Abstract
Background
Cavernous hemangiomas are usually located in the liver, skin, and subcutaneous tissues. Although they can arise from any organ, cavernous hemangiomas rarely occur as a pulmonary tumor. We herein report a rare case of a pulmonary cavernous hemangioma that was surgically resected.
Case presentation
A woman in her 40s was found to have 2 well-defined nodules in the lower lobe of the left lung by computed tomography during following up of bladder cancer. She had a history of surgery for tetralogy of Fallot at 6 years old and pulmonary valve replacement for pulmonary valve insufficiency in her late 30s. She had also undergone surgery for bladder cancer. Although there was no accumulation of 18F-fluorodeoxyglucose on positron emission tomography (PET), the tumor slowly grows. Surgical resection was therefore performed to obtain a definitive diagnosis. The postoperative histological examination revealed an encapsulated nodule comprising large, dilated vessels lined with vascular endothelium and filled with blood, which led to the diagnosis of a pulmonary cavernous hemangioma.
Conclusion
We experienced a rare case of pulmonary cavernous hemangioma and reviewed the previous reports.
Similar content being viewed by others
Background
Cavernous hemangiomas are benign diseases composed of large, dilated vascular spaces lined by a single layer of endothelial cells and filled with blood [1, 2]. They are usually located in the liver, skin, and subcutaneous tissues [1]. Although they can arise from any organ, cavernous hemangiomas rarely occur as a pulmonary tumor [3,4,5]. A previous review of pulmonary cavernous hemangiomas (PCHs) found only 10 previously reported cases during the 60 years prior to 2010 [6]. Zhuang et al. also summarized 17 cases of PCH reported in the database of PubMed, Embase, and Web of Science from 1996 to 2017 [7].
While most PCHs are clinically benign, they can be difficult to differentiate from metastases when occurring in multiples in patients with malignancy [2]. Although cough and hemoptysis are the most common symptoms, asymptomatic patients have been reported. Furthermore, PCHs rarely but occasionally cause sudden death due to blood aspiration [8].
We experienced a rare case of PCHs during the follow-up of bladder cancer that was surgically resected. We further reviewed previous reports and summarize 43 total cases of PCH [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31], including our own, making this review the largest ever with regard to the number of patients involved.
Case presentation
A woman in her 40s consulted our department because of pulmonary nodules. She had been found to have lung nodules by computed tomography (CT) performed for a routine follow-up of bladder cancer. She had a history of surgery for tetralogy of Fallot at 6 years old and pulmonary valve replacement for pulmonary valve insufficiency in her late 30s. She had also undergone surgery for bladder cancer. She had no specific family history. She had been prescribed aspirin due to her history of surgery for pulmonary valve insufficiency.
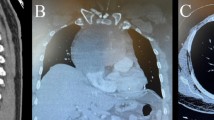
Chest X-ray showed a small nodular shadow in the left lower lung field (Fig. 1a). CT in the lung window setting showed abnormal nodules measuring 8 and 6 mm in the lower lobe of the left lung of segment 8 (Fig. 1b). These nodules were difficult to visualize under the mediastinal window setting. As a result, contrast-enhanced CT in the mediastinal window setting did not depict the pulmonary nodules nor had an enhanced effect. There was no accumulation of 18F-fluorodeoxyglucose (FDG) on positron emission tomography (PET) of the tumor (Fig. 1c). Because the nodules were small, were existing in a unilateral localized area, and showed no accumulation of FDG, they seemed benign. The attending physician therefore decided to follow them conservatively. However, after 3 years of follow-up, the nodules showed a slow growth. The patient was thus referred to our department for surgical resection to obtain a definitive diagnosis with differentiation from nontuberculous mycobacteria, metastatic lung tumor, and lung cancer.
