Abstract
In recent years, there has been a growing awareness of the limitations and risks associated with the overreliance on opioids in various surgical procedures, including cardiothoracic surgery.
This shift on pain management toward reducing reliance on opioids, together with need to improve patient outcomes, alleviate suffering, gain early mobilization after surgery, reduce hospital stay, and improve patient satisfaction and functional recovery, has led to the development and widespread implementation of enhanced recovery after surgery (ERAS) protocols.
In this context, fascial plane blocks are emerging as part of a multimodal analgesic in cardiac surgery and as alternatives to conventional neuraxial blocks for thoracic surgery, and there is a growing body of evidence suggesting their effectiveness and safety in providing pain relief for these procedures.
In this review, we discuss the most common fascial plane block techniques used in the field of cardiothoracic surgery, offering a comprehensive overview of regional anesthesia techniques and presenting the latest evidence on the use of chest wall plane blocks specifically in this surgical setting.
Similar content being viewed by others
Introduction
Over the last decade, there has been a notable trend in surgical techniques and approaches toward less invasive procedures, and regional anesthesia has evolved to complement these changes [1]. In particular, new and more superficial regional anesthesia techniques have been developed to align with the principles of minimally invasive surgery and enhanced recovery protocols [2].
The shift toward opioid-sparing techniques and the incorporation of regional anesthesia into cardiothoracic surgery pain management protocols reflect a broader trend in medicine toward improving patient outcomes, reducing complications, and enhancing the overall surgical experience for the patient [1].
Enhanced recovery after surgery (ERAS) protocols [1, 2] aims to improve functional recovery and patient outcomes trough a multimodal multidisciplinary approach in order to minimize surgical stress response and postoperative pain, alleviate suffering, gain early mobilization after surgery, reduce hospital stay, and improve patient satisfaction.
In this context, regional anesthesia is a valuable component of ERAS protocols for cardiac and thoracic surgery [1, 2]. By providing effective pain relief while minimizing opioid use, it can contribute to improved patient outcomes and a faster recovery process.
Traditionally, opioids have been a cornerstone of pain management in cardiothoracic surgery.
In recent years, there has been a growing awareness of the limitations and risks associated with the overreliance on opioids in cardiothoracic surgery and other surgical procedures.
Today, there is a new generation of regional anesthesia techniques, called fascial plane blocks [3].
These blocks are emerging as an effective alternative to conventional techniques such as paravertebral, epidural, or spinal blocks, and involve the injection of a local anesthetic between the muscles through which the peripheral nerve travels. The nerve itself is not targeted, and the needle is not directed toward the neural axis; therefore, the risks of serious complications such as neural injury and neuraxial hematoma can be prevented or at least reduced [4].
In this review, we discuss the most common fascial plane blocks used in the field of cardiothoracic surgery, offering a comprehensive overview of regional anesthesia techniques and presenting the latest evidence on the use of chest wall plane blocks specifically in this surgical setting.
Thoracic fascial plane blocks
Understanding the anatomy of fascial layers and their significance in regional anesthesia is crucial for anesthesiologists when administering nerve blocks and interfascial plane blocks to manage pain during various medical procedures.
Regarding fascial tissue anatomy in the human body, 3 fascial connective layers must be addressed [4]:
-
Superficial fascia: this is the layer of connective tissue that lies just beneath the skin. It contains fat and provides a separation between the skin and underlying structures.
-
Deep fascia: the deep fascia is a dense membrane of connective tissue that extends throughout the body. It surrounds and encases muscles, nerves, and other structures. It plays a crucial role in providing structural support and compartmentalizing different body regions.
-
Muscle-related fascial layers: within the context of muscles, there are three primary fascial layers: epimysium (the connective tissue that surrounds the entire muscle); perimysium (which surrounds bundles of muscle fibers called fascicles); and endomysium, which surrounds individual muscle fibers within the fascicles.
The deep fascia is particularly important in the setting of interfascial plane blocks because it is the primary target for these blocks. Deep fascia is a continuous membrane that connects various anatomical structures, including mechanoreceptors and nervous fibers. Targeting the deep fascial layers with regional anesthesia techniques can effectively block sensory input and provide pain relief [4, 5].
Advances in ultrasound technology have made it easier to identify and target specific fascial planes within the thoracic region (Table 1). This has certainly contributed to the growth in popularity of these techniques, also allowing to abandon more risky blind approaches.
We can classify thoracic fascial plane blocks into:
-
Anterior chest wall blocks: parasternal intercostal plane block (including superficial and deep parasternal block);
-
Antero-lateral chest wall blocks: includes pectoral nerve block (pectoralis nerve block I and II) and serratus anterior plane block;
-
Posterior chest wall block: includes the erector spinae plane block.
Methods
An extensive literature search was conducted for the present review. For this, a computer-based search was performed in PubMed, Embase, and Scopus databases. The date range for the search was set from January 2010 to September 2023.
After reading the titles and abstracts, the records obtained from the database were pre-selected by the authors. Those whose, after reading the full text, were not thought to be consistent with the review in terms of content were excluded. Since our study was designed as an article in the category of narrative review, standard methodological methods and statistical analysis were not used in meta-analyses.
We evaluated the quality of data available on each plane block and assigned a level of evidence as previously defined by the Oxford Centre for Evidence-Based Medicine (Table 1) [6].
Parasternal block—parasternal intercostal plane block
The parasternal intercostal plane (PIP) block targets the anterior cutaneous branches from T2 to T6 intercostal nerves, covering the anterior and medial chest wall. The technique can be divided into superficial and deep PIP block depending on whether the local anesthetic (LA) is deposited above or below the intercostal muscle (IM). Due to the nervous overlap, a bilateral injection is required to ensure the full coverage of the sternal area. PIP block provides analgesia and anesthesia after median sternotomy, sternal fractures or subcutaneous implantable cardioverter defibrillator (S-ICD) implantation, and to the internal mammary region after artery harvesting [7,8,9].
A further indication is breast surgery of the medial region of the chest or radical mastectomies in association with the interpectoral plane (PECS I), pectoserratus plane (PECS II), and serratus anterior plane block (SAPB) [10,11,12].
Superficial PIP block
The superficial PIP block was first introduced by Torre et al., in 2014, under the name of pectointercostal fascial plane block, and then redefined by Fusco et al., in 2017, as an analgesic technique used in breast surgery to cover the medial region of the mammary gland [13, 14], and in combination with the PECS I, PECS II, and SAP blocks.
The superficial PIP block is performed with the patient in the supine position. A high-frequency linear probe is positioned parallel and laterally to the sternum at the level of the second and fourth intercostal space. The needle is inserted with the in-plane (IP) approach in the cranial to caudal or caudal to cranial direction into the fascial plane between the pectoralis major muscle (PMM) and the external intercostal muscle (EIM) (Fig. 1A, B).
A Superficial parasternal block. Patient and probe position. The needle is inserted with the in-plane approach in the cranial to caudal or caudal to cranial direction. B Ultrasound landmarks of superficial and deep parasternal block. From top to bottom: pectoralis major muscle, external intercostal muscle, internal intercostal muscle, transversus thoracis muscle, pleura, ribs. PMM, pectoralis major muscle; EIM, external intercostal muscle; IIM, internal intercostal muscle; TTM, transversus thoracis muscle
Some clinicians have observed that the anatomical convexity of the ribs might limit the correct and adequate diffusion of the volume of LA in the fascial plane of the intercostal space, hindering fascial hydrodissection, and reducing the dermatomal spread (Fig. 2A).
A Superficial parasternal block. At level of second and fourth intercostal spaces, the local anesthetic is injected between the pectoralis major muscle and the external intercostal muscles. PMM, pectoralis major muscle; EIM, external intercostal muscle; N, needle; LA, local anesthetic. B Superficial parasternal block–modified approach. The injection on the dome of the rib allows a more homogeneous and longitudinal diffusion of local anesthetic, obtaining a better dermatomal coverage. PMM, pectoralis major muscle; IIM, internal intercostal muscle; EIM, external intercostal muscle; N, needle; LA, local anesthetic
As a result, Sepolvere et al. have suggested a modified approach by positioning the tip of the needle on the rib dome in order to reduce the local anesthetic volume and obtain a more homogeneous and longitudinal spread into the target fascial compartment [15] (Fig. 2B).
Initially proposed as an analgesic technique to manage intra- and postoperative pain from cardiac sternotomy, the superficial PIP block has been also described in case reports as an anesthetic procedure for sternal surgery (debridement, total resynthesis) on patients in spontaneous breathing with high comorbidities, considered at risk of serious pulmonary complications related to general anesthesia and intubation [16,17,18].
Deep PIP block or transversus thoracis plane block
First described in 2015 by Ueshima H et al. as the transversus thoracis plane (TTP) block [19], the deep PIP targets the deep anterior cutaneous nerves, which run into the anatomical plane between the TTM and the PMM.
The patient and probe position, such as the approach and the needle insertion, are the same for both superficial and deep block (Fig. 1A). The ultrasound landmarks of deep PIP are represented in Fig. 1B. The LA is injected between the internal intercostal muscle (IIM) and the TTM.
Both superficial and deep PIP block are effective in blocking the anterior cutaneous branches of the thoracic intercostal nerves (Th2–6) [13], but some significant anatomical considerations are warranted. The TTM is a very tiny and variable muscle in many people and difficult to visualize with ultrasound. At the level of the fourth parasternal rib intercostal space, the internal mammary artery (IMA) and internal mammary vein (IMV) can be identified between the IIM and TTM as a longitudinal pulsatile structure approximately 1.5 cm from the lateral border of the sternum, making the fascial target of TTP block the same anatomical plane in which both IMA and IMV run (Fig. 3A).
A The internal mammary artery can be identified between the internal intercostal and transversus thoracis muscles. This anatomical plane represents the target of the transversus thoracis plane block. PMM, pectoralis major muscle; EIM, external intercostal muscle; IIM, internal intercostal muscle; TTM, transversus thoracis muscle; IMA, internal mammary artery. B Ultrasound anatomy after left internal mammary artery harvesting. Patients can have tissue disruption in the transversus thoracis plane muscle after the internal mammary artery harvest, making transversus thoracis muscle identification more difficult, and the deep parasternal intercostal plane block almost impossible to perform. PMM, pectoralis major muscle; EIM, external intercostal muscle; IIM, internal intercostal muscle
On this basis, the risk of pneumothorax, local anesthetic systemic toxicity (LAST), and IMA injury or hematoma should be considered when a deep PIP block is performed. Moreover, patients can have tissue disruption in the transversus thoracis plane after IMA harvesting, making TTM identification more difficult, and the deep PIP block almost impossible to realize (Fig. 3B).
Furthermore, if the block is done before cardiac surgery, both the right and left IMAs could be damaged, rendering the arteries unusable for bypass grafting. If the block is performed after left IMA harvesting at the end of coronary artery bypass grafting (CABG), only the right IMA can be damaged. Some believe that the superficial PIP block is a more protective and safer technique for IMA compared to deep PIP block performed far from vascular structures, pleura, and heart [20].
Literature review
The analgesic efficacy of deep PIP block after cardiac surgery has been reported in several trials in terms of satisfaction and opioid sparing, suggesting its potential role in fast track cardiac anesthesia [21,22,23,24].
