Abstract
Context
Utilizing mobile apps to increase physical activity levels is now standard practice in cancer care. The study’s objective was to provide patients with precise physical activity recommendations and/or initiate self-directed exercise programs.
Methods
A multidisciplinary group directed the design procedure. We adhered to the self-determination approach,and accompanying behavior modification strategies, as well as international guidelines in the field of physical activity in cancer care. The design process was user-centered and involved three steps: Understanding the user and the context, conceptualization, and evaluation of the prototype. The testing was carried out by the beneficiaries, healthcare professionals, and two experts. Three criteria were evaluated in the designed solution: usability, quality, and potential for behavior change.
Results
The evaluation results of the designed solution showed good perception by both beneficiaries and healthcare professionals. The average system usability scale score was 90,6 (SD: 7.33) for beneficiaries, and 92.75 (SD: 3.83) for healthcare professionals. The first expert received a mean overall quality score of 4.51 on the mobile app rating scale, while the second received a score of 4.27. The results of the app behavior change scale gave the first expert a score of 17/21 and the second a score of 15/21.
Conclusion
Based on the criteria of usability, quality, and potential for behavior change, the designed app demonstrated positive results. This is a preliminary evaluation, which will be followed by additional, in-depth evaluations with larger sample sizes.
Similar content being viewed by others
Introduction
In 2018, an estimated 18.1 million people were diagnosed with cancer and 9.6 million died from the disease, making cancer the second-highest cause of death worldwide [1]. Despite advancements in cancer patient survival, the oncological approach alone is still insufficient to address the functional impact of cancer on cancer survivors. The safety and the positive effects of physical activity (PA) on the physical function and quality of life of patients appear to be supported by strong scientific evidence [2].
Despite the expanding awareness of the importance of physical activity (PA) in cancer care among healthcare professionals (HCPs) internationally [3,4,5,6,7] and nationally [8], cancer patients and survivors do not engage in sufficient PA [9,10,11,12]. Through strategies of encouragement and communication with their patients, HCPs can play a significant role in promoting PA [13, 14]. However, PA advice is limited by several barriers. There are HCPs-related barriers, patient-related barriers, and institutional barriers [15, 16].
Utilizing mobile apps to increase PA levels is now standard practice. A meta-analysis has demonstrated their short-term efficacy [17]. An increase in daily steps and a nonsignificant decrease in sedentary behavior have been demonstrated [18]. However, few PA apps adhere to WHO's recommendations [19]. A survey of oncology nurse specialists regarding the role of apps in cancer care revealed the impact of apps on PA’s access and the autonomy it affords cancer patients [20]. The literature on mobile apps for promoting PA in cancer care is growing. However, apps with a well-described design methodology are recent and mainly targeting women with breast cancer [21,22,23,24,25] or other specific cancers [26, 27].
This study describes the user-centered design process of a mobile app that facilitates the provision of PA advice and the initiation of physical exercise programs (PEP) based on international recommendations for cancer patients and survivors.
Materials and methods
Design procedural methods
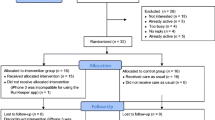
The design process is user-centered, which is viewed as a prerequisite for successful technological intervention [28, 29]. The process involves three phases of problem-solving: Understanding the user and the context; conceptualization and early prototyping; testing the prototype (Fig. 1).
Multidisciplinary team
A multidisciplinary team covering the various skills required to design a PA and PEP advice app for cancer patients and survivors. The design process was directed by a six-person team with the following areas of expertise: Sports medicine and adapted physical activity; Medical oncology; Physiotherapy and cardiorespiratory rehabilitation; and Bioinformatics.
Recruitment of participants and ethical considerations
The beneficiaries' recruitment was carried out by HE and BS, oncologist physicians. Participants met the following criteria:
-
for beneficiaries: Be a cancer patient or cancer survivor; Be at least 18 years old; Own and use a smartphone; Be able to read at least Arabic; Be willing to participate in the process of maintaining or enhancing the PA level.
-
for HCP: oncology-specializing HCP; smartphone ownership and use; regular contact with patients during and after oncology care; regular participation in therapeutic patient education.