a Chest X-ray findings: small nodular shadow (arrowhead) was observed in the left lower lung field. b Chest computed tomography findings: two well-demarcated solid nodules (arrowheads) were observed in the segment 8 region of the left lower lobe, 9 mm and 7 mm in diameter. c18F-fluorodeoxyglucose positron emission tomography (FDG-PET) findings: no accumulation was observed in pulmonary nodules (arrowheads) or other areas
Her clinical status was unremarkable, and she was thought to have enough surgical endurance. She had a surgical wound after median sternotomy and a systolic murmur at the left sternal border of the second to third intercostals. Laboratory examinations showed no remarkable changes, except for a slight elevation of brain natriuretic peptide (BNP) levels at 142 pg/mL. Tumor markers, including carcinoembryonic antigen (CEA), cytokeratin fragment (CYFRA) 21, and pro-gastrin-releasing peptide (Pro-GRP), were within the normal ranges. Cryptococcus neoformans antigen, aspergillus antigen, serum (1,3)-beat-d-glucan, and the T cell spot (T-SPOT) test were also negative. Soluble interleukin-2 receptor (sIL-2R) showed no elevation.
The multiple pulmonary nodules showed a slow growth and she had a surgical history of bladder cancer. We could not rule out that the metastases originated from bladder cancer. For that reason, we considered a biopsy of the pulmonary nodules, rather than follow them conservatively. But the nodules were small in diameter, existing in the peripheral of the left lower lobe. Therefore, a non-surgical biopsy such as transbronchial lung biopsy (TBLB) or CT-guided lung biopsy was thought to be difficult to make a definite diagnosis. With the preoperative diagnosis of a metastatic tumor originating from bladder cancer, we planned a surgical lung biopsy.
We performed wedge resection of the left lower lung, including the nodules, via three-port video-assisted thoracic surgery (VATS). During the operation, we confirmed a pulmonary nodule just below the pleura in S8 of the left lower lobe by palpation. In addition, we could also directly palpate the other deeper lesion inside the lung parenchyma.
After grasping the two nodules with ring-like grasping forceps to secure a sufficient surgical margin from the lesions, we resected the two pulmonary nodules in bulk with an autosuture device. After resection, we confirmed the sufficient margin from the deeper lesion by checking the cutting surface of the specimen.
Intraoperative histological examination showed the nodule consisted of spindle-shaped cells with oval nuclei and eosinophilic cytoplasm, forming cystic cavities abundantly. Intraoperative histological diagnosis was suspicious of lymphangiomyomatosis, obtained by examining one of the two nodules. The surgery time was 68 min, and the bleeding volume was small.
Gross findings of the resected specimen showed a well-demarcated nodule in the S8 peripheral part of the left lung (Fig. 2). Gross finding of the nodule used for intraoperative histological diagnosis is not presented because it was not stored. The resected two nodules had the same findings of histological examination. A histological examination revealed an encapsulated nodule comprising large, dilated vessels lined with endothelium and filled with blood (Fig. 3).
Macroscopic findings of the resected specimen. The cut surface of one of two resected nodules. The nodule used for intraoperative histological diagnosis is not presented because it was not stored. A well-demarcated nodular lesion (arrowhead) was found in the peripheral region of the resected specimen at the left lower lobe
Microscopic and immunohistochemical findings of the resected specimen. a Hematoxylin-eosin staining (low power field). The inside of a well-demarcated nodule consisted of the dilated vascular lumen with vascular endothelial cells and smooth muscle components. The vascular endothelial cells were histological findings of cavernous hemangioma, and no malignant features were observed. Although the smooth muscle proliferated, it did not surround the lumen of the vessel and was considered unlikely to be neoplastic. b–f Immunohistochemical staining (low power field) showed CD31- (b), CD34- (c), and von Willebrand factor (vVF)-positive endothelial cells (d) in the vascular lumen and α-smooth muscle actin-positive cells in the smooth muscle component (e). Elastic van Gieson (EVG) staining (f) showed irregular elastic fibers, and the distribution of elastic fibers was continuous in the surrounding lung tissue and hemangioma tissue, indicating that the smooth muscle cells did not form a neoplastic vessel wall. Based on the above findings, the lesion was considered to be pulmonary cavernous hemangioma complicated by smooth muscle hyperplasia
The nodule consisted of vascular endothelial and smooth muscle components. Immunohistochemistry showed the endothelial cells lining the inner lumen to be positive for anti-CD31, anti-CD34, and anti-von Willebrand factor (vWF) antibody, which are immunohistochemical markers of vessels. The smooth muscle component was positive for α-smooth muscle actin. Irregular elastic fibers were observed by elastic van Gieson (EVG) staining, and the distribution of elastic fibers was continuous in the surrounding lung tissue and hemangioma tissue, indicating that smooth muscle cells did not form a neoplastic vascular wall.
