Abstract
Introduction and hypothesis
Many women consider urinary incontinence (UI) a normal part of ageing. This belief may contribute to delays in treatment seeking. This study examined the relationship among holding that belief, UI type and severity, impact on quality of life, management and healthcare seeking in a sample of older community-dwelling Canadian women.
Methods
This was a secondary analysis of a controlled trial examining the impact of continence promotion workshops on UI self-management. All women who consented and provided baseline data were included in this analysis regardless of eligibility for the main study.
Results
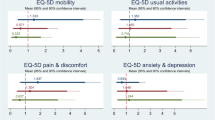
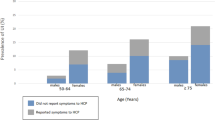
The sample included 4446 women (2022 with UI) of mean (SD) age 78.2 (9.0) years and BMI 26.6 (5.6). The belief that UI is normal for ageing was held by 2149 women [48.3% (83.7% of 1798 incontinent women)] and was not associated with age [adjusted odds ratio (OR) (95% CI): 1.00 (0.99, 1.01), p = 0.72] or perception of overall health. Women with this belief had more impaired QoL compared with the women who felt UI was not normal for ageing [mean (SD) 83.9 (19.4) vs. 87.4 (18.6) (p < 0.01)]. This belief remained unaffected by daily UI and pad use up to 2/day.
Conclusions
More than two-thirds of women thought UI normal for ageing. This belief was not associated with age or perception of overall health. More severe incontinence and greater quantities of pad use did not make women less likely to hold this belief.
Similar content being viewed by others
References
Abrams P, et al. The standardisation of terminology in lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Urology. 2003;61(1):37–49.
Cooper J, et al. Prevalence of female urinary incontinence and its impact on quality of life in a cluster population in the United Kingdom (UK): a community survey. Prim Health Care Res Dev. 2015;16(4):377–82.
Smith AP. Female urinary incontinence and wellbeing: results from a multi-national survey. BMC Urol. 2016;16:22.
Kwak Y, Kwon H, Kim Y. Health-related quality of life and mental health in older women with urinary incontinence. Aging Ment Health. 2016;20(7):719–26.
Wan X, et al. Disease stigma and its mediating effect on the relationship between symptom severity and quality of life among community-dwelling women with stress urinary incontinence: a study from a Chinese city. J Clin Nurs. 2014;23(15-16):2170–9.
Omli R, et al. Urinary incontinence and risk of functional decline in older women: data from the Norwegian HUNT-study. BMC Geriatr. 2013;13:47.
Yazdany T, Bhatia N, Reina A. Association of depression and anxiety in underserved women with and without urinary incontinence. Female Pelvic Med Reconstr Surg. 2014;20(6):349–53.
Dugan E, et al. The association of depressive symptoms and urinary incontinence among older adults. J Am Geriatr Soc. 2000;48(4):413–6.
Thom DH, Haan MN, Van Den Eeden SK. Medically recognized urinary incontinence and risks of hospitalization, nursing home admission and mortality. Age Ageing. 1997;26(5):367–74.
Shaw C, et al. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18(1):48–52.
Sexton CC, et al. The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA, UK and Sweden: EpiLUTS. BJU Int. 2009;103(Suppl 3):12–23.
Horrocks S, et al. What prevents older people from seeking treatment for urinary incontinence? A qualitative exploration of barriers to the use of community continence services. Fam Pract. 2004;21(6):689–96.
Irwin DE, et al. Symptom bother and health care-seeking behavior among individuals with overactive bladder. Eur Urol. 2008;53(5):1029–37.
Perry S, et al. An epidemiological study to establish the prevalence of urinary symptoms and felt need in the community: the Leicestershire MRC incontinence study. Leicestershire MRC incontinence study team. J Public Health Med. 2000;22(3):427–34.
Herschorn S, et al. A population-based study of urinary symptoms and incontinence: the Canadian urinary bladder survey. BJU Int. 2008;101(1):52–8.
Tannenbaum C, et al. Continence across continents to upend stigma and dependency (CACTUS-D): study protocol for a cluster randomized controlled trial. Trials. 2015;16:565.
Patrick DL, Martin ML, Bushnell DM. The I-QOL: a quality of life instrument specific to persons with urinary incontinence: user’s manual and scoring diskette for United States version. Seattle: Health Research Associates, Inc.; 1999.
Brookes ST, et al. A scored form of the Bristol female lower urinary tract symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. 2004;191(1):73–82.
Wagner TH, et al. Quality of life of persons with urinary incontinence: development of a new measure. Urology. 1996;47(1):67–71 discussion 71-2.
Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Warmoth K, et al. Older adults’ perceptions of ageing and their health and functioning: a systematic review of observational studies. Psychol Health Med. 2016;21(5):531–50.
Andrews RM, et al. Positive aging expectations are associated with physical activity among urban-dwelling older adults. Gerontologist. 2017;57(suppl_2):S178–86.
Menkin JA, et al. Positive expectations regarding aging linked to more new friends in later life. J Gerontol B Psychol Sci Soc Sci. 2017;72(5):771–81.
Duffy OK, Iversen L, Hannaford PC. The impact and management of symptoms experienced at midlife: a community-based study of women in Northeast Scotland. BJOG. 2012;119(5):554–64.
Kinchen KS, et al. Factors associated with women's decisions to seek treatment for urinary incontinence. J Women's Health (Larchmt). 2003;12(7):687–98.
Acknowledgements
We thank Quazi Imaduddin Ibrahim for his assistance with the statistical analysis.
Funding
Funding provided by: Canadian Institutes of Health Research (CIHR), Alberta Innovates Health Solutions (AIHS) and Capital Health Endowed Research Funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Wagg has received funding from Astellas Pharma, Pfizer Corp., and Essity Heath & Hygiene AB for research, speaker honoraria and consultancy—none directly related to this paper.
Dr. Rajabali, Dr. Tannenbaum and Miss Shaw declare no financial conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abstract presentation
Annual Scientific Meeting of the International Continence Society, Florence, Italy, September 2017
Rights and permissions
About this article
Cite this article
Shaw, C., Rajabali, S., Tannenbaum, C. et al. Is the belief that urinary incontinence is normal for ageing related to older Canadian women’s experience of urinary incontinence?. Int Urogynecol J 30, 2157–2160 (2019). https://doi.org/10.1007/s00192-019-03906-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03906-z