ABSTRACT
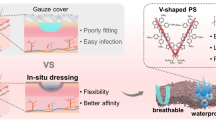
One approach in wound dressing development is to incorporate active molecules or drugs in the dressing. In order to reduce the frequency of dressing changes as well as to prolong wound healing efficacy, wound dressings that can sustain the release of the active molecules should be developed. In our previous work, we developed chitosan/sericin (CH/SS) microspheres that released sericin in a controlled rate. However, the difficulty of applying the microspheres that easily diffuse and quickly degrade onto the wound was its limitations. In this study, we aimed to develop wound dressing materials which are easier to apply and to provide extended release of sericin. Different amounts of CH/SS microspheres were embedded into various compositions of polyvinyl alcohol/gelatin (PVA/G) scaffolds and fabricated using freeze-drying and glutaraldehyde crosslinking techniques. The obtained CH/SS microspheres-embedded scaffolds with appropriate design and formulation were introduced as a wound dressing material. Sericin was released from the microspheres and the scaffolds in a sustained manner. Furthermore, an optimized formation of the microspheres-embedded scaffolds (2PVA2G+2CHSS) was shown to possess an effective antimicrobial activity against both gram-positive and gram-negative bacteria. These microspheres-embedded scaffolds were not toxic to L929 mouse fibroblast cells, and they did not irritate the tissue when applied to the wound. Finally, probably by the sustained release of sericin, these microspheres-embedded scaffolds could promote wound healing as well as or slightly better than a clinically used wound dressing (Allevyn®) in a mouse model. The antimicrobial CH/SS microspheres-embedded PVA/G scaffolds with sustained release of sericin would appear to be a promising candidate for wound dressing application.








Similar content being viewed by others
REFERENCES
Hasatsri S, Yamdech R, Chanvorachote P, Aramwit P. Physical and biological assessments of the innovative bilayered wound dressing made of silk and gelatin for clinical applications. J Biomater Appl. 2015;29:1304–13.
Aramwit P, Ratanavaraporn J, Siritientong T. Improvement of physical and wound adhesion properties of silk sericin and polyvinyl alcohol dressing using glycerin. Adv Skin Wound Care. 2015;28:358Y67.
Saarai A, Kasparkova V, Sedlacek AT, Saha P. On the development and characterization of crosslinked sodium alginate/gelatin hydrogels. J Mech Behav Biomed Mater. 2013;18:152–66.
Kuijpers AJ, Engbers GHM, Krijgsveld J, Zaat SAJ, Dankert J, Feijen J. Crosslinkingand characterization of gelatin matrices for biomedical applications. J Biomater Sci Polym Ed. 2000;11:225–43.
Juang JH, Bonner WS, Ogawa YJ, Vacanti P, Weir GC. Outcome of subcutaneous islet transplantation improved by polymer device. Transplantation. 1996;61:1557–61.
Chen DH, Leu JC, Huang TC. Transport and hydrolysis of urea in a reactor–separator combining an anion exchangemembrane and immobilized urease. J Chem Technol Biotechnol. 1994;61:351–7.
Yang M, Shuai Y, Zhou G, Mandal N, Zhu L, Mao C. Tuning molecular weights of Bombyx mori (B. mori) silk sericin to modify its assembly structures and materials formation. ACS Appl Mater Interfaces. 2014;6:13782–9.
Zhang YQ. Applications of natural silk protein sericin in biomaterials. Biotechnol Adv. 2002;20:91–100.
Zhaorigetu S, Yanaka N, Sasaki M, Watanabe H, Kato N. Inhibitory effects of silk protein, sericin on UVB-induced acute damage and tumor promotion by reducing oxidative stress in the skin of hairless mouse. J Photochem Photobiol B. 2003;71:11–7.
Dash R, Mandal M, Ghosh SK, Kundu SC. Silk sericin protein of tropical tasar silkworm inhibits UVB-induced apoptosis in human skin keratinocytes. Mol Cell Biochem. 2008;311:111–9.
Tsubouchi K, Igarashi Y, Takasu Y, Yamada H. Sericin enhances attachment of cultured human skin fibroblasts. Biosci Biotechnol Biochem. 2005;69:403–5.
Aramwit P, Kanokpanont S, De-Eknamkul W, Kamei K, Srichana T. The effect of sericin with variable amino-acid content from different silk strains on the production of collagen and nitric oxide. J Biomater Sci Polym Ed. 2009;20:1295–306.
Aramwit P, Kanokpanont S, Nakpheng T, Srichana T. The effect of sericin from various extraction methods on cell viability and collagen production. Int J Mol Sci. 2010;11:2200–11.