Li et al. [25], in a meta-analysis involving 12 randomized controlled trials (RCTs) with a total of 730 patients, aimed to assess the impact of parasternal block (PSB), including both superficial and deep blocks, on various outcomes in the field of cardiac surgery and postoperative pain management. Patients in the PSB group reported lower numerical rating scale (NRS) scores compared to the control group at specific time points, including at extubation, 4 h after surgery, and 8 h. This indicates that PSB was associated with better pain relief during the immediate postoperative period. The use of PSB was found to reduce the incidence of postoperative nausea and vomiting (PONV). Moreover, patients who received PSB had a significantly reduced mechanical ventilation time, shorter lengths of stay in the ICU, and overall hospital stay.
In line with these results, King et al. [26], in a meta-analysis, assessed the effect of PSB in patients undergoing cardiac surgery with a sternotomy approach. In their analysis, they included several approaches, including superficial and deep PIP and both single-shot or continuous infusion. They reported a significant reduction in postoperative pain and opioid use.
In another meta-analysis, Liu et al. explored the adverse effects of deep PIP, observing that the procedure provides effective postoperative analgesia and inconclusive incidence of PONV, though no further complications or side effects were considered [27].
In a cadaveric study, Samerchua et al. evaluated the optimal injection technique of both superficial and deep PIP to cover the T2–T6 intercostal nerves, the presence of TTM and its ultrasound identification, and the location of the IMA. They found that TTM were found at the second and up to sixth intercostal spaces, and the IMA was located along the second to sixth intercostal spaces medially to the halfway point between the sternal border and the costochondral junction. Moreover, the dye spread after superficial PIP block was better and more localized compared to the deep PIP block. They concluded that an optimal technique for superficial PIP block was a triple injection at the second, fourth, and fifth intercostal spaces, while a double injection at the third and fifth intercostal spaces represented the best technique for the deep PIP block [28].
In another cadaveric model, Harbell et al. [29] opted for a deep PIP injection between rib 3 and 4 and observed consistent spread to 4–6 intercostal levels.
A current and controversial opinion in cardiac surgery is whether the PIP block should be performed before or at the end of surgery. Padala et al., in a single-blind, randomized trial compared the preincisional and postincisional PIP block, concluding that both the choices provide equivalent pain relief during the postoperative period [30]. Despite extubation time was significantly higher in the preoperative group, the authors identified higher duration of surgery and cardiopulmonary bypass as possible source of bias.
Zou et al. reported, in a double-blind, randomized trial, that the preemptive deep PIP block reduced the intraoperative opioid need and provided effective analgesia during the first 12 postoperative hours in patients undergoing off-pump CABG [31].
Rectus sheath block
The rectus sheath block (RSB) provides somatic analgesia to the anteromedial abdominal wall and periumbilical area after midline laparotomy abdominal surgery, targeting the anterior cutaneous branches from the T9 to T12 intercostal nerves. First described as a blind technique in 1899 by Schleich, the introduction of ultrasound made the ultrasound guided RSB a safe and effective ERAS procedure, reducing the opioid requirements and avoiding many complications related to neuraxial techniques and vascular injury.
In addition to the pain after median sternotomy, drainage catheter insertion sites are highly painful locations after cardiac surgery and, therefore, an adequate tube site pain control has an important role in overall pain management after cardiac surgery. Positioning is burdened by a high incidence of severe postoperative pain reported in the epigastric region, impairing the patient’s respiratory dynamics, potentially leading to prolonged weaning from ventilation [32, 33].
RSB can be performed at the end of the surgery after subxiphoid drainage placement. The patient is in the supine position, and a high−frequency linear probe is positioned just below the tubes emerging from the skin (Fig. 4A). The ultrasound landmarks are represented by the skin, the right (RAM) and left (LAM) rectus abdominis muscles, the rectus abdominis muscles sheath (RAMS), and the peritoneum.
A Patient and probe position. The patient is in the supine position and a high-frequency linear probe is placed just below the tube emergence from the skin. B The local anesthetic injected between the rectus abdominis muscle and its sheath. LRAM, left rectus abdominis muscle; LAMS, left abdominis muscle sheath; N, needle
Through an IP approach and a bilateral injection (lateral to medial first and medial to lateral subsequently), 15–20 ml of LA for each side is deposited between the rectus muscle and its sheath (Fig. 4B)
Literature review
RSB has a potential role as part of effective multimodal opioid-sparing approach in combination with superficial or deep PIP both to manage pain deriving from median sternotomy and subxiphoid drainages, as reported in two recent case series in the pediatric and adult populations [34, 35].
Toscano et al., in a case report, described the combined use of PIP and RSB blocks, also known as pectoralis-intercostal rectus sheath (PIRS) plane block, for pain in a fragile patient undergoing mediastinal revision via subxiphoid access due to deep sternal wound infection [36].
This technique can also be performed at induction of general anesthesia through the introduction of bilateral dwelling catheters that run from the epigastrium, where a single shot RSB is first administered bilaterally, to the sternal notch covering T1 to T10 dermatomes through a continuous infusion of LA in patients undergoing cardiac surgery via sternotomy, and receiving subxiphoid drainages [37, 38].
A further potential and innovative application for pain management after left ventricular assist device (LVAD) implantation via median sternotomy is the combination of bilateral deep PIP block to provide analgesia to the sternal region and unilateral RSB to ensure pain relief to left abdominal structures through which the LVAD driveline was inserted. This approach was described in a case report, resulting in good quality analgesia and leading to a quick discharge from the ICU without need for rescue analgesia administration [39].
Pectoralis nerve blocks
The PECS block is a fascial plane block that provides analgesia to the upper anterior chest wall. The PECS 1 block targets the medial and lateral pectoral nerves, anesthetizing the pectoralis muscles. The PECS 2 block, an extension of the PECS 1 block, provides an additional injection to block the upper intercostal nerves (T2–T7, including the intercostobrachial nerve) and, in addition, the long thoracic and thoracodorsal nerves. Due to their relative efficacy, simplicity, and safety, the PECS blocks have quickly gained in popularity [40]. Blanco first described the PECS 1 block for providing analgesia after breast surgery involving pectoralis muscles, and later described the PECS 2 as a modification of the PECS 1 for more extensive surgeries and those involving axillary dissections [11, 12]. Recently, in order to standardize the nomenclature of regional anesthesia techniques, a consensus was drafted by representatives of both the American Society of Regional Anesthesia and Pain Medicine (ASRA) and the European Society of Regional Anesthesia and Pain Therapy (ESRA), referring to the PECS I block as an interpectoral plane block, and PECS 2 as pectoserratus plane block [41].
The PECS 1 block can be carried out using a linear ultrasound probe. The probe is positioned in a sagittal orientation, in the deltopectoral groove. When the axillary artery and vein are visualized, the probe is slid downwards until ribs are visualized (Fig. 5A). Pectoralis major is recognized as the large superficial muscle beneath the subcutaneous tissue, with the pectoralis minor deeper into it. At this level, there is the pectoral branch of the thoracoacromial artery, which pulses between the pectoralis muscles, with the lateral branch of the pectoral nerve typically close to the artery. Usually, a volume of 10 ml of LA is deposited in the fascial plane between the pectoralis muscles to perform a standard block [11, 41] (Fig. 5B).
PECS 2 is the modified version of the PECS 1 block and consists of two separate injections. The first injection aims to deposit LA in the fascial plane between pectoralis muscles (same as PECS 1 block). Then, sliding the probe onto the anterior axillary line, the 3rd and 4th ribs are visualized (Fig. 6A). A slight rotation is made to the probe to allow needle insertion along a superiormedial to inferior-lateral passage. Usually, 20 ml of LA is then deposited in the plane between pectoralis minor and serratus anterior muscles [12, 41] (Fig. 6B).
A PECS 2 before injection of local anesthetic. B PECS 2 after injection of local anesthetic, which spreads into the fascial layers between pectoral minor and serratus anterior muscles. PMM, pectoralis major muscle; PMm, pectoralis minor muscle; SM, serratus anterior muscle; N, needle; LA, local anesthetic
Literature review
First described by Blanco for providing analgesia after breast surgery, PECS blocks have progressively been used for a wide variety of breast surgery procedures. In 2020, the PROSPECT Working Group (a collaboration of surgeons and anaesthetists working to formulate procedure-specific recommendations for pain management in several surgical settings) developed recommendations based on a procedure-specific systematic review of randomized controlled trials. According to PROSPECT recommendations for oncological breast surgery, PECS blocks were suggested for major breast surgery if no axillary node dissection is performed or if paravertebral block (PVB) is contraindicated (grade A recommendation) [42]. However, a review of the same recommendation made by Italian opinion leaders has highlighted that PECS 2 block can be used to cover muscles, axilla, and lateral branches of the intercostal nerves (T2–T7), allowing surgeries involving the axilla (level 1), such as sentinel node biopsy and axillary dissection. For this reason, when the axilla is involved, PECS 2 block represents an effective and safer alternative compared to PVB, which is not an “entry level” block due to its potential difficulties and complications. Moreover, PVB does not cover the cervical and brachial plexus branches, which contribute to the innervation of the breast and axillary region [43,44,45]. PECS blocks have also demonstrated its analgesic efficacy in plastic surgery [46]. However, a promising field of application is cardiothoracic surgery, including thoracotomy, video-assisted thoracoscopic surgery (VATS), median sternotomy, cardiac interventional procedures, thoracic trauma, and Port-a-Cath insertion [47].
Kumar et al. [48] randomized 40 patients scheduled for CABG or valve surgeries via midline sternotomy to postop PECS block or no block. In the PECS group, extubation was significantly earlier, with a median ventilatory duration of 108.5 ± 24.33 versus 206.3 ± 47 min and pain scores at rest and with cough were also significantly lower at zero, three, six, 12, and 18 h after surgery.
Moreover, Marcoe et al. [49] compared 112 patients who received PECS 1 block, subcostal transversus abdominis plane (TAP) block multimodal analgesia, or multimodal analgesia without regional block. The group that received regional blocks had a 51.1% reduction in intraoperative opioid requirements (p < 0.001).
Yalamuri et al. [50] also described a case in which PECS 2 block was used as rescue analgesia in a patient undergoing mitral valve repair via right anterior thoracotomy. However, despite potentially useful, no trials are available for the use of PECS in mini invasive cardiac surgery.
In a prospective randomized trial, Yildirim et al. [51] compared thoracic paravertebral block (TPVB) with PECS II for postoperative analgesia in patients undergoing VATS. They enrolled 26 patients for each group and no significant differences were found in static and dynamic VAS score in the first 24 postoperative hours. However postoperative morphine consumption and rescue analgesia requirement were higher in the PECS group. On the other side, PECS II block provided better intraoperative hemodynamic stability compared to TPVB. In 2021, Luo et al. [52] recruited 40 adult patients undergoing lobectomy, segmentectomy, and partial lung resection and highlighted how PECS 2 block preconditioning significantly reduced surgical stress, stabilized blood flow, and prolonged the time required for first analgesia. It also reduced surgical pain related to the incision, and opioid consumption, often responsible for serious side effects.