HCPs were recruited from within institutions. Beneficiaries were solicited during doctor's visits. The Joint Ethics Committee of the Faculty of Medicine and Pharmacy at Mohammed V University in Rabat, Morocco, approved this investigation (November 2019; CRTN: 104/19). All participants gave informed consent before participation.
Conceptual models
We used self-determination theory [30] to facilitate long-term changes in PA-related behaviors. In order to accomplish this, we utilized the Coventry, Aberdeen, and London-Refined taxonomy, which has been characterized as an efficient, straightforward, and simple method for identifying the factors most likely to produce positive effects on PA behavior change [31]. In apps for PA promotion, several strategies for accompanying behavior change have been listed [32]. We have prioritized feedback, adaptation, goal-setting, and user targeting.
Step 1: understanding user and context
First, extensive research was conducted on the content of PA advice and suggested PEPs. Several international organizations in the United States, Australia, and Europe have developed general guidelines for combating sedentary lifestyles and physical inactivity, as well as guidelines for specific clinical contexts. PEP guidelines and modalities were developed based on available literature data, which determined the type of exercise, its frequency, intensity, duration, risks, and precautions [33,34,35,36,37,38,39]. Literature data was analyzed by HE and SB, oncologist physicians, and by HB, IBA, and YA, PA and sports physiotherapists. The data sheets were presented, discussed and validated by all work team.
In the second stage , participants underwent a semi-structured interview. For the beneficiaries, we determined their requirements and expectations regarding the app's features, as well as PA barriers. We searched for difficulties associated with therapeutic education in the field of PA prescription for HCPs. This interview was conducted by FE, nursing care manager; and YA, specialized PA physiotherapist.
Step 2: conceptualization
After the team had discussed the literature review on PA advice and PEP, we established decision-making algorithms. The process of validation was predicated on a team meeting, followed by a discussion. Objectives of the app's participation procedure, decision-making matrices, and the nature of the deliverables were the primary topics of discussion. YA designed the user participation pathway and algorithms according to the beneficiary's clinical and functional conditions.
The team based the design process for the mobile app's features on a brainstorming session.. Subsequently, it concluded by a validation of the mobile app's features according to needs and possibilities. The team then began designing the interfaces and deliverable document templates, while wireframes were created using the "Bootstrap 5.3 in Front-end, and Bootstrap smart admin in Back-end". JD, IT specialist, designed the wireframes and proposed several models for the mobile app; then the work team chose the graphic models.
Multiple trial tests (simulated cases) were conducted to ensure that the PA boards or PEPs adhered to the established decision algorithms. As a result of suggestions from team members, enhancements were implemented.
Step 3: evaluation of the prototype
User evaluation
The objective of this phase was for users, both beneficiaries and HCPs , to evaluate the app. Using the available audiovisual tutorials, participants were able to independently discover the app's functionalities following a concise explanation. In addition, participants were instructed to capture screenshots of any ambiguous information. Participants were instructed to utilize all of the app's features to obtain PA advice and/or PEPs. FE, nursing manager, was the administrator of interviews and instruments for recruited users.The user evaluation consisted of two instruments:
-
i.
The System usability Scale (SUS): As its name suggests, the SUS evaluates the usability of apps [40]. We utilized the Arabic version of the SUS scale, which demonstrates comparable levels of reliability, validity, and sensitivity to the original English SUS questionnaire [41]. The questionnaire contains ten questions used to assess the usability of a system swiftly and accurately. Each item is scored between one and five points (Strongly disagree: one point; Disagree: two points; Neutral: three points; Agree: four points; Strongly agree: five points). Higher scores indicate increased user-friendliness. The rating is computed as follows: X = Sum of points for questions with an odd number - 5; and Y = 25 - Sum of points for questions with an even number; then (X + Y) x 2.5 .The SUS score was interpreted using the Significance scale adapted by de Bangor, Kortum, and Miller (2009) [42]. The interpretation proposed is as follows: Excellent (if score > 80.3); Good (if score varies between 68 and 80.3); Acceptable (if score = 68); Poor (if SUS score varies between 51 and 68); Bad (if score 51).
-
ii.
Semi-directive interview: After the session, a semi-structured interview was conducted to address the following topics: (a) opinions on the app and its functionalities; (b) users' opinions on PEP and PA advice; and (c) missing elements and development opportunities if the app lacked something.