We finally diagnosed the patient with PCH with smooth muscle hyperplasia. The postoperative course was uneventful, and the patient was discharged after the surgery. Currently, a CT follow-up is underway at the outpatient department.
Discussion
Hemangiomas are benign vascular tumors commonly seen in the head and neck region [1, 2]. They are usually classified as capillary hemangioma, cavernous hemangioma, large-vessel hemangioma, skeletal muscle hemangioma, intravascular papillary endothelial hyperplasia, spindle cell hemangioma, and hobnail hemangioma based on their clinical appearance and the caliber of the vessel involved [1]. Cavernous hemangioma, a relatively uncommon variant, is histologically composed of tangles of capillaries or widely dilated vascular channels [1, 2]. Although cavernous hemangioma can occur throughout the body, it rarely occurs as a pulmonary tumor [2,3,4,5].
Ishikawa et al. summarized the 11 cases of PCH in 2010 [6]. Zhuang et al. also summarized 17 cases of PCH reported in the database of PubMed, Embase, and Web of Science from 1996 to 2017 [7], including their own case. We summarized these previous reports, including these two review reports, and searched the databases again, including PubMed, Embase, and Web of Science. We finally collected a total of 43 patients, including our present case (Table 1) [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. The age of the affected patients ranged from 10 weeks to 84 years old, with the highest incidence occurring in the 5th decade of life. Hemorrhaging was seen independent of age. Among the 43 patients with PCHs, 21 were men and 22 were women. Twenty of the 43 patients were asymptomatic, including our case. Among the symptomatic cases related to PCH, hemoptysis (n=8), cough (n=6), and hemosputum (n=4) were the most common symptoms. Life-threatening massive hemoptysis was reported in only one case [8]. The symptoms were not related to the size of the hemangioma [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. The number of pulmonary lesions in the reported cases was solitary in 27 of 43 cases and multiple in 16 of 43 cases.
The preoperative diagnosis is difficult because the clinical symptoms and imaging findings are scarce, and the imaging findings are similar to those of other malignant and benign pulmonary lesions. Radiologically, PCHs show solitary or multiple nodular lesions with no characteristic features. Fine and Whitney stated that calcification in PCH was indicative of organized thrombosis in the veins [2]. In the present case, chest CT did not show calcification of the nodules. The preoperative diagnosis was difficult in all previously reported cases as well, and a diagnosis was only made during or after surgery. Bae et al. [30] proposed the usefulness of dual-layer spectral CT for the diagnosis of PCH. Contrast-enhanced CT is useful for the diagnosis of liver cavernous hemangioma [32]. It may be also useful for the diagnosis of PCH above a certain size. In our case, the nodules were small and it was difficult to visualize under the mediastinal window setting.
In many cases, resection was performed for diagnostic and therapeutic purposes including enucleation, wedge resection, and lobectomy depending on the location and size of the hemangioma [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. In the case of solitary lung lesions, if a definitive diagnosis can be obtained during surgery, wedge resection or enucleation that preserves the lung function is desirable, as it is a benign lesion. However, for multiple lung lesions, complete resection of all lesions is not realistic. A careful follow-up is a good option for asymptomatic small lesions. No recurrence after complete resection has been reported thus far.