PECS blocks have also been successfully used as a valid analgesic technique in pediatric surgery.
Kaushal et al. [53] compared the effectiveness of ultrasound-guided deep SAP block, PECS 2 block, and intercostal nerve block in the treatment of pain after thoracotomy in pediatric cardiac surgery. These blocks showed comparable effectiveness on pain scores in the early postoperative period (1 to 4 hours).
Kamal et al. [54] compared the analgesic effect of bilateral PECS 2 block with conventional intravenous analgesia (control) on post-sternotomy pain after cardiac surgery in children. The block group had lower pain scores and lower postoperative opioid requirements compared with the control group. Additionally, agitation upon awakening and length of stay in the ICU were lower in the study group.
The mechanism by which PECS 2 blockade mediates post-sternotomy analgesia is unclear. Though these blocks are not expected to cover the anterior cutaneous branches of the intercostal nerves, several studies have reported effective analgesia with PECS blocks during median sternotomy in pediatric cardiac surgery [48, 54]. In fact, for median sternotomy, bilateral PECS 2 blockade has been shown to be superior to systemic analgesia alone, though the mechanism is unclear. PECS blocks are not expected to block the anterior cutaneous branches of the intercostal nerves; however, they may exert an analgesic effect by reducing the spasm in pectoral or intercostal muscles [47].
Pectoral nerve blocks have also been successfully used in interventional cardiac procedures. PECS 2 alone and in combination with general anesthesia has been shown to facilitate cardiac device implantation and transcatheter procedures [55], while PECS 1 block for cardiac device implantation in combination with general anesthesia has been shown to provide optimal analgesia in children [56]. PECS blocks have also been used with success for Port-a-Cath insertion [57].
Serratus anterior plane block
The SAPB is a fascial plane block, and initially described by Blanco et al. [58] with the intent of providing analgesia for the lateral chest. It is an appropriate choice for procedures involving the lateral thorax (anterolateral thoracotomy, robotically assisted approaches).
The SAPB can be performed with two different techniques, depending on the LA injection site: in the superficial SAPB, the LA is deposited in the interfascial plane between the serratus anterior muscle (SAM) and the latissimus dorsi muscle; in the deep SAPB, the LA is deposited between the SAM and intercostal muscles at the intersection of the V rib.
SAPB can be performed as single-shot or continuous block through the placement of a peripheral nerve catheter in the interfascial plane. With the patient in lateral or supine position, an ultrasound probe is placed at the level of the midclavicular line in a sagittal plane. The ribs are counted with caudal and lateral probe movement until the fourth and fifth ribs are identified in the midaxillary line. At this level, the SAM, visible as a small hypoechoic muscle, overlies the ribs, while the latissimus dorsi muscle is clearly identifiable superficial to the SAM (Fig. 7A).
A Sono-anatomy of SAPB: In the superficial SAPB, the target is the interfascial plane between LD and SAM; in the deep SAPB, the target is the interfascial plane between SAM and the periosteum of the V rib. B Deep SAPB: the needle is advanced in-plane in the interfascial plane between the SAM and the V rib and LA is injected. LD, latissimus dorsi; SAM, serratus anterior muscle; P, pleura; LA, local anesthetic; N, needle
The needle is introduced in the caudal-cephalad direction using an in-plane approach, and after confirming the position of the tip by hydrodissection, LA is deposited above (superficial SAPB) or below (deep SAPB) the SAM (Fig. 7B).
After the interfascial space is opened with LA or saline, a catheter can be placed inside the serratus anterior muscle plane with a continuous infusion of LA (continuous SAPB). Deep SAPB may be preferable in authors opinion because the deeper approach can provide simplified sonographic imaging, and by inserting the catheter between the serratus muscle and V rib, there is probably less risk of dislocation [59] (Fig. 8A, B).
The lateral cutaneous branches of the intercostal nerves traverse both the deep and superficial serratus anterior planes and are the targets of both blocks. At the midaxillary line, the lateral cutaneous nerves penetrate the external intercostal and serratus anterior muscles, further dividing into anterior and posterior divisions, which innervate the anterolateral chest wall.
Daga et al. [60] undertook a descriptive cadaveric study to delineate the extent of the cephalo-caudal spread of the injectate after superficial SAPB, showing the diffusion area, including the lateral cutaneous branches of the second to sixth intercostal nerves, the long thoracic nerve, and the thoracodorsal nerve. Therefore, anatomically, both superficial and deep SAPB can block the lateral cutaneous branch of the intercostal nerve, while superficial SAPB also affects the long thoracic and the thoracodorsal nerves that lie on top of the SAM.
Blanco et al. demonstrated a longer duration and better spread of LA with the superficial block compared to the deeper [58]. However, two human cadaveric studies examined the spread of dye after 20 ml or 40 ml of methylene blue injection: increasing the volume from 20 to 40 ml doubled the area of injectate spread and promoted dye spread preferentially to the anterior chest wall and axilla, providing a more reliable analgesic coverage; consequently, using 40 ml of solution, the duration and distribution were the same for the superficial and the deep block, precisely from T2 to T9 [61, 62].
Literature review
Initially utilized in breast surgery [63], the use of SAPB has greatly increased in both thoracic and cardiac surgery. The guidelines for the perioperative management of patients undergoing lung surgery recommend SAPB in single-port VATS or when paravertebral blockade is not appropriate (e.g., pleurectomy and decortication) [2].
Despite the small incision, a moderate-severe postoperative pain following VATS is not rare, affecting expectoration and leading to complications, such as pulmonary infection [64]. Viti et al. randomly allocated 94 patients eligible for VATS into two groups: opioid-based systemic pain treatment (control group) and the same systemic analgesics regimen plus pre-emptive SAPB (interventional group). They found that SAPB provided better pain control and, consequently, a better performance during postoperative rehabilitation exercises in terms of duration and quality of incentive spirometry [65].
SAPB represents a safe, effective alternative to standard of care in the treatment of thoracic pain in the acute setting, such as rib fractures [66] or chest tube placement [67].
Continuous SAPB has been described in case reports and case series on post-operative pain management after lung transplantation [68] for post-thoracotomy analgesia [69] and for pain relief in multiple fractured ribs [70]. Moreover, SAPB has been successfully used for the treatment of post-thoracotomy [71] and postmastectomy pain [72]. SAPB has also achieved a prominent role in postoperative pain management in minimally invasive cardiac surgery via thoracotomy.
An observational cohort study evaluated the analgesic impact of continuous deep SAPB (interventional group n = 33) against opioid-based systemic analgesia (control group n = 26) for patients undergoing minimally invasive mitral valve surgery through right minithoracotomy. The authors noted a marked reduction in morphine consumption in the first 24 h in the interventional group, allowing good quality analgesia with low consumption of opioids [59].
In a double-blind RCT, Gautam et al. achieved similar results, showing that SAPB reduced the postoperative pain scores and opioid requirements in patients undergoing minimally invasive direct coronary artery bypass (MIDCAB) surgery [73].
Moreover, SAPB, alone or combined with parasternal block, has been shown to be an effective and durable means of treating pain associated with subcutaneous implantable cardiac defibrillator (S-ICD) placement [74].
SAPB has been compared to erector spinae plane block in also in thoracic surgery With regard to thoracotomy, ESPB has shown a superior analgesic profile to SAPB in several clinical trials [75, 76]. Specifically, Elsabeeny et al. [75] compared, in a randomized trial, the analgesic efficacy of ESPB, SAPB, and TEA in perioperative pain control in thoracotomy surgery. While ESPB and TEA showed a nearly comparable analgesic profile, both were superior compared to SAPB. The postoperative morphine consumption was also higher in patients in the SAPB group.
Taking all of this into account, the authors suggested a possible role of ESPB as alternative to TEA in thoracotomy surgery, with a secondary role for the SAPB. Mixed results were instead found for VATS: Ekinci et al. [77] found lower pain scores and lower opioid consumption in the ESPB group compared with deep SAPB; in a pilot randomized comparison trial, Gaballah et al. [78] found comparable results, while Finnerty et al. [79] showed the superiority of ESPB, both in analgesic effect and opioid consumption.
In line with these studies, the PROSPECT guidelines for VATS cannot actually consider SAPB as first‐line treatment until its efficacy compared with the more established paravertebral and ESP blocks has been confirmed by other studies [80].
However, the same PROSPECT guidelines underlined how the SAPB, which is simple and quick to perform with limited side-effects, could bring benefits in terms of pain and opioid consumption compared with systemic basic analgesia. This is also confirmed by a recent meta-analysis by De Cassai et al. [81], which assessed the analgesic efficacy of SAPB compared with general anesthesia only for VATS peri-operative pain control. In their study, seven RCTs, for a total of 489 patients, were included. In the SAPB group, pain scores at 6, 12, and 24 h were reduced, together with a reduction in postoperative opioids (mean difference − 4.81 mg of intravenous morphine equivalent, 95% CI − 8.41 to − 1.22) and in the incidence of nausea and vomiting.
Erector spinae plane block
The ESPB was first described by Forero, in 2016, and is considered a relatively recent addition to the field of regional anesthesia and pain management [82]. The ESPB involves the injection of LA into the interfascial plane located between the erector spinae muscles and the tip of the transverse vertebral process.
ESPB can be performed in different positions, depending on the clinical situation and the preferences and expertise of the health care provider. ESPB can be performed with the patient in a sitting position (Fig. 9A), prior to general anesthesia, or can also be performed with the patient in a lateral position. This can be done either before or after the induction of general anesthesia, depending on the clinical circumstances and the anesthesia team’s preferences.
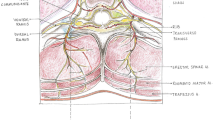
A ESPB performed with the patient in sitting position before general anesthesia induction. B Sono-anatomy of the ESPB block: trapezius (uppermost), rhomboid (middle), and erector spinae (lowermost) are identified. The hyperechoic T4 transverse process is individuated inferior to the erector spinae muscle. TR, trapezius muscle; RH, rhomboid muscle; ESM, erector spinae muscle; T4, transverse process
To perform the block in cardiothoracic surgery, a linear probe is generally placed in a sagittal view at the level of T4-spinous process, 2–3 cm laterally from the midline in order to identify the T4 transverse process, the trapezius, rhomboideus, and erector spinae muscles (Fig. 9B).
The needle is then inserted via an in-plane approach, and LA is injected in the caudal to cranial direction into the interfascial plane between the erector spinae muscle and the transverse process (Fig. 10A). By the placement of a peripheral nerve catheter in the interfascial plane, a continuous ESPB can be performed (Fig. 10B).
A ESPB: the needle is advanced with an in-plane approach in caudo-cranial direction to reach the interfascial plane between the transverse process and the erector spinae muscle. B Ultrasound visualization of the ESPB catheter between the ESM and the transverse process. ESM, erector spinae muscle; LA, local anesthetic; N, needle; T4, transverse process
Since its first description, ESPB has gained attention and stimulated an interesting debate over its mechanism of action [83]. To date, thanks to several cadaveric studies and to magnetic resonance imaging, we know that ESPB has been found to provide both somatic (related to the body wall and musculoskeletal structures) and visceral (related to internal organs) analgesia. This suggests that it can be effective for managing pain originating from different sources [84, 85].
