Abstract
Background
The prevalence, clinical characteristics, management and long-term outcomes of patients with atrial secondary mitral regurgitation (ASMR) are not well described.
Methods
We performed a retrospective, observational study of consecutive patients with grade III/IV MR determined by transthoracic echocardiography. The aetiology of MR was grouped as being either primary (due to degenerative mitral valve disease), ventricular SMR (VSMR: due to left ventricular dilatation/dysfunction), ASMR (due to LA dilatation), or other.
Results
A total of 388 individuals were identified who had grade III/IV MR; of whom 37 (9.5%) had ASMR, 113 (29.1%) had VSMR, 193 had primary MR (49.7%), and 45 (11.6%) were classified as having other causes. Compared to MR of other subtypes, patients with ASMR were on average older (median age 82 [74–87] years, p < 0.001), were more likely to be female (67.6%, p = 0.004) and usually had atrial fibrillation (83.8%, p = 0.001). All-cause mortality was highest in patients with ASMR (p < 0.001), but similar to that in patients with VSMR once adjusted for age and sex (hazard ratio [HR] 0.81, 95% confidence interval [CI] 0.52–1.25). Hospitalisation for worsening heart failure was more commonly observed in those with ASMR or VSMR (p < 0.001) although was similar between these groups when age and sex were accounted for (HR 0.74, 95% CI 0.34–1.58). For patients with ASMR, the only variables associated with outcomes were age and co-morbidities.
Conclusions
ASMR is a prevalent and distinct disease process associated with a poor prognosis, with much of this related to older age and co-morbidities.
Graphical Abstract

Highlights
-
Atrial secondary mitral regurgitation is highly prevalent amongst patients with at least moderate-severe mitral regurgitation.
-
Patients with atrial secondary mitral regurgitation are older, more likely to be female and usually have atrial fibrillation.
-
Outcomes were poor, but much of this was related to advanced age and co-morbidities.
-
Optimal treatments for atrial secondary mitral regurgitation are unknown but should be tailored to the distinct characteristics of this population.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Background
Mitral regurgitation (MR) is a prevalent heart valve disorder, usually classified into two broad categories; either ‘primary’ or ‘secondary’ [1]. Primary MR results from valve apparatus pathology, for example leaflet retraction, or chordae tendineae pathology, whilst secondary MR (SMR) occurs as the result of cardiac structural changes in the absence of significant leaflet pathology, and is most commonly seen in the setting of left ventricular (LV) dilatation and systolic dysfunction. In ventricular secondary mitral regurgitation (VSMR), LV remodelling results in apical-lateral displacement of the papillary muscles causing systolic tethering of the mitral leaflets and failure of morphologically normal leaflets to coapt [2]. However, an increasingly recognised number of patients develop severe MR in the absence of either valve leaflet pathology or LV systolic dysfunction in whom annular dilatation and failure of coaptation is the result of left atrial (LA) remodelling, often associated with atrial fibrillation [3]. Whilst annular dilatation can also contribute to VSMR, atrial secondary mitral regurgitation (ASMR) has been proposed as a distinct clinical entity with a unique pathophysiology. The prevalence, clinical characteristics, management, and long-term outcomes of these patients have not been well described.
Objectives
We aimed to firstly report the prevalence of ASMR in an unselected population with grade III/IV (moderate-severe or severe) MR and secondly, to report and contrast the clinical and echocardiographic characteristics compared to other subtypes of MR. Finally, we sought to describe the long-term outcomes of patients with ASMR compared with other subtypes.
Methods
Study design
We performed a retrospective, observational study to explore the prevalence, characteristics and outcomes of consecutive patients who had grade III/IV MR determined by transthoracic echocardiography at a tertiary cardiology centre. Patients aged ≥ 18 years assessed between 01 January 2012 and 31 December 2013, who had MR graded as III/IV were eligible and identified by searches of the local echocardiography databases using ‘mitral regurgitation’ as the primary search term, and manually evaluated for inclusion. The institutional review board approved the study (IRB #9434 30/07/2021), and in view of the retrospective nature, individual patient consent was waived as appropriate data protection safeguards were in place.
Data sources, definitions and outcomes
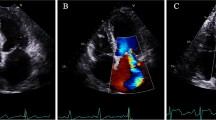
Transthoracic echocardiography images were analysed offline using Medcon (McKesson, Texas, USA). We recorded LA and LV dimensions, volumes and determined left ventricular ejection fraction (LVEF) by Simpson’s biplane method. Mitral annulus dimensions were measured using apical two-chamber, three-chamber and four-chamber imaging planes. Mitral annular area was calculated using the formula: mitral annulus area = 3.14 × commissure-commissure dimension x anteroposterior dimension / 4, as previously published [4, 5]. Mitral regurgitation was graded utilising an integrated approach according to guideline recommendations [6]. For the purposes of analysis, the aetiology of MR was grouped as being either primary (due to degenerative mitral valve disease), VSMR (due to LV dilatation/dysfunction), ASMR (due to atrial dilatation) or other (rheumatic mitral valve disease, infective endocarditis or unclassified). Classification as ASMR required grade III/IV MR, morphologically grossly normal mitral valve leaflets without evidence of prolapse or stenosis, LA dilatation, LV volume within normal limits and LVEF ≥ 50% with no regional wall motion abnormalities. VSMR required grade III/IV MR, morphologically normal mitral valve leaflets, LV dilatation and/or LVEF < 50%, with or without regional wall motion abnormalities, with or without co-existent atrial dilatation.
Clinical data and outcomes were obtained from local electronic care records and linked Office of National Statistics mortality data. Demographic and clinical data included age, sex and co-morbidities, which were hypertension, atrial fibrillation, diabetes mellitus, ischaemic heart disease and cerebrovascular disease. We recorded hospitalisations, surgical or transcatheter mitral valve interventions, and all-cause mortality. All non-elective hospital admissions prior to death or study censorship were classified as either due to or not due to heart failure, defined as the new onset of worsening of signs and symptoms of heart failure with evidence of congestion, with or without the use of intravenous diuretics. Patients were followed up until death with final censorship occurring September 2021.
Statistical analysis
All statistical analyses were done using IBM SPSS Statistics version 26 (IBM Corporation, Armonk, NY). Normality of distribution was explored visually by distribution plots and confirmed using skewness tests. Continuous variables are presented as mean ± standard deviation if normally distributed, as median (interquartile range) if non-normally distributed and discrete variables are presented as number (percentage). Groups were compared using t-tests or one way analysis of covariance for normally distributed continuous data, Mann-Whitey or Kruskal–Wallis H tests for non-normally distributed data, and two-sided Pearson χ2 for categorical variables. Kaplan–Meier analysis was used to plot survival and groups compared using log-rank test. Univariate logistic regression used Cox proportional hazards, for which non-normally distributed data were log10 transformed. We also did sensitivity analyses comparing patients with ASMR and VSMR who did not undergo mitral valve intervention during follow-up. All tests were two-sided, statistical significance was defined as p < 0.05 and no imputation for missing data was made.
Results
Patients
During the study period a total of 2445 imaging datasets were identified by searches of echocardiography databases at our institution. Following manual evaluation and exclusion of serial imaging (repeated) datasets, a total of 388 individuals were identified who had at least grade III/IV MR. According to our criteria, 37 (9.5%) patients were classified as having ASMR, 113 (29.1%) as VSMR, 193 as primary MR (49.7%), whilst 45 (11.6%) were classified as having other aetiologies of mitral valve disease.
Clinical and echocardiographic characteristics
Descriptive data contrasting patients according to aetiology of MR are displayed in Table 1. The median age was 75 (65–83) years and 197 (50.8%) were female. The most common co-morbidities were atrial fibrillation (44.4%), ischaemic heart disease (35.8%) and hypertension (29.6%). Compared to MR of other subtypes, patients with ASMR were on average older (median age 82 [74–87] years, p < 0.001), were more likely to be female (67.6%, p = 0.004) and more frequently had atrial fibrillation (83.8%, p = 0.001). Ischaemic heart disease was more common in patients with VSMR (59.5%, p < 0.001), whilst the distribution of diabetes mellitus and hypertension were similar.
Echocardiography data contrasting patients according to the type of mitral regurgitation are displayed in Table 1. Those with VSMR had more dilated and impaired LV systolic function. The distribution of LA volumes was similar between groups. Mitral annulus dimensions and area were greatest in patients with VSMR, but similar between patients with ASMR and primary MR. Those with primary (75.1%) or other (64.4%) aetiologies of MR were most likely to have 4 + MR, whilst those with ASMR were most likely to have moderate/severe tricuspid regurgitation.
Mitral valve interventions
Overall, 76 (19.6%) patients underwent mitral valve intervention following a median of 270 (71–549) days, of which 39 (10.1%) were surgical mitral valve replacements and 37 (9.5%) were mitral valve repairs. No patients underwent percutaneous mitral valve intervention during the study period. Intervention for mitral valve disease was less commonly undertaken for ASMR compared to other aetiologies of mitral valve disease. Three patients underwent surgical mitral valve repair (annuloplasty ring), with concomitant tricuspid annuloplasty ring (n = 1) surgical atrial fibrillation ablation (n = 1) or both (n = 1). Patients with other aetiologies of MR, including rheumatic valve disease and infective endocarditis were the most likely to undergo mitral valve intervention (35.6%, p = 0.001) and mitral valve replacement (28.9%, p < 0.001). The distribution of mitral valve interventions and additional procedures undertaken at the time of operation are displayed in Additional file 1: Table S1.
Outcomes
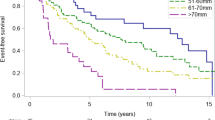
During a mean follow-up of 4.7 ± 3.3 years a total of 245 (63.1%) patients died. Unadjusted all-cause mortality was highest in patients with ASMR, and lowest in those with primary or other aetiologies of MR (p < 0.001) (Fig. 1). Accounting for differences in age and sex between groups, using adjusted Cox proportional hazards regression, survival was not different between patients with ASMR or VSMR (hazard ratio [HR] 0.81, 95% confidence interval [CI] 0.52–1.25), which was also the case in a sensitivity analysis restricted to those who did not undergo mitral valve intervention (HR 1.12, 95% CI 0.70–1.79).
In total 69 (17.8%) patients were hospitalised for worsening heart failure which was more commonly observed in patients with ASMR (24.3%) or VSMR (28.3%) than patients with primary (13.5%) or other (4.4%) aetiologies (p < 0.001) (Fig. 1). Comparing patients with ASMR and VSMR, there was no significant difference in the risk of heart failure hospitalisation once age and sex were accounted for (HR 0.74, 95% CI 0.34–1.58). With similar findings when the analysis was restricted to those who did not undergo mitral valve intervention (HR 0.99, 95% CI 0.43–2.27). The total number of heart failure hospitalisations was highest in patients with ASMR (p = 0.001) with 5 (13.5%) patients having multiple hospitalisations for heart failure.
Within the entire cohort, variables associated with all-cause mortality or hospitalisation for worsening heart failure included age, history of atrial fibrillation or ischaemic heart disease, lower LVEF, higher LA volume, the presence of other significant valvular heart disease and pulmonary and right ventricular systolic pressures (Table 2). Within patients with ASMR, the only variables associated with outcomes were age (HR 1.07 [95% CI 1.02–1.12] per year) and co-morbidities, specifically ischaemic heart disease (HR 2.38 [95% CI 1.13–5.03]) and history of cerebrovascular disease (HR 2.81 [95% CI 1.02–7.72]). In the VSMR group, aside from older age only moderate/severe aortic stenosis and right ventricular systolic pressure were associated with heart failure hospitalisation or all-cause mortality.
Discussion
SMR occurs as the result of cardiac structural or functional changes in the absence of primary valve leaflet pathology. This broad term is usually applied to MR resulting from LV dilatation and/or systolic dysfunction, in which apical-lateral displacement of papillary muscles and systolic tethering cause failure of coaptation [2]. However, SMR is increasingly recognised in the absence of these features. In ASMR, mitral annulus dilatation due to increased LA volumes coupled with insufficient leaflet remodelling and atriogenic leaflet tethering result in failure of coaptation. [7]
Our analysis reveals that ASMR was common within an unselected cohort of patients with at least moderate-severe MR, with a prevalence of 9.5%, broadly in line with previous reports [7, 8]. Consistent with our criteria, those with ASMR had higher LVEF, and smaller LV dimensions compared to those with VSMR. It was notable, however, that the distributions of LA volumes were similar, suggesting LA dilatation may also be a contributor to the development and progression of MR in many patients with VSMR. Patients with ASMR had less elliptical mitral annuluses (as evidenced by higher apical three-chamber/two-chamber diameter ratio) due to dilatation in the antero-posterior direction, although this comparison did not reach statistical significance.
Prior studies reporting the characteristics and outcomes in ASMR have used varying definitions and imaging modalities, and have been limited to comparator populations of either VSMR or primary MR. Applying a definition requiring morphological normal mitral valve leaflets, LA dilatation and normal LV dimensions and function to an unselected population with at least moderate-severe MR, we identified a phenotypically distinct group of patients. Atrial fibrillation was highly prevalent (83.8%), which may be a major driver, or indeed consequence of the underlying pathophysiology. That some individuals had no documented history of paroxysmal or persistent atrial fibrillation suggests this is not a prerequisite for the development of ASMR, rather, an atrial myopathy resulting in deformation or dilatation could underpin this process. These findings were in keeping with prior studies, which have suggested that co-morbidities, particularly atrial fibrillation, hypertension and diabetes mellitus are highly prevalent within this population [9].
In our analysis, all-cause mortality was highest in patients with ASMR, although similar to VSMR, and less favourable compared to primary or other aetiologies once age and sex were accounted for. Prior studies contrasting patients with ASMR and VSMR have suggested that the prognosis of VSMR is less favourable, with differential predictors of outcomes between these distinct groups. This may in part be explained by differing definitions applied across studies, with those with SMR in the current study being classified as having VSMR if they had any degree of LV systolic dysfunction or dilatation [10, 11]. Patients with ASMR had a median age of 82 [74–84] years, and although the age range included patients aged 61–96 years, suggesting it does not solely affect older populations, prognosis in ASMR was most closely related to advanced age and co-morbidities. In VSMR, outcomes were primarily related to the presence of ischaemic heart disease and aortic stenosis. In other studies it has been suggested that LV dilatation and more severe MR are associated with worse prognosis [12], but this was not observed in our data. Heart failure hospitalisation was commonly observed in both ASMR and VSMR, and was significantly higher compared to primary or other aetiologies, and, although the total number of hospitalisations was highest for patients who had ASMR a time to event analysis was similar for ASMR and VSMR once age and sex were accounted for.
For patients with heart failure with reduced ejection fraction, disease modifying pharmacological therapies and cardiac resynchronisation therapy are associated with reductions in LV volumes and the severity of SMR [13]. Persistent MR despite optimised pharmacological and device therapies in the presence of LV systolic dysfunction is associated with worse outcomes [14]. For these patients, surgery to correct valvular dysfunction has not proven to be successful, with two randomised controlled trials of surgical annuloplasty ring in addition to coronary artery bypass grafting [15] and mitral valve repair or chordal-sparing replacement [16] failing to demonstrate improvements in outcomes—perhaps because these interventions target the valvular apparatus, rather than the underlying pathophysiology. More recently, two trials of transcatheter mitral valve repair using the Mitra-Clip (Abbott) device in patients with LV systolic dysfunction and moderate-severe [17] or severe [18] MR reached divergent results, leading to the plausible (but unproven) concept of proportionate and disproportionate SMR [19]. Despite this, there are now guideline recommendations that leaflet treatments for VSMR can be considered in selected patients [20]. Meanwhile, the landscape is advancing rapidly, with several percutaneous annular treatments under investigation, including a multi-centre blinded, sham-controlled study powered for patient-orientated clinical outcomes [21].
In contrast, LA remodelling resulting in secondary MR cannot currently be directly targeted by pharmacological therapies, with management limited to diuretics and rate or rhythm control of atrial fibrillation. Electrical cardioversion has been shown to restore mitral annular dynamics [22], whilst maintenance of sinus rhythm following ablation is associated with a reduction in LA volumes [23] with both approaches associated with a improvements in the degree of ASMR. Few of our patients underwent mitral valve surgery and none underwent transcatheter mitral valve intervention as our cohort predates its widespread availability and although technically feasible, these devices have not been established in this setting. Given that ASMR requires annular dilatation, an annuloplasty device might be a more logical choice. The Carillon (Cardiac Dimensions) mitral valve annuloplasty system reduces annular dimensions and MR in patients with severe [24] and non-severe [25] secondary MR who have LV systolic dysfunction and, despite the absence of randomised trials, is approved for treating ASMR in several regions. Regardless of the approach taken, the average age and burden of co-morbidities in this population should be taken into account when designing future trials.
Limitations
This was a retrospective study, conducted in a single centre and our findings should be interpreted considering this. Three-dimensional transthoracic echocardiography or transoesophageal echocardiography imaging data were not available for all patients, which may have helped further refine classification, although two-dimensional echocardiography for SMR likely represents usual care in many settings. We do not report objective measures of mitral regurgitation severity, however our aim was to contrast the characteristics, management and outcomes of these groups diagnosed according to an integrated approach as part of usual care. Patients received intervention for mitral valve disease at the discretion of their physician or surgeon, and the cohort predated the widespread availability of transcatheter or transvenous mitral valve interventions. Due to a small number of events within each group, multivariable analyses were not undertaken.
Conclusion
Our data suggest that ASMR represents a prevalent disease process associated with a distinct clinical phenotype and a poor prognosis. Much of the increased risk of death or heart failure hospitalisation was related to age and co-morbidities, such that therapeutic strategies for ASMR are urgently required to prove their benefit and should be tailored to the distinct characteristics of this population.
Abbreviations
- ASMR:
-
Atrial secondary mitral regurgitation
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- LA:
-
Left atrial/atrium
- LV:
-
Left ventricular/ventricle
- LVEF:
-
Left ventricular ejection fraction
- MR:
-
Mitral regurgitation
- SMR:
-
Secondary mitral regurgitation
- VSMR:
-
Ventricular secondary mitral regurgitation
References
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005–11.
O’Gara PT, Mack MJ. Secondary mitral regurgitation. N Engl J Med. 2020;383(15):1458–67.
Deferm S, Bertrand PB, Verbrugge FH, et al. Atrial functional mitral regurgitation: JACC review topic of the week. J Am Coll Cardiol. 2019;73(19):2465–76.
Kwan J, Shiota T, Agler DA, et al. Geometric differences of the mitral apparatus between ischemic and dilated cardiomyopathy with significant mitral regurgitation: real-time three-dimensional echocardiography study. Circulation. 2003;107(8):1135–40.
Hyodo E, Iwata S, Tugcu A, et al. Accurate measurement of mitral annular area by using single and biplane linear measurements: comparison of conventional methods with the three-dimensional planimetric method. Eur Heart J Cardiovasc Imaging. 2012;13(7):605–11.
Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography Developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30(4):303–71.
Kagiyama N, Mondillo S, Yoshida K, Mandoli GE, Cameli M. Subtypes of atrial functional mitral regurgitation: imaging insights into their mechanisms and therapeutic implications. JACC Cardiovasc Imaging. 2020;13(3):820–35.
Abe Y, Akamatsu K, Ito K, et al. Prevalence and prognostic significance of functional mitral and tricuspid regurgitation despite preserved left ventricular ejection fraction in atrial fibrillation patients. Circ J. 2018;82(5):1451–8.
Mesi O, Gad MM, Crane AD, et al. Severe atrial functional mitral regurgitation: clinical and echocardiographic characteristics, management and outcomes. JACC Cardiovasc Imaging. 2021;14(4):797–808.
Okamoto C, Okada A, Nishimura K, et al. Prognostic comparison of atrial and ventricular functional mitral regurgitation. Open Heart. 2021;8(1):e001574. https://doi.org/10.1136/openhrt-2021-001574.
Hirji SA, Cote CL, Javadikasgari H, Malarczyk A, McGurk S, Kaneko T. Atrial functional versus ventricular functional mitral regurgitation: prognostic implications. J Thorac Cardiovasc Surg. 2020.
Kim K, Kitai T, Kaji S, et al. Outcomes and predictors of cardiac events in medically treated patients with atrial functional mitral regurgitation. Int J Cardiol. 2020;316:195–202.
Nasser R, Van Assche L, Vorlat A, et al. Evolution of functional mitral regurgitation and prognosis in medically managed heart failure patients with reduced ejection fraction. JACC Heart Fail. 2017;5(9):652–9.
Sannino A, Smith RL 2nd, Schiattarella GG, Trimarco B, Esposito G, Grayburn PA. Survival and cardiovascular outcomes of patients with secondary mitral regurgitation: a systematic review and meta-analysis. JAMA Cardiol. 2017;2(10):1130–9.
Smith PK, Puskas JD, Ascheim DD, et al. Surgical treatment of moderate ischemic mitral regurgitation. N Engl J Med. 2014;371(23):2178–88.
Acker MA, Parides MK, Perrault LP, et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N Engl J Med. 2014;370(1):23–32.
Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018;379(24):2307–18.
Obadia JF, Messika-Zeitoun D, Leurent G, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med. 2018;379(24):2297–306.
Grayburn PA, