/ajprenal.00365.2001.
Toyoki D, Shibata S, Kuribayashi-Okuma E, Xu N, Ishizawa K, Hosoyamada M, et al. Insulin stimulates uric acid reabsorption via regulating urate transporter 1 and ATP-binding cassette subfamily G member 2. Am J Physiol Renal Physiol. 2017;313(3):F826–F34. https://doi.org/10.1152/ajprenal.00012.2017.
Chang CC, Tung CH, Chen CW, Tu CH, Chu YW. SUMOgo: prediction of sumoylation sites on lysines by motif screening models and the effects of various post-translational modifications. Sci Rep. 2018;8(1):15512. https://doi.org/10.1038/s41598-018-33951-5.
Matic I, Schimmel J, Hendriks IA, van Santen MA, van de Rijke F, van Dam H, et al. Site-specific identification of SUMO-2 targets in cells reveals an inverted SUMOylation motif and a hydrophobic cluster SUMOylation motif. Mol Cell. 2010;39(4):641–52. https://doi.org/10.1016/j.molcel.2010.07.026.
Acknowledgments
This work was supported by grants (to Dr. Guofeng You) from National Institute of General Medical Sciences (R01-GM079123 and R01-GM097000).
We would like to thank Dr. Kexin Liu and his group from Provincial Key Laboratory for Pharmacokinetics and Transport, Liaoning Dalian Medical University for their technical help on kidney slice preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that there is no conflict of interest.
Additional information
Guest Editors: Diane Burgess, Marilyn Morris and Meena Subramanyam
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 67 kb)
Rights and permissions
About this article
Cite this article
Zhang, J., You, G. Peptide Hormone Insulin Regulates Function, Expression, and SUMOylation of Organic Anion Transporter 3. AAPS J 23, 41 (2021). https://doi.org/10.1208/s12248-021-00575-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-021-00575-z