In fact, it has been observed that the LA injected into the fascial plane between the erector spinae muscles and the transverse vertebral processes can spread through channels in the intertransverse connective tissues, reaching the ventral and dorsal ramus of the thoracic spinal nerve along with the sympathetic ramus communicans at the intervertebral foramen level. Moreover, the involvement of lateral cutaneous branches of intercostal nerves contributes to the block’s analgesic effect.
Scharztmann et al. [84], using magnetic resonance imaging (MRI), have provided valuable insights into the spread and clinical effects of the ESPB injectate. The MRI study demonstrated that the injectate used in ESPB consistently spreads to several anatomical areas. These areas included the erector spinae muscles (which are the target of the block), neural foramina (openings through which spinal nerves exit the spinal column), and the intercostal space (the space between the ribs).
The distribution of the erector spinae muscle (ESM) from the neck to the lumbar region makes ESPB a versatile regional anesthesia technique. Its ability to provide analgesia in a wide area of the torso, including the thoracic region, has indeed contributed to its popularity in various surgical procedures. Here are just some of the reasons that ESPB has gained popularity, especially in cardiothoracic surgery.
Literature review
Several randomized trials have been conducted to compare ESPB with other regional anesthesia techniques like epidural anesthesia, paravertebral blockade, and SAPB in thoracic surgery. ESPB is being actively studied and considered as a potential anesthesia technique in thoracic surgery, particularly for VATS and open thoracic surgery.
At present, enhanced recovery after surgery (ERAS) guidelines [2] recommend thoracic paravertebral block (TPVB) as a valid locoregional alternative to thoracic epidural anesthesia (TEA), with evidence of a better side effect profile. Therefore, in recent years, together with the growth in popularity of ESPB, several trials have compared it with PVB in thoracic surgery.
In a recent meta-analysis, which included 10 randomized trials on the topic, for a total of 624 patients, it was found that PVB was associated with improved pain scores only at 12 h after thoracic surgery, but with a lower opioid consumption at 48 h. On the other hand, ESPB was associated with a borderline significant trend toward reduction of block-related complications. These results suggest a possible role of ESPB as first choice, especially in patients undergoing VATS surgery and in those with coagulation disorders [86].
Regarding thoracotomy surgery, in a randomized trial, Das et al. [87] compared the analgesic efficacy and safety of preoperative, single-shot ultrasound-guided TPVB, ESPB, and SAPB in 90 patients scheduled for thoracic surgery undergoing posterolateral thoracotomy. They reported a better analgesic efficacy of ESPB compared with TPVB and SAPB, together with lower total opioid dose required and VAS score during the first 24 h.
Similar results were obtained in the already mentioned trial performed by Elsabeeny et al. [75], which compared ESPB, SAPB, and TEA for pain management in thoracotomy pain. Also in this trial, ESPB was superior to SAPB in terms of pain scores and opioid consumption in open thoracic surgery. In particular, outcome measures included 24 h postoperative visual analog scale (VAS), intraoperative rescue fentanyl consumption, and total postoperative morphine consumption. VAS scores at rest were significantly lower for the TEA group compared to the SAPB group and comparable between TEA and ESPB. In the SAPB group, 88.2% of the patients required postoperative morphine compared to 47.1% in the ESPB group and the total postoperative morphine consumption was higher in the SAPB group compared to the TEA and ESPB groups. Moreover, the first time to receive morphine was longer in the ESPB compared with SAPB group.
The efficacy of ESPB for VATS have been also described in several trials.
Zhao et al. [88], in a prospective randomized trial, compared ESPB with PVB for pain management in VATS surgery. The primary outcome was the postoperative oxycodone consumption at 48 h. Their trial showed the non-inferiority of ESPB regarding pain score, analgesic rescue consumption, and quality of recovery. Specifically, postoperative oxycodone consumption at 48 h was 7.9 ± 8.7 boluses in ESPB and 6.9 ± 6.3 boluses in PVB groups and the time to first oxycodone rescue was 16.1 ± 5.3 h in ESPB group vs. 15.8 ± 8.7 h in PVB group. No difference was detected in postoperative pain score at 12 h, 24 h, 36 h, and 48 h.
Finnerty et al. [79] compared ESPB and SAPB in terms of quality of recovery and overall morbidity after minimally invasive thoracic surgery. They found a clinically meaningful improvement in quality of recovery at 24 h for patients who received ESPB compared with a SAP block. Furthermore, ESPB showed a longer time to first opioid analgesia, and reduced pain at rest and on deep inspiration.
ESPB has also gained popularity as a valid alternative option for pain management in cardiac surgery. Athar et al. [89] compared bilateral ESB with 20 ml per side of 0.25% levobupivacaine (group E) or sham block with 20 ml of normal saline in patients undergoing elective on-pump single-vessel coronary artery bypass grafting or valve replacement. They found that single-shot ESPB decreased the first 24-h postoperative analgesic consumption by 64.5%, and risk of pain by five times in the patient population, also reducing the sedation and duration of mechanical ventilation in postcardiac surgery patients.
Similar results were reported in a randomized trial [90] that compared continuous ESPB with multimodal intravenous analgesia in 40 patients undergoing coronary bypass surgery. In this trial, the ESPB group showed a significantly lower VAS score than in the group of multimodal i.v. analgesia. Intraoperative fentanyl and postoperative morphine doses were significantly less in the ESPB group, together with shorter duration of mechanical ventilation.
In a randomized study, Nagaraja et al. [91] compared the effectiveness of ESPB catheters to thoracic epidural analgesia in adult patients undergoing median sternotomy for cardiac surgery.
Bilateral ESPB catheters were non-inferior to thoracic epidural analgesia at least for the initial 12 h post-extubation. However, beyond 12 h, the thoracic epidural group had improved pain scores. Importantly, there were no significant differences in the need for rescue analgesia, or other complications between the two groups.
Krishna et al. [92], in a prospective, randomized, single-blinded study involving adult patients undergoing cardiac surgery, compared the use of preinduction single-shot ESPB to a control group receiving paracetamol and tramadol. Patients in the ESPB group received a single-shot of ESPB with 3 mg/kg of 0.375% ropivacaine before surgery. Patients in the control group received 1 g of paracetamol every 6 h and 50 mg of tramadol every 8 h for pain management.
Patients in the ESP group had a significantly longer duration of analgesia, during which their pain score was less than 4 compared to the control group. The duration of effective pain relief in the ESPB group was reported as 8.98 ± 0.14 h, while it was 4.60 ± 0.12 h in the control group.
The efficacy of monolateral ESPB has been also described for minimally invasive cardiac surgery in several observational and retrospective trials [76, 93].
However, results from these studies are in contrast with a recent double blind randomized trial by Hoogma et al. [94] which compared 36 patients treated with continuous ESP with 36 control patients for minimally invasive mitral valve surgery. The authors did not found any significant differences in primary (cumulative morphine consumption during the first 24 h after extubation) and secondary outcomes (severity of pain, presence/extent of sensory block, duration of postoperative ventilation, and hospital length of stay).
The efficacy of ESPB in cardiac surgery has also been described in the pediatric population by Karacaer et al. [95], who reported a significant reduction in morphine consumption in the first 24 h using bilateral ESPB for postoperative pain management in children undergoing median sternotomy. Moreover, Macaire et al. described the use of bilateral ESPB catheters in a pediatric cardiac population, reporting reduced pain and opioid requirements [96].
The results described are in line with a recent metanalysis from Nair et al. [97]. In their analysis, the authors included 16 RCTs that compared ESPB with a control group (no block/sham block) in adult and pediatric patients undergoing cardiac surgeries for a total of 110 patients. The primary outcomes were postoperative opioid consumption and postoperative pain scores. They found that single-shot ESPB or continuous analgesia via catheter was associated with reduced intraoperative and 48 h opioid consumption and with reduced pain scores after extubation up to 16 h. Moreover, patients treated with ESPB had reduced duration of ventilation, reduced ICU and hospital stay, and early mobilization. However, no significant reduction in 24-h opioid consumption, PONV, and pruritus was observed in ESPB group compared with control. However, it must be noted that studies included in this metanalysis had a very high level of heterogeneity due to variable sample sizes, different surgical approaches and surgeries, and single-shot and continuous blocks.
Safety of fascial plane blocks
Regional anesthesia techniques, including thoracic fascial plane blocks, can be associated with technical or needle-related complications. These may include bleeding at the injection site, inadvertent intravascular injection of local anesthetic, and nerve injury. In the thoracic region, where cardiac surgery often takes place, additional risks such as pneumothorax (air in the chest cavity) and hemothorax (blood in the chest cavity) should be considered.
Many patients undergoing cardiothoracic surgery may be on anticoagulation or antiplatelet therapy before, during, and after the procedure, potentially increasing the risk of bleeding complications associated with regional anesthesia techniques.
Evidence about the safety of fascial plane blocks in cardiac surgery is still sparse and the available literature consists mostly of case report and case series with a low level of evidence.
Adhikary et al. [98] reported the use of continuous ESPB for pain management in five patients undergoing left thoracotomy for left ventricular assist device placement. No complications were observed despite the need for prolonged postoperative heparinization.
Galacho et al. [99] reported no bleeding complications after ESPB in a case series of five patients with coagulation impairment (thrombocytopenia, INR > 1.5 and one patient on low-molecular-weight heparin anticoagulation).
A study by Toscano et al., in 2021 [100], provides valuable insights into the safety of fascial plane blocks, specifically continuous ESPB and SAPB in patients receiving anticoagulation and coagulopathy. The study involved a retrospective analysis of 70 patients undergoing minimally invasive mitral valve surgery through a right mini-thoracotomy. These patients received either continuous ESPB or SAPB for perioperative pain control, and coagulation status of patients at the time of catheter insertion and removal were assessed.
There were no adverse outcomes attributable to SAPB or ESPB in terms of vascular puncture, active bleeding, or hematoma formation, suggesting that these fascial plane blocks can be safely done in patients receiving anticoagulation and with coagulopathy.
Safety of fascial plane blocks have been also evaluated in thoracic surgery, with some data available from the analysis of secondary outcomes of RCTs.
Fang et al. [101], in a randomized trial, including 94 patients (not treated with antiplatelet or anticoagulant drugs) undergoing thoracotomy, reported 5 cases of hematoma in the group treated with PVB vs. 0 cases in the group treated with ESPB.
Similar results were reported by Chen et al. [102], in a randomized trial comparing intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery. They reported 4 cases of hematoma in the PVB group (16.7% of a total of 24 patients) vs. 0 cases in the ESPB group.
Given the available evidence, it is not surprising that there are currently no specific guidelines available on the use of fascia blocks in patients considered at risk of bleeding.
Therefore, the safety of performing nerve blocks in patients on anticoagulant therapy is a subject of ongoing debate, and may vary depending on regional guidelines and expert opinions.
The American Society of Regional Anesthesia and Pain Medicine guidelines [103], regarding regional anesthesia in patients receiving antithrombotic therapy, recommend the need for caution in patients on anticoagulants or antiplatelet drugs. In cases where deep plexus or peripheral blocks are performed, the guidelines recommend applying neuraxial guidelines, which involve assessing the patient’s coagulation status and considering the risks of bleeding.