Expert evaluation
After perusing a document and audiovisual aids describing the app, two mobile app experts in design and usability conducted an evaluation based on the following instruments:
-
The Mobile App Rating Scale (MARS) evaluates mobile apps' overall quality [43]. The MARS scale consists of 23 items that are rated on a scale of 1 to 5 across four categories: engagement, functionality, aesthetics, and information. Each commodity is rated between "1" and "5" This score's metrological qualities are excellent [44]. We employed the validated Arabic version [45].
-
The App Behavior Change Scale (ABACUS) evaluates the likelihood of behavior change. The ABACUS scale, which consists of 21 items, was used to evaluate the app's potential for behavior change in terms of goal setting, action planning, obstacle identification, self-monitoring, and feedback. The ABACUS scale fills a void by standardizing the evaluation of a large number of health-related mobile apps [46].
Results
Step 1: understanding user and context
The results of the semi-structured interview outlined the socio-demographic and clinical characteristics (Tables 1 & 2). The participants in the design process were 24 beneficiaries and 11 HCPs. The beneficiary's mean age was 49, SD (14.27). As indicated by both HCPs and beneficiaries, there were no PEP recommendations. Smartphones, messaging, and social networks are significantly associated with the participants’ technology uses .
In Table 3, participants' requirements and expectations for the app, as well as barriers and enablers to participation in PEP, are outlined. Overall, participant expectations highlighted the significance of an easy-to-use solution, accessible and secure PA advice and PEPs, and care partner communication.
Step 2: conceptualization
This work's app is titled "Nachate Badani," which is the Arabic word for "PA" written in Latin script. It is a dynamic, open-source, web-based solution that is accessible to multiple stakeholders, including the patient, the healthcare provider, and the app manager. The app is available in Arabic and French, as well as smartphone, tablet, and computer varieties. The contents and functionalities of the app are explained via audiovisual tutorials. In Fig. 2, some screenshots of the app. Here is the link to the app: http://www.azemmouryouness.com/nachatbadani/
The app attempts to:
-
i.
The beneficiaries to receive specific PA advice regarding the improvement of their PA levels, or even the initiation and follow-up of a specific and individualized PEP.
-
ii.
The HCP should provide both general and specific PA advice, as well as specific, structured, accessible, and adapted PEPs.
-
iii.
For surveillance and evaluation purposes, the app manager must have access to certain clinical and functional data on the beneficiaries.
The design principles are:
-
i.
Ensure the safety of beneficiaries by, on the one hand, adhering to the applicable guidelines and, on the other hand, involving the accompanying physician.
-
ii.
Respect the self-determination approach and supporting behavior change strategies.
-
iii.
Promote the autonomy and empowerment of beneficiaries by requiring their participation in all phases of the process, including form entry, completion, monitoring, and evaluation of recommendations.
-
iv.
Respect evidence-based design guidelines when constructing PA boards and PEPs.
-
v.
Respect the inter-individual and environmental diversity of beneficiaries by describing PEPs that are accessible (without special apparatus or infrastructure) and require minimal functional skills.
-
vi.
Respect the basic principles of progression, dosage, and tolerance.
-
vii.
Respect the beneficiary's requirements and preferences.
The process and algorithms:Participation in the app begins with the HCP or beneficiary completing a form. The form includes fields (input) that serve as parameters for HCP advice and/or PEP (output). The beneficiary, the HCP, and/or the virtual coach conduct follow-up. The form contains two complementary sections: PA level assessment with the International Physical Activity Questionnaire, and Quality of life assessment with the SF12 questionnaire. Screenshots of the static portion of the app (a), the form (b), and the social connectivity/virtual coach (c) are displayed in Fig. 2. The HCP can receive a PEP during both the survival and post-treatment segments, while the beneficiary can only do so during the survival phase. As this necessitates close medical supervision and control, it has been decided that PEP will not be sent to beneficiaries in other phases of the treatment pathway or who are experiencing side effects. Therefore, we prefer to give specific PA advice according to the participant's clinical and functional condition only.
