Abstract
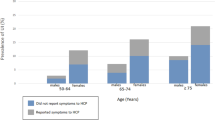
In the 1996 baseline surveysoftheAustralianLongitudinal StudyofWomen’s Health (ALSWH), 36.1% of mid-age women (45–50) and 35% of older women (70–75) reported leaking urine. This study aimed to investigate (a) the range of self-management strategies used to deal with urinary incontinence (UI); (b) the reasons why many women who report leaking urine do not seek help for UI; and (c) the types of health professionals consulted and treatment provided, and perceptions of satisfaction with these, among a sample of women in each age group who reported leaking urine “often” at baseline.
Five hundred participants were randomly selected from women in each of the mid-age and older cohorts of the ALSWH who had reported leaking urine “often” ina previous survey. Details about UI (frequency, severity, and situations), self-management behaviors and help-seeking for UI, types of health professional consulted, recommended treatment for the problem, and satisfaction with the service provided by health care professionals and the outcomes of recommended treatments were sought through a self-report mailed follow-up survey.
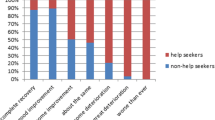
Most respondents had leaked urineinthe last month (94% and 91% of mid-age and older women, respectively), and 72.2% and 73.1% of mid-aged and older women, respectively, had sought help or advice about their UI. In both age groups, the likelihood of having sought help significantly increased with severity of incontinence. The most common reasons for not seeking help were that the women felt they could manage the problem themselves or they did not consider it to be a problem. Many women in both cohorts had employed avoidance techniques in an attempt to prevent leaking urine, including reducing their liquid consumption, going to the toilet “just in case,” and rushing to the toilet the minute they felt the need to.
Strategies are needed to inform women who experience UI of more effective management techniques and the possible health risks associated with commonly used avoidance behaviors. There may be a need to better publicize existing incontinence services and improve access to these services for women of all ages.
Similar content being viewed by others
References
AHCPR. (1996).Clinical practice guidelines on urinary incontinence in adults. Rockville, MD: American Agency for Healthcare Policy and Research (AHCPR). U.S. Department of Health and Human Services.
Bo, K., Talseth, T., & Holme, I. (1999). Single blind, randomized controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in the management of genuine stress incontinence in women.British Medical Journal, 318, 487–493.
Burgio, K. L., Ives, D. G., Locher, J. L., Arena, V. C., & Kuller, L. H. (1994). Treatment seeking for urinary incontinence in older adults.Journal of American Geriatric Society, 42, 208–212.
Cammu, H., Van Nylen, M., & Amy, J. J. (2000). A 10-year follow-up after Kegel pelvic floor muscle exercises for genuine stress incontinence.British Journal of Urology International, 85, 655–658.
Chiarelli, P., & Brown, W. J. (1999). Leaking urine in Australian women: prevalence and associated conditions.Women & Health, 29, 1–13.
Chiarelli, P., & Cockburn, J. (1999). The development of a physiotherapy continence promotion program using a customer focus.Australian Journal of Physiotherapy, 45, 111–120.
Chiarelli, P., Murphy B., & Cockburn, J. (in press). Women’s knowledge, practices and intentions regarding correct pelvic floor exercises.Neurourology & Urodynamics.
Crist, T., Shingleton, H., & Koch, G. (1972). Stress Incontinence and the nulliparous patient.British Journal of Obstetric Gynecology, 40, 13–17.
Department of Primary Industries and Energy, Department of Human Services and Health. (1994).Rural, remote and metropolitan areas classification: 1991 census edition. Canberra: Australian Government Publishing Service.
Dugan, E., Roberts, C. P., Cohen, S. J., Preisser, J. S., Davis, C. C., Bland, D. R.,et al. (2001). Why older community-dwelling adults do not discuss urinary incontinence with their primary care physicians.Journal of American Geriatric Society, 49, 462.
Engberg, S. J., McDowell, B. J., Burgio, K. L., Watson, J. E., & Belle, S. (1995). Self-care behaviors of older women with urinary incontinence.Journal of Gerontology Nursing, 21(8), 7–14.
Flynn, L., Cell, P., & Luisi, E. (1994). Effectiveness of pelvic muscle exercises inreducing urge incontinence among community residing elders.Journal of Gerontological Nursing, 20, 23–27.
Gunthorpe, W., Brown, W., & Redman, S. (2000). The development and evaluation of an incontinence screening questionnaire for female primary care.Neurourology and Urodynamics, 19, 595–607.
Herzog, A. R., Fultz, N. H., Normolle, D. P., Brock, B. M., & Diokno, A. C. (1989). Methods used to manage urinary incontinence by older adults in the community.Journal of American Geriatrics Society, 37, 339–347.
Hilton, P. (1988). Urinary incontinence during sexual intercourse: A common but rarely volunteered problem.British Journal of Obstetric Gynaecology, 95, 377–380.
Johnson, T. M., Kincade, J. E., Bernard, S. L., Busby-Whitehead, J., & DeFriese, G. H. (2000). Self-care practices used by older men and women to manage urinary incontinence: Results from the national follow-up survey on self-care and aging.Journal of American Geriatrics Society, 48, 894–902.
Millard, R. J. (1985). The incidence of urinary incontinence in Australia: A demographic survey conducted in the Sydney area in 1983.Journal of Urology, 57, 98–99.
Millard, R. J. (1998). The prevalence of urinary incontinence in Australia: a demographic survey conducted in Sydney in 1983.Australian Continence Journal, 4(4), 92–99.
Miller, Y. D., Brown, W. J., Russell, A., & Chiarelli, P. (in press). Urinary incontinence across the lifespan.Neurourology and Urodynamics.
Norton, P. A., MacDonald, L. D., Sedgwick, P. M., & Stanton, S. L. (1988). Distress and delay associated with urinary incontinence, frequency and urgency in women.British Medical Journal, 297, 1187–1189.
Norwood, M. (1990). Detrusor instability and its treatment.Physiotherapy, 76, 439–445.
Pinnock, C. B., & Marshall, V. R. (1997). Troublesome lower urinary tract symptomsinthe community: A prevalence study.Medical Journal Association, 167, 72–75.
Sandvik, H., Hunskaar, S., Seim, A., Hermstad, R., Vanvik, A., & Bratt, H. (1993). Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey.Journal of Epidemiology and Community Health, 47, 497–499.
Sandvik, H., Hunskaar, S., Vanvik, A., Bratt, H., Seim, A., & Hermstad, R. (1995). Diagnostic classification of female urinary incontinence: An epidemiological survey corrected for validity.Journal of Clinical Epidemiology, 48, 339–343.
Skoner, M. M. (1994). Self-management of urinary incontinence among women 31 to 50 years of age.Rehabilitative Nursing, 19, 339–343.
Skoner, M. M., & Haylor, M. J. (1993). Managing incontinence: Women’s normalizing strategies.Health Care Women International, 14, 549–560.
Thomas, T., Plymat, K. R., Blannin, J., & Meade, T. (1980). Prevalence of urinary incontinence.British Medical Journal, 281, 1243–1245.
Wall, L., Norton, P. A., & DeLancey, J. O. L. (1993). Surgical managementofstress incontinence.Practical Urogynecology, 153–190.
Wilson, P., Al-Samarrai, T., Deakin, M., Kolbe, E., & Brown, A. D. (1987). An objective assessment of physiotherapy for female genuine stress incontinence.British Journal of Obstetrics and Gynaecology, 94, 575–582.
Yarnell, J. W. G., Voyle, G. J., & Richardson, C. J. (1981). The prevalence and severity of urinary incontinence in women.Journal of Epidemiology and Community Health, 35, 71–74.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, Y.D., Brown, W.J., Smith, N. et al. Managing urinary incontinence across the lifespan. Int. J. Behav. Med. 10, 143–161 (2003). https://doi.org/10.1207/S15327558IJBM1002_04
Issue Date:
DOI: https://doi.org/10.1207/S15327558IJBM1002_04