The Austrian Society of Anesthesiology, Resuscitation, and Intensive Care has a more permissive stance when it comes to performing superficial nerve blocks in patients on anticoagulants [104]. They do not consider systemic coagulation to be an absolute contraindication for certain nerve blocks.
A panel of Canadian experts on regional anesthesia reviewed the evidence and classified the risk of bleeding complications following peripheral regional nerve blocks [105]. They categorized the risk of bleeding complications for SAPB and PECS as intermediate, while ESPB was considered at low risk.
To conclude, although current literature suggests a greater profile of fascial plane blocks compared to neuraxial anesthesia, to date, we have no evidence that definitively confirms their safety in patients at high risk of bleeding, such as those on anticoagulant therapy or undergoing major cardiothoracic surgery.
Adequately powered randomized trial in the context cardiothoracic surgery are warranted to better determine their safety of TPVB and ESPB in patients with an increased risk of bleeding.
Postoperative implications after loco-regional anesthesia: the fast track
The second millennium is the fast-track.
The concept of fast-track surgery, known today also as enhanced recovery after surgery (ERAS), was introduced in 1990 [106]. The goal was to optimize the perioperative care of surgical patients and accelerate their recovery while minimizing the stress response to surgery.
Since its first description, fast-track surgery has gained popularity in various surgical procedures including thoracic surgery, with the aim to improve patient satisfaction, reduce the length of hospital stays, and minimize the overall impact of surgery on patients’ daily lives.
The first, and pioneering, description of the fast track in thoracic surgery was that of Cerfolio et al. [107], which reported a case series of 500 pulmonary resection with a median discharge at day 4 (range 2–119 days) with 65% of the patients leaving before day 5, and a low 1.8% readmission rate, although they had a conventional thoracotomy. Cerfolio’s protocol included several elements intended to become the basis of the fast track, including early rehabilitation at day 1, epidural analgesia, removal of invasives by day 3, and discharge by day 4.
The implementation of VATS in thoracic surgery has facilitated the development of fast-track protocols or enhanced recovery after surgery (ERAS) programs in this field, and today, patients admitted for lobectomy are often discharged at home on the third postoperative day [108].
Achieving this outcome involves a comprehensive approach to perioperative management, with a specific focus on fast-track surgery principles, including prehabilitation and pulmonary rehabilitation programs, minimally invasive surgery approaches, an optimal intraoperative management and, obviously, a multimodal approach to pain [2].
Pain management is indeed a key component of fast track in thoracic surgery and is often a challenge for the anesthesiologist.
Pain after thoracic procedures can be debilitating and lead to poor outcomes, including respiratory complications such as atelectasis and pneumonia, as well as longer hospital stays, poor quality of life, and chronic persistent postoperative pain syndrome [109].
Together with recommendations for minimally invasive approach to surgery, ERAS strongly recommend a multimodal approach to pain, based on the combination of regional anesthesia techniques and non-opioid drugs, with the aim of reducing postoperative opioid use and its related side effects [2]. Actually, PVB is recommended as a valid alternative to TEA, with evidence of a better side effect profile and has become the first choice for postoperative analgesia in patients undergoing thoracic surgery, despite specific concerns, particularly regarding the risk of hematoma and pleural puncture, still remain.
Over the last 10 years, as surgery is moving toward less invasive techniques and approaches, regional anesthesia is also evolving and new and more superficial techniques have been described [3].
Specifically, in the context of thoracic surgery, new evidences about the efficacy of SAPB and ESPB are growing.
Capuano et al. [86], in a metanalysis, compared the analgesic efficacy of ESPB and PVB in thoracic surgery and reported a comparable pain scores at 6, 24, and 48 h after surgery, with a borderline significant trend toward reduction of block-related complications in favor of ESPB.
Similar considerations were advanced by Huang et al. [110] in another metanalysis, which showed that the PVB analgesic efficacy was comparable to that of ESPB in pain scores and opioid consumption at 24 h after surgery in a mixed population undergoing thoracic and breast surgery.
These findings are in line with the PROSPECT guidelines for VATS, which recommend the use of regional anesthesia techniques as fundamental components of fast track in thoracic surgery, suggesting the primary role of ESPB or PVB for postoperative pain management instead of the SAPB, considered as second choice [83].
Fast-track cardiac care is a complex intervention involving several components of care during cardiac anesthesia and in the postoperative period, with the ultimate aim of early extubation after surgery, and reduction of the length of stay in the ICU and in the hospital. Cardiac surgery can be associated with considerable postoperative discomfort and pain, and an optimal dynamic pain management has become a prerequisite for early postoperative recovery.
In the 1990s, high-dose opioid anesthetic strategies and mechanical ventilation in the ICU for 12 to 24 h were common [111]. Pain control based on the use of opioids was considered safe in hemodynamic terms and also protective for anti-ischemic and preconditioning effects [112]. This approach was eventually abandoned when it became well understood that the use and abuse of these drugs did not have beneficial results in these patients. On the contrary, it was the cause of a series of adverse effects (e.g., respiratory depression, bradycardia), ending in the extension of the extubation times. This idea was consolidated in 2019 with the enhanced recovery after cardiac surgery (ERACS) recommendations.
ERACS recommends effective perioperative pain control to improve patient outcomes, alleviate suffering, gain early mobilization after surgery, reduce hospital stay, and improve patient satisfaction and functional recovery [113]. In fact, poor pain management during the early postoperative period results in deleterious side effects on pulmonary (atelectasis, pneumonia, and bronchial secretion stasis), cardiovascular (increased oxygen consumption and tachycardia), and musculoskeletal (muscle weakness and disuse) systems that can prompt reintubation. As a solution, ERACS recommends multimodal analgesia, opioid sparing, and consideration of locoregional analgesia in all patients undergoing cardiac surgery procedures [112, 114].
Having now passed the era of neuraxial blocks (epidural and paravertebral block) due to the well-known side effects (e.g., epidural hematoma, pneumothorax) or due to concerns related to anticoagulation, cardiac anesthesia is oriented toward new regional techniques that can have the desired pain control as a final result. A number of studies have recently been published on fascial blocks in the cardiac surgery setting. The most studied blocks are parasternal superficial block, the pectoral block, and erector spinae plane block, and because these are all superficial blocks, they have fewer side effects and risk of hematoma formation [105].
A randomized control trial by Kumar et al., published in 2018 [48], analyzed forty adult patients undergoing coronary artery bypass grafting or valve surgeries through midline sternotomy. Group 1 patients did not receive PECS block, whereas group 2 patients received bilateral PECS block postoperatively. The PECS group patients required shorter duration of ventilator support (p < 0.0001) compared to the control group. Pain scores at rest and cough were significantly lower in the PECS group at 0, 3, 6, 12, and 18 h after extubation (p < 0.05). Furthermore, 34 episodes of rescue analgesia were registered in the control group, while in the PECS group there were only four episodes.
A more recent randomized control trial, by Zhang et al. [115], investigated the effect of bilateral pectointercostal fascial block in 108 patients undergoing open cardiac surgery allocated to receive either nerve block or no nerve block. This study concluded that the nerve block provides effective analgesia and accelerates recovery in terms of time of extubation, and ICU and hospital length of stay in patients undergoing open cardiac surgery.
A meta-analysis by Dost et al. [116] analyzed the effects of regional anesthesia on postoperative opioid consumption in patients undergoing open cardiac surgery. This study concluded that all the regional anesthesia techniques evaluated significantly reduced postoperative opioid consumption at 24 h, and that the ESPB was the most effective treatment.
A similar finding was published in another recent meta-analysis by Li J et al., in which the authors evaluated ultrasound-guided PSB, and found a decrease in opioid consumption, as well as improvement in clinical outcomes, such as mechanical ventilation time, total length of ICU stay, and hospital days [25].
Several fascial block techniques are currently utilized, and it is still challenging to determine which is better, given the lack of studies available in the literature. With this evidence, we can conclude that loco regional anesthesia is certainly a key pain control technique in this new era of cardiac surgery, as it spares use of opioids, reduces hemodynamic impact without interfering with the coagulative status of the patient, and enables a prompt fast track.
Conclusion
Fascial plane blocks for cardiac and thoracic surgery represent the future of a well-established ERAS program. These blocks allow good quality analgesia with a simple and safe approach thanks to ultrasound guidance. However, the use of these blocks should be tailored to each patient’s needs, and future studies are needed to better understand their effects on patient outcomes.
Availability of data and materials
Not applicable.