The eligibility for a PEP is contingent upon the absence of exercise-related risk and the possession of the bare minimum of required physical abilities. Every PEP recipient is entitled to general guidance on combating sedentary lifestyles and sustaining an active lifestyle. PEP is always accompanied by advice, especially in cases of lymphedema or abdominal hernia or risk of hernia. If the PEP entails potential risks, receiving specific PA guidance may be the only content provided (Fig. 3).
The suggested PEP comprises the following information (Fig. 4):
-
i.
Essential programs include aerobic exercise training and muscle strengthening. Beneficiaries at risk of abdominal hernia (abdominal surgery, stoma) are excluded from the "muscle strengthening" program. For gynecological malignancies, "pelvic floor exercises" is an essential program; otherwise, it is a supplementary program. The programs for "balance exercises" and "stretching exercises" are complementary.
-
ii.
Counsel in parallel: Read the section on receiving counsel.
-
iii.
Duration: six months for those in the survival phase and three months for those in the post-treatment phase.
-
iv.
Frequency per week: three times for adults and five times for the elderly.
Regarding the app's dependability, several case simulation tests were conducted to identify defects in the PA advice and the PEPs.
A chat space and a forum exist to facilitate communication between users with each other and with the virtual coach. The self-monitoring is daily, which consists in giving a feedback to the beneficiary according to the objectives of the day. Self-monitoring is carried out daily . The graphs and curves visible in the personal space and which reflect the data provided daily by the beneficiary. Some videos explain the app’s use, PA programs, and self-monitoring (Table 4).
The app's PA recommendations for beneficiaries varied according to their clinical and functional conditions. a dozen participants received a specific PA advice, seven received both specific and general PA advice, and five received only specific PA advice.
Step 3: evaluation of the prototype
Due to non-response or loss of sight, the number of users participating in the evaluation decreased from 24 to 18 for beneficiaries and from 11 to 10 for HCPs. The average SUS score for beneficiaries was 90,6 (SD: 7.33) and for HCPs, it was 92.75 (SD: 3.83). The obtained ratings are above the threshold for acceptability (above 68). Moreover, according to Bangor, Kortum, and Miller's (2009) verbal scale [47], the two scores obtained indicated that the usability of the app for both beneficiaries and HCPs would be categorized as outstanding (Table 5).
The results of the semi-structured interviews with app users revealed a generally favorable perception of the app. Users expressed satisfaction with both the app's usability and the PA advice and PEPs it generated. They did, however, observe the lack of reminder notifications, the limited selection of exercises, and the inability to integrate pedometers (Table 6).
The first expert received a mean overall quality score of 4.51 on the MARS scale, while the second expert received a score of 4.27 (Table 7). The results of the ABACUS scale gave the first expert a score of 17/21 and the second expert a score of 15/21 (Table 8). Overall, the results suggest that the designed app is of high quality and has the potential to alter behavior. However, the experts identified areas for enhancement, such as appealing to the desire for change.
Discussion
To our knowledge, this is the first mobile app developed on a national scale and adapted to the sociocultural and linguistic context of Morocco to promote PA in cancer care, and possibly in the care of all chronic diseases. This solution is a response to the expanding demand for developing mobile apps in the field of cancer in order to improve patient adherence while respecting cultural and linguistic requirements [47].
Participants reported some impediments to the utilization and promotion of PA in the oncology care pathway. These results appear to corroborate the barriers identified in a previous study of the same setting, namely the difficulties and lack of training for HCPs [8]. Nonetheless, the "E-health" initiative is viewed as a chance to improve the results of the healthcare system, given the high rate of connectivity among Moroccans compared to other African nations [48].
Evidence-based design is one of the developed solution's strengths. This characteristic is a requirement for mobile PA apps, but it is rarely respected [49]. In addition, adherence to the adaptation strategies retained in theoretical models appears to enhance the efficacy of PA-specific apps [50].
According to the obtained results, both experts and users approved and praised the functionality of the app. A higher level of persuasiveness in a mobile app promoting PA should be characterized by dependability, expertise, authority, third-party endorsement, and verifiability [21]. In addition, the app's appearance, which inspires science and professionalism [51], and provides access to credible information sources [27], contributes to its credibility .