Aramwit P, Sangcakul A. The effects of sericin cream on wound healing in rats. Biosci Biotechnol Biochem. 2007;712473–7.
Aramwit P, Siritienthong T, Srichana T, Ratanavaraporn J. Accelerated healing of full-thickness wounds by genipin-crosslinked silk sericin/PVA scaffolds. Cells Tissues Organs. 2013;197:224–38.
Siritienthong T, Angspatt A, Ratanavaraporn J, Aramwit P. Clinical potential of a silk sericin-releasing bioactive wound dressing for the treatment of split-thickness skin graft donor sites. Pharm Res. 2014;31:104–16.
Siritienthong T, Ratanavaraporn J, Aramwit P. Development of ethyl alcohol-precipitated silk sericin/polyvinyl alcohol scaffolds for accelerated healing of full-thickness wounds. Int J Pharm. 2012;439:175–86.
Siritienthong T, Ratanavaraporn J, Srichana T, Aramwit P. Preliminary characterization of genipin-cross-linked silk sericin/poly(vinyl alcohol) films as two-dimensional wound dressings for the healing of superficial wounds. Biomed Res Int. 2013;Article ID 904314.
Aramwit P, Ekasit S, Yamdech R. The development of non-toxic ionic-crosslinked chitosan-based microspheres as carriers for the controlled release of silk sericin. Biomed Microdevices. 2015;17:9991.
Rabea EI, Badawy ME, Stevens CV, Smagghe G, Steurbaut W. Chitosan as antimicrobial agent: applications and mode of action. Biomacromolecules. 2003;4:1457–65.
Goy RC, Britto D, Assis OBG. A review of the antimicrobial activity of chitosan. Polímeros: Ciência e Tecnologia. 2009;19:241–7.
Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65:55–6.
Huang X, Brazel CS. On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Release. 2001;73:121–36.
Kang HW, Tabata Y, Ikada Y. Fabrication of porous gelatin scaffolds for tissue engineering. Biomaterials. 1999;20:1339–44.
Vartiainen J, Harlin A. Crosslinking as an efficient tool for decreasing moisture sensitivity of biobased nanocomposite films. Mater Sci Appl. 2011;2:346–54.
Komsa-Penkova RS, Rashap RK, Yomtova VM. Advantages of orange-labelled collagen and gelatine as substrates for rapid collagenase activity measurement. J Biochem Biophys Methods. 1997;34:237–49.
Ratanavaraporn J, Furuya H, Kohara H, Tabata Y. Synergistic effects of the dual release of stromal cell-derived factor-1 and bonemorphogenetic protein-2 from hydrogels on bone regeneration. Biomaterials. 2011;32:2797–811.
Lischer S, Körner E, Balazs DJ, Shen D, Wick P, Grieder K, et al. Antibacterial burst-release from minimal Ag-containing plasma polymer coatings. J R Soc Interface. 2011;8:1019–30.
Ong SY, Wu J, Moochhala SM, Tan MH, Lu J. Development of a chitosan-based wound dressing with improved hemostatic and antimicrobial properties. Biomaterials. 2008;29:4323–32.
Fouda MMG, Wittke R, Knittel D, Schollmeyer E. Use of chitosan/polyamine biopolymers based cotton as a model system to prepare antimicrobial wound dressing. Int J Diabetes Mellit. 2009;1:61–4.
Wittayasuporn M, Rengpipat S, Palaga T, Asawanonda P, Anumansirikul N, Wanichwecharungruang S. Chitosan derivative nanocarrier: safety evaluation, antibacterial property and ascorbylpalmitate encapsulation. J Microencapsul. 2010;27:218–25.
Helbig D, Bodendorf MO, Grunewald S, Kendler M, Simon JC, Paasch U. Immunohistochemical investigation of wound healing in response to fractional photothermolysis. J Biomed Opt. 2009;14:064044.
Tranquillo RT, Murray JD. Continuum model of fibroblast-driven wound contraction: inflammation-mediation. J Theor Biol. 1992;158:135–72.
ACKNOWLEDGMENTS
This research was supported by Chula Research Scholar from The Ratchadaphiseksomphot Endowment Fund, Chulalongkorn University (Contract number GCURS_58_07_33_01).
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editors: Otilia M. Koo, Panayiotis P. Constantinides, Lavinia M. Lewis, and Joseph Reo
Rights and permissions
About this article
Cite this article
Aramwit, P., Yamdech, R. & Ampawong, S. Controlled Release of Chitosan and Sericin from the Microspheres-Embedded Wound Dressing for the Prolonged Anti-microbial and Wound Healing Efficacy. AAPS J 18, 647–658 (2016). https://doi.org/10.1208/s12248-016-9897-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-016-9897-y