Abbreviations
- ERAS:
-
Enhanced recovery after surgery
- PIP:
-
Parasternal intercostal plane
- LA:
-
Local anesthetic
- IM:
-
Intercostal muscle
- S-ICD:
-
Subcutaneous implantable cardioverter defibrillator
- PECS 1:
-
Interpectoral plane
- PECS II:
-
Pectoserratus plane
- SAPB:
-
Serratus anterior plane block
- IP:
-
In-plane
- PMM:
-
Pectoralis major muscle
- EIM:
-
External intercostal muscle
- TTP:
-
Transversus thoracis plane
- IIM:
-
Internal intercostal muscle
- IMA:
-
Internal mammary artery
- IMV:
-
Internal mammary vein
- LAST:
-
Local anesthetic systemic toxicity
- ICU:
-
Intensive care unit
- PSB:
-
Parasternal block
- RCTs:
-
Randomized controlled trials
- NRS:
-
Numerical rating scale
- PONV:
-
Postoperative nausea and vomiting
- CABG:
-
Coronary artery bypass grafting
- RSB:
-
Rectus sheath block
- RAM:
-
Right rectus abdominis muscles
- LAM:
-
Left rectus abdominis muscles
- RAMS:
-
Rectus abdominis muscles sheath
- PIRS:
-
Pectoralis−intercostal rectus sheath
- LVAD:
-
Left ventricular assist device
- ASRA:
-
American Society of Regional Anesthesia and Pain Medicine
- ESRA:
-
European Society of Regional Anesthesia and Pain Therapy
- VATS:
-
Video−assisted thoracoscopic surgery
- TAP:
-
Transversus abdominis plane
- SAM:
-
Serratus anterior muscle
- ESPB:
-
Erector spinae plane block
- MRI:
-
Magnetic resonance imaging
- ESM:
-
Erector spinae muscle
- TPVB:
-
Thoracic paravertebral block
- TEA:
-
Thoracic epidural anesthesia
- ERACS:
-
Enhanced recovery after cardiac surgery
References
Noss C, Prusinkiewicz C, Nelson G, Patel PA, Augoustides JG, Gregory AJ (2018) Enhanced recovery for cardiac surgery. J Cardiothorac Vasc Anesth 32(6):2760–2770. https://doi.org/10.1053/j.jvca.2018.01.045
Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E et al (2019) Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 55(1):91–115. https://doi.org/10.1093/ejcts/ezy301
Bailey JG, Uppal V. Fascial plane blocks: moving from the expansionist to the reductionist era. Blocs des plans fasciaux : de l’ère expansionniste à l’ère réductionniste. Can J Anaesth. 2022;69(10):1185–1190. https://doi.org/10.1007/s12630-022-02309-x
Elsharkawy H, Pawa A, Mariano ER (2018) Interfascial plane blocks: back to basics. Reg Anesth Pain Med 43(4):341–346. https://doi.org/10.1097/AAP.0000000000000750
Findley T, Chaudhry H, Stecco A, Roman M (2012) Fascia research—a narrative review. J Bodyw Mov Ther 16:67–75
The Centre for Evidence-Based Medicine. Available: https://www.cebm.net/category/ebm-resources/loe/
Sepolvere G, Coppolino F, Tedesco M, Cristiano L (2021) Ultrasound-guided parasternal blocks: techniques, clinical indications and future prospects. Minerva Anestesiol 87(12):1338–1346. https://doi.org/10.23736/S0375-9393.21.15599-3. (Epub 2021 Oct 11 PMID: 34633167)
Droghetti A, Fusco P, Marini M, Harizai F, Scimia P (2019) Ultrasound-guided serratus anterior plane block and parasternal block in cooperative sedation for S-ICD implantation. Pacing Clin Electrophysiol 42(7):1076–1078. https://doi.org/10.1111/pace.13727. (Epub 2019 Jun 4 PMID: 31116436)
King M, Stambulic T, Hassan SMA, Norman PA, Derry K, Payne DM, El Diasty M (2022) Median sternotomy pain after cardiac surgery: to block, or not? A systematic review and meta-analysis. J Card Surg 37(11):3729–3742. https://doi.org/10.1111/jocs.16882. (Epub 2022 Sep 13 PMID: 36098374)
Blanco R (2011) The ‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia 66(9):847–848. https://doi.org/10.1111/j.1365-2044.2011.06838.x. (PMID: 21831090)
Blanco R, Fajardo M, Parras MT (2012) Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim 59(9):470–475. https://doi.org/10.1016/j.redar.2012.07.003. (Epub 2012 Aug 29 PMID: 22939099)
Blanco R, Parras T, McDonnell JG, Prats-Galino A (2013) Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia 68(11):1107–1113. https://doi.org/10.1111/anae.12344. (Epub 2013 Aug 7 PMID: 23923989)
de la Torre PA, García PD, Alvarez SL, Miguel FJ, Pérez MF (2014) A novel ultrasound-guided block: a promising alternative for breast analgesia. Aesthet Surg J 34:198–200
Fusco P, Scimia P, Petrucci E, Carlo DI, S, Marinangeli F. (2017) The ultrasound-guided parasternal block: a novel approach for anesthesia and analgesia in breast cancer surgery. Minerva Anestesiol 83(2):221–222. https://doi.org/10.23736/S0375-9393.16.11546-9. (Epub 2016 Oct 4 PMID: 27701373)
Scimia P, Gentili L, Tedesco M, Fusco P, Sepolvere G (2023) A modified approach to a parasternal block: a case report. A A Pract 17(1):e01644. https://doi.org/10.1213/XAA.0000000000001644. (PMID: 36602918)
Sepolvere G, Tedesco M, Cristiano L (2020) Ultrasound parasternal block as a novel approach for cardiac sternal surgery: could it be the safest strategy? J Cardiothorac Vasc Anesth 34(8):2284–2286. https://doi.org/10.1053/j.jvca.2020.03.014. (Epub 2020 Mar 19 PMID: 32360012)
Costa F, Caruso S, Pascarella G, Nenna A, Grande S, Sarubbi D, Chello M, Agrò FE (2020) Sternotomy debridement in critical patient with difficult predicted airway: can regional anesthesia be the labyrinth exit? Minerva Anestesiol 86(4):462–463. https://doi.org/10.23736/S0375-9393.19.14133-8. (Epub 2019 Dec 9 PMID: 31820875)
Dost B, Taflan MG, Kaya C, Gurz S, Tulgar S (2022) Awake sternal fixation using the ultrasound-guided superficial parasternal intercostal plane block in a patient with cervical spine fracture. Cureus 14(8):e28618. https://doi.org/10.7759/cureus.28618.PMID:36185906;PMCID:PMC9523735
Ueshima H, Kitamura A (2015) Blocking of multiple anterior branches of intercostal Nerves (Th2-6) using a transversus thoracic muscle plane block. Reg Anesth Pain Med 40:388
Sepolvere G, Tognù A, Tedesco M, Coppolino F, Cristiano L (2021) Avoiding the internal mammary artery during parasternal blocks: ultrasound identification and technique considerations. J Cardiothorac Vasc Anesth 35(6):1594–1602. https://doi.org/10.1053/j.jvca.2020.11.007. (Epub 2020 Nov 16 PMID: 33293216)
Fujii S, Roche M, Jones PM, Vissa D, Bainbridge D, Zhou JR (2019) Transversus thoracis muscle plane block in cardiac surgery: a pilot feasibility study. Reg Anesth Pain Med 44:556–560
Aydin ME, Ahiskalioglu A, Ates I, Tor IH, Borulu F, Erguney OD et al (2020) Efficacy of ultrasound-guided transversus thoracic muscle plane block on postoperative opioid consumption after cardiac surgery: a prospective, randomized, double-blind study. J Cardiothorac Vasc Anesth 34:2996–3003
Zhang Y, Li X, Chen S (2021) Bilateral transversus thoracis muscle plane block provides effective analgesia and enhances recovery after open cardiac surgery. J Card Surg 36:2818–2823
Zhang Y, Min J, Chen S. Sensory assessment and block duration of deep parasternal intercostal plane block in patients undergoing cardiac surgery: a prospective observational study. Pain Ther. 2022;11(3):951–958. https://doi.org/10.1007/s40122-022-00403-y. Epub 2022 Jun 25. PMID: 35751781; PMCID: PMC9314528.
Li J et al (2022) Efficacy of ultrasound-guided parasternal block in adult cardiac surgery: a meta-analysis of randomized controlled trials. Minerva Anestesiol 88(9):719–728
King M, Stambulic T, Hassan SMA et al (2022) Median sternotomy pain after cardiac surgery: to block, or not? A systematic review and meta-analysis. J Card Surg 37(11):3729–3742. https://doi.org/10.1111/jocs.16882
Liu G, Gao M, Hu Y, Wang B, Lin Y, Guan Y, Chen G, Zhang P, Hu Y, Cai Q, Qin W (2023) Effects of ultrasound-guided transversus thoracic muscle plane block on postoperative pain and side effects: a systematic review and meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth 37(5):788–800. https://doi.org/10.1053/j.jvca.2022.11.001. (Epub 2022 Nov 5 PMID: 36435722)
Samerchua A, Leurcharusmee P, Supphapipat K, Unchiti K, Lapisatepun P, Maikong N, Kantakam P, Navic P, Mahakkanukrauh P. Optimal techniques of ultrasound-guided superficial and deep parasternal intercostal plane blocks: a cadaveric study. Reg Anesth Pain Med. 2023:rapm-2023–104595. https://doi.org/10.1136/rapm-2023-104595. Epub ahead of print. PMID: 37460213
Harbell MW, Langley NR, Seamans DP, Kraus MB, Carey FJ, Craner RC. Deep parasternal intercostal plane nerve block: an anatomical study. Reg Anesth Pain Med. 2023:rapm-2023–104716. https://doi.org/10.1136/rapm-2023-104716. Epub ahead of print. PMID: 37419507
Padala SRAN, Badhe AS, Parida S, Jha AK (2020) Comparison of preincisional and postincisional parasternal intercostal block on postoperative pain in cardiac surgery. J Card Surg 35(7):1525–1530. https://doi.org/10.1111/jocs.14651. (Epub 2020 Jun 24 PMID: 32579779)
Zou M, Ruan W, Liu J, Xu J (2023) Preemptive parasternal intercostal nerve block for patients undergoing off-pump coronary artery bypass grafting: a double-blind, randomized, controlled trial. Front Cardiovasc Med 18(10):1188518. https://doi.org/10.3389/fcvm.2023.1188518.PMID:37273884;PMCID:PMC10233104
Sepolvere G, Tedesco M, Fusco P, Scimia P, Donatiello V, Cristiano L (2020) Subxiphoid cardiac drainage pain management: could ultrasound rectus sheath block be the answer? Minerva Anestesiol 86(9):994–996. https://doi.org/10.23736/S0375-9393.20.14576-0. (Epub 2020 May 18 PMID: 32420716)
Kang H, chung Ys, choe JW, Woo Yc, Kim sW, Park sJ, et al. application of lidocaine jelly on chest tubes to reduce pain caused by drainage catheter after coronary artery bypass surgery. J Korean Med Sci 2014;29:1398–403
Yamamoto T, Seino Y, Matsuda K, Imai H, Bamba K, Sugimoto A, Shiraishi S, Schindler E (2020) Preoperative implementation of transverse thoracic muscle plane block and rectus sheath block combination for pediatric cardiac surgery. J Cardiothorac Vasc Anesth 34(12):3367–3372. https://doi.org/10.1053/j.jvca.2020.07.041. (Epub 2020 Jul 16 PMID: 32800620)
Everett L, Davis TA, Deshpande SP, Mondal S (2022) Implementation of bilateral rectus sheath blocks in conjunction with transversus thoracis plane and pectointercostal fascial blocks for immediate postoperative analgesia after cardiac surgery. Cureus 14(7):e26592. https://doi.org/10.7759/cureus.26592.PMID:35936156;PMCID:PMC9354918
Toscano A, Balzani E, Capuano P, Vaninetti A, Perrucci C, Simonato E, Rinaldi M, Brazzi L (2022) Awake cardiac surgery using the novel pectoralis-intercostal-rectus sheath (PIRS) plane block and subxiphoid approach. J Card Surg 37(9):2923–2926. https://doi.org/10.1111/jocs.16658. (Epub 2022 Jun 4 PMID: 35665964)
Cibelli M, Brodier EA, Smith FG. Pectoralis-intercostal-rectus sheath (PIRS) plane block with catheters. A new technique to provide analgesia in cardiac surgery. J Cardiothorac Vasc Anesth. 2020;34(3):846–847. https://doi.org/10.1053/j.jvca.2019.09.014. Epub 2019 Sep 18. PMID: 31590939
Harloff MT, Vlassakov K, Sedghi K, Shorten A, Percy ED, Varelmann D, Kaneko T; Nerve Block Working Group. Efficacy of opioid-sparing analgesia after median sternotomy with continuous bilateral parasternal subpectoral plane blocks. J Thorac Cardiovasc Surg. 2023:S0022–5223(23)00177–0. https://doi.org/10.1016/j.jtcvs.2023.02.018. Epub ahead of print. PMID: 37212769
Toscano A, Capuano P, Attisani M, Rinaldi M, Brazzi L (2022) Transversus thoracic plane block and rectus sheath block for left ventricular assist device implantation via full median sternotomy: a case report. J Card Surg 37(7):2115–2119. https://doi.org/10.1111/jocs.16391. (Epub 2022 Mar 7 PMID: 35254689)
Versyck B, Groen G, van Geffen GJ, Van Houwe P, Bleys RL. The pecs anesthetic blockade: a correlation between magnetic resonance imaging, ultrasound imaging, reconstructed crosssectional anatomy and cross-sectional histology. Clin Anat. 2019.
El-Boghdadly K, Wolmarans M, Stengel AD et al (2021) Standardizing nomenclature in regional anesthesia: an ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg Anesth Pain Med 46(7):571–580. https://doi.org/10.1136/rapm-2020-102451
. Jacobs A, Lemoine A, Joshi GP, Van de Velde M, Bonnet F; PROSPECT Working Group collaborators#. PROSPECT guideline for oncological breast surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2020;75(5):664–673. doi:https://doi.org/10.1111/anae.14964
Costa F, Strumia A, Remore LM et al (2020) Breast surgery analgesia: another perspective for PROSPECT guidelines. Anaesthesia 75(10):1404–1405. https://doi.org/10.1111/anae.15161
Kim DH, Kim SJ, Liu J, Beathe J, Memtsoudis SG (2021) Fascial plane blocks: a narrative review of the literature. Reg Anesth Pain Med 46(7):600–617. https://doi.org/10.1136/rapm-2020-101909
Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB (2017) Perioperative breast analgesia: a qualitative review of anatomy and regional techniques. Reg Anesth Pain Med 42(5):609–631. https://doi.org/10.1097/AAP.0000000000000641
Prenter A, Quinn J, Raj N (2015) A prosPECtive technique. Anaesthesia 70:11
Jack JM, McLellan E, Versyck B, Englesakis MF, Chin KJ. The role of serratus anterior plane and pectoral nerves blocks in cardiac surgery, thoracic surgery and trauma: a qualitative systematic review [published online ahead of print, 2020 Feb 16]. Anaesthesia. 2020;https://doi.org/10.1111/anae.15000.doi.
Kumar KN, Kalyane RN, Singh NG et al (2018) Efficacy of bilateral pectoralis nerve block for ultrafast tracking and postoperative pain management in cardiac surgery. Ann Card Anaesth 21:333–338. https://doi.org/10.4103/aca.ACA_15_18
Marcoe GP, Wood H, Marcoe JP, Irfan FB (2019) Multimodal analgesia & regional anesthesia in cardiac surgery. Clin Nutr ESPEN 31:121
Yalamuri S, Klinger RY, Bullock WM, Glower DD, Bottiger BA, Gadsden JC (2017) Pectoral fascial (PECS) I and II blocks as rescue analgesia in a patient undergoing minimally invasive cardiac surgery. Reg Anesth Pain Med 42:764–766. https://doi.org/10.1097/AAP.0000000000000661
Yildirim K, Sertcakacilar G, Hergunsel GO (2022) Comparison of the results of ultrasound-guided thoracic paravertebral block and modified pectoral nerve block for postoperative analgesia in video-assisted thoracoscopic surgery: a prospective, randomized controlled study. J Cardiothorac Vasc Anesth 36(2):489–496. https://doi.org/10.1053/j.jvca.2021.08.014
Luo G, Zhu J, Ni H et al (2021) Pretreatment with pectoral nerve block ii is effective for reducing pain in patients undergoing thoracoscopic lobectomy: a randomized, double-blind, placebocontrolled trial. Biomed Res Int 2021:6693221. https://doi.org/10.1155/2021/669322134
Kaushal B, Chauhan S, Saini K, Bhoi D, Bisoi AK, Sangdup T et al (2019) Comparison of the efficacy of ultrasound-guided serratus anterior plane block, pectoral nerves II block, and intercostal nerve block for the management of postoperative thoracotomy pain after pediatric cardiac surgery. J Cardiothorac Vasc Anesth 33:418–425
Kamal F, Abd El-Rahman A, Hassan RM, Helmy AF (2022) Efficacy of bilateral PECS II block in postoperative analgesia for ultrafast track pediatric cardiac anesthesia. Egypt J Anaesth 38:150–157
Toscano A, Capuano P, Bartoletti L et al (2022) Use of pectoralis type 2 block (PECS II) for awake trans-subclavian transcatheter aortic valve replacement: first experience in two cases. J Cardiothorac Vasc Anesth 36(5):1401–1405. https://doi.org/10.1053/j.jvca.2021.02.034
Johnson M, Doyle Y, McNeill D, McGinley J (2015) A case series of pectoralis blocks in the paediatric cath lab; a novel technique for postoperative analgesia. Reg Anesth Pain Med 40:e196
Munshey F, Ramamurthi RJ, Tsui B. Early experience with PECS 1 block for Port-a-Cath insertion or removal in children at a single institution. Journal of Clinical Anesthesia 2018
Blanco R, Parras T, McDonnell JG, Prats-Galino A (2013) Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia 68(11):1107–1113. https://doi.org/10.1111/anae.12344. (Epub 2013 Aug 7 PMID: 23923989)
Toscano A, Capuano P, Costamagna A, Burzio C, Ellena M, Scala V, Pasero D, Rinaldi M, Brazzi L (2020) The serratus anterior plane study: continuous deep serratus anterior plane block for mitral valve surgery performed in right minithoracotomy. J Cardiothorac Vasc Anesth 34(11):2975–2982. https://doi.org/10.1053/j.jvca.2020.05.021. (Epub 2020 May 27 PMID: 32561247)
Daga V, Narayanan MK, Dedhia JD, Gaur P, Crick H, Gaur A. Cadaveric feasibility study on the use of ultrasound contrast to assess spread of injectate in the serratus anterior muscle plane. Saudi J Anaesth. 2016;10(2):198–201. https://doi.org/10.4103/1658-354X.168825. PMID: 27051373; PMCID: PMC4799614
Biswas A, Castanov V, Li Z, Perlas A, Kruisselbrink R, Agur A, Chan V (2018) Serratus plane block: a cadaveric study to evaluate optimal injectate spread. Reg Anesth Pain Med 43(8):854–858. https://doi.org/10.1097/AAP.0000000000000848. (PMID: 30063656)
Kunigo T, Murouchi T, Yamamoto S et al (2017) Injection volume and anesthetic effect in serratus plane block. Reg Anesth Pain Med 42(6):737–740. https://doi.org/10.1097/AAP.0000000000000649
Hards M, Harada A, Neville I et al (2016) The effect of serratus plane block performed under direct vision on postoperative pain in breast surgery. J Clin Anesth 34:427–431. https://doi.org/10.1016/j.jclinane.2016.05.029. (Epub 2016 Jun 16)
Hanley C, Wall T, Bukowska I, Redmond K, Eaton D, Ní Mhuircheartaigh R, Hearty C (2020) Ultrasound-guided continuous deep serratus anterior plane block versus continuous thoracic paravertebral block for perioperative analgesia in videoscopic-assisted thoracic surgery. Eur J Pain 24(4):828–838. https://doi.org/10.1002/ejp.1533. (Epub 2020 Jan 30 PMID: 31955478)
Viti A, Bertoglio P, Zamperini M, Tubaro A, Menestrina N, Bonadiman S, Avesani R, Guerriero M, Terzi A (2020) Serratus plane block for video-assisted thoracoscopic surgery major lung resection: a randomized controlled trial. Interact Cardiovasc Thorac Surg 30(3):366–372. https://doi.org/10.1093/icvts/ivz289. (PMID: 31808538)
Durant E, Dixon B, Luftig J, Mantuani D, Herring A. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017 Jan;35(1):197.e3–197.e6. doi: https://doi.org/10.1016/j.ajem.2016.07.021. Epub 2016 Jul 19. PMID: 27595172
Chu GM, Jarvis GC (2017) Serratus anterior plane block to address postthoracotomy and chest tube-related pain: a report on 3 cases. A A Case Rep 8(12):322–325. https://doi.org/10.1213/XAA.0000000000000502. (PMID: 28614112)
Sekandarzad MW, Konstantatos A, Donovan S (2019) Bilateral continuous serratus anterior blockade for postoperative analgesia after bilateral sequential lung transplantation. J Cardiothorac Vasc Anesth 33(5):1356–1359
Vig S, Bhan S, Ahuja D et al (2019) Serratus anterior plane block for post-thoracotomy analgesia: a novel technique for the surgeon and anaesthetist. Indian J Surg Oncol 10(3):535–539. https://doi.org/10.1007/s13193-019-00937-2
Jadon A, Jain P (2017) Serratus anterior plane block-an analgesic technique for multiple rib fractures: a case series. Am J Anesth Clin Res 3(1):001–004
Madabushi R, Tewari S, Gautam S et al (2015) Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician 18(3):E421–E424
Rahimzadeh P, Imani F, Faiz SHR et al (2018) Impact of the ultrasound-guided serratus anterior plane block on post-mastectomy pain: a randomised clinical study. Turk Anesteziyoloji ve Reanimasyon Dernegi Dergisi 46(5):388–392. https://doi.org/10.5152/TJAR.2018.86719. (Epub 2018 Sep 4)
. Gautam S, Pande S, Agarwal A, Agarwal SK, Rastogi A, Shamshery C, Singh A. Evaluation of serratus anterior plane block for pain relief in patients undergoing MIDCAB surgery. Innovations (Phila). 2020;15(2):148–154. https://doi.org/10.1177/1556984520908962. PMID: 32352903
Droghetti A, Fusco P, Marini M, Harizai F, Scimia P (2019) Ultrasound-guided serratus anterior plane block and parasternal block in cooperative sedation for S-ICD implantation. Pacing Clin Electrophysiol 42(7):1076–1078. https://doi.org/10.1111/pace.13727. (Epub 2019 Jun 4 PMID: 31116436)
Elsabeeny WY, Ibrahim MA, Shehab NN, Mohamed A, Wadod MA (2021) Serratus anterior plane block and erector spinae plane block versus thoracic epidural analgesia for perioperative thoracotomy pain control: a randomized controlled study. J Cardiothorac Vasc Anesth 35(10):2928–2936. https://doi.org/10.1053/j.jvca.2020.12.047. (Epub 2021 Jan 4 PMID: 33483269)
20Toscano A, Capuano P, Costamagna A, Canavosio FG, Ferrero D, Alessandrini EM, Giunta M, Rinaldi M, Brazzi L. Is continuous Erector Spinae Plane Block (ESPB) better than continuous Serratus Anterior Plane Block (SAPB) for mitral valve surgery via mini-thoracotomy? Results from a prospective observational study. Ann Card Anaesth. 2022 Jul-Sep;25(3):286–292. doi: https://doi.org/10.4103/aca.aca_69_21. PMID: 35799555; PMCID: PMC9387628
Ekinci M, Ciftci B, Gölboyu BE, Demiraran Y, Bayrak Y, Tulgar S (2020) A randomized trial to compare serratus anterior plane block and erector spinae plane block for pain management following thoracoscopic surgery. Pain Med 21(6):1248–1254. https://doi.org/10.1093/pm/pnaa101. (PMID: 32417925)
Gaballah KM, Soltan WA, Bahgat NM (2019) Ultrasound-guided serratus plane block versus erector spinae block for postoperative analgesia after video-assisted thoracoscopy: a pilot randomized controlled trial. J Cardiothorac Vasc Anesth 33(7):1946–1953. https://doi.org/10.1053/j.jvca.2019.02.028. (Epub 2019 Feb 21 PMID: 30930141)
Finnerty DT, McMahon A, McNamara JR, Hartigan SD, Griffin M, Buggy DJ (2020) Comparing erector spinae plane block with serratus anterior plane block for minimally invasive thoracic surgery: a randomised clinical trial. Br J Anaesth 125(5):802–810. https://doi.org/10.1016/j.bja.2020.06.020. (Epub 2020 Jul 11 PMID: 32660716)
Feray S, Lubach J, Joshi GP, Bonnet F, Van de Velde M; PROSPECT Working Group *of the European Society of Regional Anaesthesia and Pain Therapy. PROSPECT guidelines for video-assisted thoracoscopic surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2022;77(3):311–325. https://doi.org/10.1111/anae.15609. Epub 2021 Nov 5. PMID: 34739134; PMCID: PMC9297998
De Cassai A, Boscolo A, Zarantonello F et al (2021) Serratus anterior plane block for video-assisted thoracoscopic surgery: a meta-analysis of randomised controlled trials. Eur J Anaesthesiol 38(2):106–114. https://doi.org/10.1097/EJA.0000000000001290
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ (2016) The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med 41(5):621–627. https://doi.org/10.1097/AAP.0000000000000451)
Chin KJ, El-Boghdadly K. Mechanisms of action of the erector spinae plane (ESP) block: a narrative review. Mécanismes d’action du bloc du plan des muscles érecteurs du rachis (erector spinae, ESP) : un compte rendu narratif. Can J Anaesth. 2021;68(3):387–408. https://doi.org/10.1007/s12630-020-01875-2
Schwartzmann A, Peng P, Maciel MA, Alcarraz P, Gonzalez X, Forero M. A magnetic resonance imaging study of local anesthetic spread in patients receiving an erector spinae plane block. Étude d’imagerie par résonance magnétique de la diffusion d’un anesthésique local chez des patients recevant un bloc du plan des muscles érecteurs du rachis. Can J Anaesth. 2020;67(8):942–948. https://doi.org/10.1007/s12630-020-01613-8
Adhikary SD, Bernard S, Lopez H, Chin KJ (2018) Erector spinae plane block versus retrolaminar block: a magnetic resonance imaging and anatomical study. Reg Anesth Pain Med 43(7):756–762. https://doi.org/10.1097/AAP.0000000000000798
Capuano P, Hileman BA, Martucci G, et al. Erector spinae plane block versus paravertebral block for postoperative pain management in thoracic surgery: a systematic review and meta-analysis [published online ahead of print, 2023 Sep 5]. Minerva Anestesiol. 2023;https://doi.org/10.23736/S0375-9393.23.17510-9
Das S, Saha D, Sen C (2022) Comparison among ultrasound-guided thoracic paravertebral block, erector spinae plane block and serratus anterior plane block for analgesia in thoracotomy for lung surgery. J Cardiothorac Vasc Anesth 36:4386–4392
Zhao H, Xin L, Feng Y. The effect of preoperative erector spinae plane vs. paravertebral blocks on patient-controlled oxycodone consumption after video-assisted thoracic surgery: a prospective randomized, blinded, non-inferiority study. J Clin Anesth. 2020;62:109737. https://doi.org/10.1016/j.jclinane.2020.109737
Athar M, Parveen S, Yadav M et al (2021) A randomized double-blind controlled trial to assess the efficacy of ultrasound-guided erector spinae plane block in cardiac surgery. J Cardiothorac Vasc Anesth 35(12):3574–3580. https://doi.org/10.1053/j.jvca.2021.03.009
Wasfy SF, Kamhawy GA, Omar AH, Abd HF, Aziz El (2021) Bilateral continuous erector spinae block versus multimodal intravenous analgesia in coronary bypass surgery A randomized trial. Egypt J Anaesth 37(1):152–158. https://doi.org/10.1080/11101849.2021.1904548
Nagaraja PS, Ragavendran S, Singh NG et al (2018) Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth 21(3):323–327. https://doi.org/10.4103/aca.ACA_16_18
Krishna SN, Chauhan S, Bhoi D, et al. Bilateral erector spinae plane block for acute post-surgical pain in adult cardiac surgical patients: a randomized controlled trial [published correction appears in J Cardiothorac Vasc Anesth. 2022;36(2):627]. J Cardiothorac Vasc Anesth. 2019;33(2):368–375. https://doi.org/10.1053/j.jvca.2018.05.050
Statzer NJ, Plackis AC, Woolard AA et al (2022) Erector spinae plane catheter analgesia in minimally invasive mitral valve surgery: a retrospective case–control study for inclusion in an enhanced recovery program. Sem Cardiothorac Vasc Anesth 26(4):266–273. https://doi.org/10.1177/10892532221104420
Hoogma DF, Van den Eynde R, Al Tmimi L et al (2023) Efficacy of erector spinae plane block for minimally invasive mitral valve surgery: results of a double-blind, prospective randomized placebo-controlled trial. J Clin Anesth 86:111072. https://doi.org/10.1016/j.jclinane.2023.111072
Karacaer F, Biricik E, Ilgınel M, Tunay D, Topçuoğlu Ş, Ünlügenç H (2022) Bilateral erector spinae plane blocks in children undergoing cardiac surgery: a randomized, controlled study. J Clin Anesth 80:110797. https://doi.org/10.1016/j.jclinane.2022.110797
Macaire P, Ho N, Nguyen V et al (2020) Bilateral ultrasound-guided thoracic erector spinae plane blocks using a programmed intermittent bolus improve opioid-sparing postoperative analgesia in pediatric patients after open cardiac surgery: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 45(10):805–812. https://doi.org/10.1136/rapm-2020-101496
Nair A, Saxena P, Borkar N, Rangaiah M, Arora N, Mohanty PK. Erector spinae plane block for postoperative analgesia in cardiac surgeries- a systematic review and meta-analysis. Ann Card Anaesth. 2023;26(3):247–259. https://doi.org/10.4103/aca.aca_148_22. PMID: 37470522; PMCID: PMC10451138
Adhikary SD, Prasad A, Soleimani B et al (2019) Continuous erector spinae plane block as an effective analgesic option in anticoagulated patients after left ventricular assist device implantation: a case series. J Cardiothorac Vasc Anesth 33:1063–1067
Galacho J, Veiga M, Ormonde L (2020) Erector spinae plane block and altered hemostasis: is it a safe optiona case series. Korean J Anesthesiol 73:445–449
Toscano A, Capuano P, Galatà M, Tazzi I, Rinaldi M, Brazzi L (2022) Safety of ultrasound-guided serratus anterior and erector spinae fascial plane blocks: a retrospective analysis in patients undergoing cardiac surgery while receiving anticoagulant and antiplatelet drugs. J Cardiothorac Vasc Anesth 36(2):483–488. https://doi.org/10.1053/j.jvca.2021.05.037
Fang B, Wang Z, Huang X (2019) Ultrasound-guided preoperative single-dose erector spinae plane block provides comparable analgesia to thoracic paravertebral block following thoracotomy: a single center randomized controlled double-blind study. Ann Transl Med 7:174
Chen N, Qiao Q, Chen R, Xu Q, Zhang Y, Tian Y (2020) The effect of ultrasound-guided intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery: a randomized, double-blinded, clinical trial. J Clin Anesth 59:106–111
Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition) [published correction appears in Reg Anesth Pain Med. 2018;43(5):566. Vandermeuelen, Erik [corrected to Vandermeulen, Erik]]. Reg Anesth Pain Med. 2018;43(3):263–309. https://doi.org/10.1097/AAP.0000000000000763
Kozek-Langenecker SA, Fries D, Gütl M, et al. Lokoregionalanästhesien unter gerinnungshemmender Medikation. Empfehlungen der Arbeitsgruppe Perioperative Gerinnung (AGPG) der Osterreichischen Gesellschaft für Anästhesiologie und Intensivmedizin (OGARI) [Locoregional anesthesia and coagulation inhibitors. Recommendations of the Task Force on Perioperative Coagulation of the Austrian Society for Anesthesiology and Intensive Care Medicine]. Anaesthesist. 2005;54(5):476–484. https://doi.org/10.1007/s00101-005-0827-0
Tsui BCH, Kirkham K, Kwofie MK, et al. Practice advisory on the bleeding risks for peripheral nerve and interfascial plane blockade: evidence review and expert consensus. Recommandations cliniques sur les risques de saignement lors de la réalisation de blocs des nerfs périphériques et de plan interfascial: compte-rendu des données probantes et consensus d’experts. Can J Anaesth. 2019;66(11):1356–1384.https://doi.org/10.1007/s12630-019-01466-w
Kehlet H, Wilmore DW (2005) Fast-track surgery. Br J Surg 92:3–4
Cerfolio RJ, Pickens A, Bass C, Katholi C (2001) Fast-tracking pulmonary resections. J Thorac Cardiovasc Surg 122:318–324
Umari M, Falini S, Segat M et al (2018) Anesthesia and fast-track in video-assisted thoracic surgery (VATS): from evidence to practice. J Thorac Dis 10(Suppl 4):S542–S554. https://doi.org/10.21037/jtd.2017.12.83
Loop T (2016) Fast track in thoracic surgery and anaesthesia: update of concepts. Curr Opin Anaesthesiol 29(1):20–25. https://doi.org/10.1097/ACO.0000000000000282
Huang W, Wang W, Xie W, Chen Z, Liu Y (2020) Erector spinae plane block for postoperative analgesia in breast and thoracic surgery: a systematic review and meta-analysis. J Clin Anesth 66:109900
Ishii H (2014) Cardioprotection with opioids– trusted old friends -clinical science. Curr Pharm Des 20(36):5794–5798
Daniel T. Engelman, Walid Ben Ali, Judson B. Williams et al. Guidelines for perioperative care in cardiac surgery enhanced recovery after surgery society recommendations. JAMA Surg. 2019;154(8):755–766
Wick EC, Grant MC, Wu CL (2017) Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 152(7):691–697. https://doi.org/10.1001/jamasurg.2017.0898BarrLF
Boss MJ, Mazzeffi MA, Taylor BS, Salenger R (2020) Postoperative multimodal analgesia in cardiac surgery. Crit Care Clin 36(4):631–651
Zhang Y, Gong H, Zhan B, Chen S. Effects of bilateral Pecto-intercostal Fascial Block for perioperative pain management in patients undergoing open cardiac surgery: a prospective randomized study. BMC Anesthesiol. 2021;21(1):175. Published 2021 Jun 22.https://doi.org/10.1186/s12871-021-01391-w
Dost B, De Cassai A, Balzani E, Tulgar S, Ahiskalioglu A. Effects of ultrasound-guided regional anesthesia in cardiac surgery: a systematic review and network meta-analysis. BMC Anesthesiol. 2022;22(1):409. Published 2022 Dec 29. https://doi.org/10.1186/s12871-022-01952-7
Acknowledgements
None.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
P.C., G.S., A.T., P.S., S.S., M.T., L.G.: conception and design of the work, draft preparation. P.C., G.M., G.B.: supervising, editing, and final revision of the paper. All author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Capuano, P., Sepolvere, G., Toscano, A. et al. Fascial plane blocks for cardiothoracic surgery: a narrative review. J Anesth Analg Crit Care 4, 20 (2024). https://doi.org/10.1186/s44158-024-00155-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44158-024-00155-5