Both experts highlighted the dearth of appeal of behavioral change motivation. However, the feedback provided by the HCP or virtual coach would help beneficiaries maintain their motivation. In fact, it appears that users who receive social feedback are more engaged with HCP recommendations [52]. However, users noted that our solution lacked reminder notifications. This feature appears to be a factor ensuring user compliance with the desired behavior [53]. In our app, however, we have emphasized visual aids, especially graphics. This permits the visualization of behavior modification [44]. Participants in the study who were HCPs recommended the incorporation of pedometers for the objective surveillance of PA. In fact, a meta-analysis revealed that the incorporation of a PA tracker could serve as a useful instrument for HCPs to provide ongoing monitoring and support [18]However, a faint correlation has been established between user evaluation and clinical utility [54], so positive user evaluation does not necessarily imply clinical utility. The evaluation of healthcare apps faces some obstacles, including the time required to complete the evaluation, the paucity of evidence-based data regarding evaluation instruments, and the inflexibility of the latter [55]. We believe that the devised solution also addresses these obstacles.
The methodology for designing mobile apps to promote PA in people with cancer has been described by several previous studies [21,22,23,24,25,26,27]. Compared to previous solutions, ours appears to be more global and comprehensive, as it is designed to assist HCPs in recommending PA and to assist patients in maintaining an adequate level of PA throughout the entire therapeutic pathway. The realities of the clinical context, which have demonstrated HCPs' lack of knowledge in this field [8], may justify these decisions. The absence of comparable experience in the context in which this app was developed was also a determining factor, as we sought to fill the void in this field to the best of our ability. The app's general nature is also reflected in its numerous and diverse recommendations, as it offers both PA advice and PEPs. The latter include all components, including exercise retraining, muscle strengthening, pelvic floor exercises, balance exercises, and flexibility exercises. In a study on the design of a mobile PA app, the authors acknowledged that the recommended PEP [22], lacked a resistance program (muscle conditioning).
Limitations
Due to the limited sample size, results obtained from users (beneficiaries and HCP) should be interpreted with caution. Although the results of the user evaluations are encouraging, they must be supported by a post-hoc evaluation of the program's long-term impact. The selection of beneficiaries based on the criteria of smartphone ownership and use brings into question the applicability of such a solution to all individuals who are dismayed by the oncology recommendation for PA. Despite the potential for mobile apps to improve access to e-health, there are some related issues: unequal access to mobile technology, lack of familiarity with or knowledge of how to use apps, and privacy and security concerns [47].
Conclusion
The design of the "NachateBadani" app based on a user-centered process was able to identify the specific PA recommendation requirements of cancer patients and survivors. We adhered to the pertinent guidelines, the self-determination approach of the beneficiaries, and the accompanying behavior change strategies. The objective was to improve the user-friendliness and acceptability of the tool, as well as the recipients' long-term commitment to the behavior change process. The outcomes of the evaluation of usability, quality, and behavior-change potential appear favorable. Also, the short-term impact on the volume and quality of beneficiaries' PA appears promising.
This is a preliminary evaluation, which will be followed by additional, in-depth evaluations with larger sample sizes. In the future, we intend to evaluate the solution's long-term impact, develop other, more specialized tools (such as those for breast cancer), and possibly expand the experiment to other chronic diseases.
Availability of data and materials
The anonymized data used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ABACUS:
-
The Application Behavior Change Scale
- MARS:
-
The Mobile Application Rating Scale
- HCP:
-
Healthcare Professional
- PA:
-
Physical Activity
- PEP:
-
Physical Exercise Program
- SUS:
-
The System Usability Scale
References
Bray F, Ferlay J, Soerjomataram I. Global Cancer Statistics 2018 : GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. 2018;394–424.
Segal R, Zwaal C, Green E, Tomasone JR, Loblaw A, Petrella T. Exercise for people with cancer : a clinical practice guideline. Curr Oncol. 2017;24(1):40–6.
Douglas F, Torrance N, Van Teijlingen E, Meloni S, Kerr A. Primary care staff’s views and experiences related to routinely advising patients about physical activity. A questionnaire survey. BMC Public Health. 2006;6(1):1–10.
Hardcastle SJ, Kane R, Chivers P, Hince D, Dean A, Higgs D, et al. Knowledge, attitudes, and practice of oncologists and oncology health care providers in promoting physical activity to cancer survivors: an international survey. Support Care Cancer. 2018;26(11):3711–9.
Sheill G, Guinan E, Neill LO, Hevey D, Hussey J. Physical activity and advanced cancer: the views of oncology and palliative care physicians in Ireland. Ir J Med Sci. 2018;187(2):337–42.
O’Hanlon E, Kennedy N. Exercise in cancer care in Ireland: a survey of oncology nurses and physiotherapists. Eur J Cancer Care (Engl). 2014;23(5):630–9.
Van Veen MR, Hoedjes M, Versteegen JJ, Van De Meulengraaf-Wilhelm N, Kampman E, Beijer S. Improving oncology nurses’ knowledge about nutrition and physical activity for cancer survivors. Oncol Nurs Forum. 2017;44(4):488–96.
Azemmour Y, Boutayeb S, Nafai S, Amine Souadka, Hind Mrabti, Ibrahim Elghissassi, Marfak A, Errihani H. Knowledge and views of physicians and nurses about physical activity advice in oncology care : a cross- sectional study. Pan Afr Med J. 2022;41(57):1–13.
Wong JN, EM, LT. Physical activity programming and counseling preferences among cancer survivors: a systematic review. Int J Behav Nutr Phys Act. 2018;15. https://doi.org/10.1200/JCO.2017.35.5_suppl.162.
Mcgowan EL, Speed-andrews AE, Blanchard CM, Rhodes RE, Friedenreich CM, Culos-reed SN, et al. Physical Activity Preferences Among a Population-Based Sample of Colorectal Cancer Survivors. Oncol Nurs Forum. 2013;40(1):44–52.
Errol J. Philip, Elliot J. Coups, Marc B. Feinstein, Bernard J. Park, Donna J. Wilson and JSO. Physical activity preferences of early-stage lung cancer survivors. Support Care Cancer. 2014;22(2):495–502.
Fassier P, Zelek L, Partula V, Srour B, Bachmann P, Touillaud M, et al. Variations of physical activity and sedentary behavior between before and after cancer diagnosis. 2016;0(June).
Jones LW, Courneya KS, Fairey AS, Mackey JR. Effects of an oncologist’s recommendation to exercise on self-reported exercise behavior in newly diagnosed breast cancer survivors: a single-blind, randomized controlled trial. Ann Behav Med. 2004;28(2):105–13.
Fisher A, Williams K, Beeken R, Wardle J. Recall of physical activity advice was associated with higher levels of physical activity in colorectal cancer patients. BMJ. 2015;5:e006853.
Smith-Turchyn J, Richardson J, Tozer R, McNeely M, Thabane L. Physical activity and breast cancer: a qualitative study on the barriers to and facilitators of exercise promotion from the perspective of health care professionals. Physiother Canada. 2016;68(4):383–90.
Azemmour Y, Boutayeb S, Beddaa H, Errihani H. Physical activity in cancer care: barriers and interventions. Pan Afr Med J. 2022;43:1–5.
Yerrakalva D, Yerrakalva D, Hajna S, Griffin S. Effects of Mobile Health App Interventions on Sedentary Time, Physical Activity, and Fitness in Older Adults: Systematic Review Corresponding Author. J Med INTERNET Res. 2019;21:1–13. https://doi.org/10.2196/14343.
Brickwood K, Hons B, Watson G, Brien JO, Williams AD. Consumer-based wearable activity trackers increase physical activity participation : systematic review and meta-analysis corresponding author : 2019;7(4):1–20.
Knight E, Stuckey MI, Prapavessis H, Petrella RJ. Public Health Guidelines for Physical Activity: Is There an App for That? A Review of Android and Apple App Stores. JMIR MHealth UHealth. 2015;3:1–9. https://doi.org/10.2196/mhealth.4003.
Roberts AL, Fishe HWWP, Stevens C, Lally P, Smith L, Abigail. Cancer specialist nurses ’ perspectives of physical activity promotion and the potential role of physical activity apps in cancer care. J Cancer Surviv. 2019;13:815–28.
Marcu G, Plank M, Leader A, Caro K, Barsevick A. Bounce: Designing a Physical Activity Intervention for Breast Cancer Survivors. PervasiveHealth. 2018. https://doi.org/10.1145/3240925.3240927.
Monteiro-guerra F, Signorelli GR, Tadas S, Zubiete ED. A personalized physical activity coaching app for breast cancer survivors : design process and early prototype testing corresponding author : JMIR mhealth uhealth. 2020;8(7):1–22.
Lee H, Uhm KE, Cheong IY, Yoo JS, Chung SH, Park YH. Patient Satisfaction with Mobile Health (mHealth) Application for Exercise Intervention in Breast Cancer Survivors. J Med Syst. 2018;42:1–9.
Economou D, Kounenis T, Bell N, Azimi T, Elliott B. PhytoCloud: A gamified Mobile Web Application to modulate diet and physical activity of women with breast cancer. IEEE Comput. Soc., EEE 30th International Symposium on Computer-Based Medical Systems; 2017. https://doi.org/10.1109/CBMS.2017.164.
Zhang X, Deng Z, Parvinzamir F, Dong F. MyHealthAvatar lifestyle management support for cancer patients. Ecancermedicalscience. 2018;12(849):1–17.
Fuemmeler BF, Holzwarth E, Sheng Y, Do EK, Miller CA, Blatt J, et al. Mila blooms : a mobile phone application and behavioral intervention for promoting physical activity and a healthy diet among adolescent survivors of childhood cancer. Games Health J. 2020;9(4):279–89.
Hong Y, Dahlke DV, Ory M, Hochhalter A, Purcell NP, Talwar D, et al. Designing iCanFit: A Mobile-Enabled Web Application to Promote Physical Activity for Older Cancer Survivors. JMIR Res Protoc. 2013;2:1–11. https://doi.org/10.2196/resprot.2440.
Ghulam S, Shah S, Robinson I, Alshawi S. Developing medical device technologies from users’ perspectives: A theoretical framework for involving users in the development process. Int J Technol Assess Health Care. 2009;25:514–21. https://doi.org/10.1017/S0266462309990328.
Abras C, Maloney-krichmar D, Preece J. User-Centered Design. 2004;1–14.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation. Soc Dev Well-Being. 2000;55(1):68–78.
Michie S, Ashford S, Sniehotta FF, Stephan U, Bishop A, French DP, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours : The CALO- RE taxonomy. 2011;0446.
Valerie DA, Hermens HJ. Tailoring real-time physical activity coaching systems : a literature survey and model. 2014;351–92.
Buffart LM, Galvão DA, Brug J, Chinapaw MJM, Newton RU. Evidence-based physical activity guidelines for cancer survivors : current guidelines, knowledge gaps and future research directions. Cancer Treat Rev. 2014;40(2):327–40. https://doi.org/10.1016/j.ctrv.2013.06.007.
Brown JK, Byers T, Doyle C, Courneya KS, Demark-Wahnefried W, Kushi LH, et al. Nutrition and physical activity during and after cancer treatment: an American cancer society guide for informed choices. CA Cancer J Clin. 2003;53(5):268–91.
Hayes SC, Spence RR, Galvão DA, Newton RU. Australian Association for Exercise and Sport Science position stand: optimising cancer outcomes through exercise. J Sci Med Sport. 2009;12:428–34.
Schmitz KH, Courneya KS, Matthews C, Galva DA, Pinto BM, Irwin ML et al. I. American College of Sports Medicine Roundtable on Exercise Guidelines for Cancer Survivors. Med Sci Sport Exerc Copyr 2010 by Am Coll Sport Med. 2010;0195-9131/. https://doi.org/10.1249/MSS.0b013e3181e0c112
Rock CL, Doyle ; Colleen, Demark-Wahnefried ; Wendy, Meyerhardt; ; Jeffrey, Courneya KS, Schwartz ; Anna L., et al. Nutrition and physical activity guidelines for cancer survivors. Ca Cancer J Clin. 2012;62:242-274.
Campbell A, Stevinson C, Crank H. The BASES Expert Statement on Exercise and Cancer Survivorship The BASES Expert Statement on Exercise and Cancer Survivorship. J Sports Sci. 2012;30:949–52. https://doi.org/10.1080/02640414.2012.671953.
Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, et al. American college of sports medicine roundtable report on physical activity. Sedent Behav Cancer Prev Control. 2019;2018(3):2391–402.
Brooke J. a “quick and dirty” Usability Scale. Jordan PW, Thomas B, Mcclell IL, Weerdmeester B, Ed Usability Eval Ind Boca Raton, Florida CRC Press. 1996;4–7.
Alghannam BA, Albustan SA, Al-hassan AA, Lamees A, Alghannam BA. Towards a standard Arabic system usability scale : psychometric evaluation using communication disorder app towards a standard arabic system usability scale : psychometric evaluation using communication disorder app. Int J Hum-Comput Interact. 2017;00(00):1–6. https://doi.org/10.1080/10447318.2017.1388099.
Bangor A, Staff T, Kortum P, Miller J, Staff T. Determining what individual sus scores mean: adding an adjective rating scale. J Usabil Stud. 2009;4(3):114–23.
Stoyanov SR, Psych M, Hides L, Kavanagh DJ, Zelenko O. Mobile App Rating Scale: A New Tool for Assessing the Quality of Health Mobile Apps. JMIR MHealth UHealth. 2015;3:1–9. https://doi.org/10.2196/mhealth.3422.
Terhorst Y, Philippi P, Sander LB, Schultchen D, Paganini S, Bardus M, et al. Validation of the Mobile Application Rating. PLoS One. 2020;1–14. https://doi.org/10.1371/journal.pone.0241480
Bardus M, Awada N, Ghandour LA, Fares E, Gherbal T, Al-zanati T, et al. The Arabic Version of the Mobile App Rating Scale: Development and Validation Study. JMIR MHealth UHealth. 2020;8:1–15. https://doi.org/10.2196/16956.
Mckay FH, Slykerman S, Dunn M. The App Behavior Change Scale: Creation of a Scale to Assess the Potential of Apps to Promote Behavior Change. JMIR MHealth UHealth. 2019;7:1–18. https://doi.org/10.2196/11130.
Kim H, Goldsmith J V, Sengupta S, Mahmood A, Powell MP, Bhatt J, et al. Mobile health application and e-health literacy : opportunities and concerns for cancer patients and caregivers. 2017.
Santé M de la. Livre blanc sur la e-santé au Maroc Livre blanc sur la e-santé au Maroc. 2021.
Kebede M, Steenbock B, Helmer SM, Sill J, Pischke CR. Identifying evidence-informed physical activity apps : content analysis corresponding author : 2018;6.
Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. 2008;23(3):454–66.
Chang T. What influences users ’ decisions to take apps into use ? A framework for evaluating persuasive and engaging design in mobile apps for well-being. 2012.
Ayubi SU, Parmanto B. PersonA : persuasive social network for physical activity. 2012;2153–7.
Lappalainen P, Langrial S. Web-based acceptance and commitment therapy for depressive symptoms with minimal support : a randomized controlled trial. 2015.
Singh K, Drouin K, Newmark LP, Lee J, Faxvaag A, Rozenblum R, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Aff. 2016.
Dawson RM, Felder TM, Donevant SB, Kane K, Card EB, Callie III, et al. What makes a good health ‘ app ’? Identifying the strengths and limitations of existing mobile application evaluation tools. 2019;(June):1–8.
Acknowledgements
We gratefully thank all study participants, patients, and healthcare professionals for taking part in this study. We gratefully thank the Translational Oncology Research Team and the Moroccan Association of Manual Therapy for their technical and administrative support.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YA, SB, and HE participated in the design of the study. JD was responsible for the IT aspect of the design. The original manuscript was drafted by YA and reviewed by all authors YA, SB, HB, IBA, HC, FE, and HE. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Joint Ethics Committee of the Faculty of Medicine and Pharmacy at Mohammed V University in Rabat, Morocco, approved this investigation (November 2019; CRTN: 104/19). All participants gave informed consent before participation.
Consent for publication
Not Applicable. Participants signed a consent form that informed them about the intention to publish the data from the study. In addition, no identifying or personal details are presented in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Azemmour, Y., Boutayeb, S., Elkhalloufi, F. et al. User-centered design of a mobile app for physical activity advice in cancer care: preliminary study in Morocco at the National Institute of Oncology. BMC Digit Health 2, 36 (2024). https://doi.org/10.1186/s44247-024-00093-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-024-00093-w