None of the previous reports pointed out a link to hemangiomas based on the presence of smooth muscle hyperplasia. In our case, smooth muscle cells were not neoplastic and did not surround the vascular lumen. The relationship between cavernous hemangioma and smooth muscle hyperplasia is unclear. Further analyses and the accumulation of cases will be needed to clarify this relationship.
Conclusion
We reported a rare case of PCHs and reviewed previous reports of similar cases. Cavernous hemangiomas are rarely seen in the lung. A preoperative diagnosis of PCH is difficult, and surgical resection is recommended as the treatment of choice for solitary lesions. If a tumor is diagnosed as PCH during the operation, wedge resection or enucleation is favored because of the benign behavior of such lesions.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PCH:
-
Pulmonary cavernous hemangiomas
- CT:
-
Computed tomography
- FDG-PET:
-
18F-fluorodeoxyglucose on positron emission tomography
- BNP:
-
Brain natriuretic peptide
- CEA:
-
Carcinoembryonic antigen
- CYFRA 21:
-
Cytokeratin fragment 21
- Pro-GRP:
-
Pro-gastrin-releasing peptide
- T-SPOT:
-
T cell spot
- sIL-2R:
-
Soluble interleukin-2 receptor
- TBLB:
-
Transbronchial lung biopsy
- VATS:
-
Video-assisted thoracic surgery
- vWF:
-
von Willebrand factor
- EVG:
-
Elastic van Gieson
References
Robbins SL, Cotran RS, Kumar V. Robbins pathologic basis of disease. Philadelphia: WB Saunders; 1999.
Fine SW, Whitney KD. Multiple cavernous hemangiomas of the lung: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:1439–41.
Wu JM, Lin CS, Wang JN, et al. Pulmonary cavernous hemangiomatosis treated with interferon alfa 2a. Pediatr Cardiol. 1996;17:332–4.
Maeda R, Isowa N, Sumitomo S, et al. Pulmonary cavernous hemangioma. Gen Thorac Cardiovasc Surg. 2007;55:177–9.
Kobayashi A, Ohno S, Bando M, et al. Cavernous hemangiomas of lungs and liver in an asymptomatic girl. Respiration. 2003;70:647–50.
Ishikawa T, Pollak S, Perdekamp MG, et al. Hemorrhage from a cavernous hemangioma with fatal blood aspiration: a rare cause of sudden unexpected death. Leg Med (Tokyo). 2010;12:308–12.
Zhuang BW, Li W, Chen ZF, et al. Multiple cavernous hemangiomas of the lung and liver mimicking metastasis: a case report and literature review. Medicine (Baltimore). 2018;97:e13509.
Sirmali M, Demirag F, Aydin E, et al. A pulmonary cavernous hemangioma causing massive hemoptysis. Ann Thorac Surg. 2003;76:1275–6.
Cleland WP. Cavernous haemangioma of the lung; report of a case. Thorax. 1948;3:48–52.
Forsee JH, Mahon HW, James LA. Cavernous hemangioma of the lung. Ann Surg. 1950;131:418–23.
Nakamura A, Uchiyama Y, Yamaoka N, et al. A resected case of cavernous hemangioma of the lung. Jpn J Chest Surg. 1998;12:167–71 [In Japanese with English abstract].
Taniguchi T, Iseki K, Nakade M, et al. A case of cavernous hemangioma of the lung. Jpn J Chest Surg. 1999;13:643 [In Japanese with English abstract].
Goodall JF, Stewart I. Cavernous haemangioma of the lung. Lancet. 1958;271:242–3.
Galliani CA, Beatty JF, Grosfeld JL. Cavernous hemangioma of the lung in an infant. Pediatr Pathol. 1992;12:105–11.
Ienaga H, Takahashi H, Dambara T, et al. Pulmonary cavernous hemangioma identification of its endothelial cell origin by immunohistological staining. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34:1427–30 [In Japanese with English abstract].
Kase M, Sakamoto K, Yamagata T, et al. A case of pulmonary cavernous hemangioma: immunohistological examination revealed its endothelial cell origin. Kyobu Geka. 2000;53:1055–7 [In Japanese with English abstract].
Fujita A, Tanaka R, Teruya M, et al. A resected case of cavernous hemangioma of the lung. Jpn J Chest Surg. 2003;17:578–81 [In Japanese with English abstract].
Giannopoulos S, Pelidou SH, Kyritsis AP. Multiple-organ cavernous hemangiomas involving brain, skin, and lung. Cornea. 2008;27:128.
Basile U, Cavallotti C, Burza A, et al. Cavernous haemangioma of the lung: a case report and review of the literature. Chir Ital. 2009;61:213–6.
Kunitani K, Uchiyama M, Taniguchi T, et al. A case of cavernous hemangioma arising from the anterior mediastinum and lung. Jpn J Chest Surg. 2010;24:1081–5 [In Japanese with English abstract].
Lovrenski A, Panjkovic M, Eri Z, et al. Cavernous hemangioma of the lung. Med Pregl. 2011;64:327–30.
Matsubara S, Nonaka H, Kobayashi M, et al. Uterine artery pseudoaneurysm after dilation and curettage in a woman with multiple hepatic and pulmonary cavernous hemangiomas. Int J Gynaecol Obstet. 2014;125:84–5.
Chen QR, Li H, Hu B, et al. Multiple cavernous hemangiomas of the lung. Ann Thorac Surg. 2014;98:1835–7.
Yang LL, Dai J, Xiao Y, et al. Cardiac cavernous hemangioma and multiple pulmonary cavernous hemangiomas. Ann Thorac Surg. 2014;97:687–9.
Jia CY, Sun SL, Zhang XK, et al. Pulmonary cavernous hemangioma: a case report. Chinese German J Clin Oncol. 2014;13:549–50.
Miyamoto U, Tominaga M, Tomimitsu S, et al. A case of multiple pulmonary cavernous hemangioma. Respirol Case Rep. 2015;3:29–32.
Wang C, Chen H, Sun L, et al. Cardiac cavernous hemangioma coexisting with pulmonary cavernous hemangiomas and giant hepatic hemangioma. Ann Thorac Surg. 2017;103:e149.
Gandhi S, Das B, Basu R, et al. A rare case of solitary pulmonary cavernous haemangioma with non-resolving recurrent haemoptysis. Indian J Thorac Cardiovasc Surg. 2019;35:51–4.
Ancel J, Perotin JM, Dewolf M, et al. A case of multifocal cavernous haemangiomas of the lung, spleen and bone. Rev Mal Respir. 2020;37:275–9 [In French with English abstract].
Bae K, An HJ, Jung JJ, et al. Diagnosis of multiple pulmonary cavernous hemangiomas via dual-layer spectral CT: a case report. Medicine (Baltimore). 2020;99:e22495.
Lee JH, Lee YU, Kang HJ. Multiple cavernous hemangiomas of the posterior mediastinum, lung, and liver: a case report. J Chest Surg. 2021;54:547–50.
Brancatelli G, Federle MP, Blachar A, et al. Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology. 2001;219:69–74.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
TI and SK analyzed and interpreted the patient data. TI, TK, MS, and SN treated the patient. TI and SK reviewed previous reports and prepared the manuscript. KS supervised this study. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
The written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ibe, T., Kosaka, T., Sugano, M. et al. Pulmonary cavernous hemangioma combined with smooth muscle hyperplasia: a case report and review of the literature. Gen Thorac Cardiovasc Surg Cases 2, 22 (2023). https://doi.org/10.1186/s44215-023-00048-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44215-023-00048-z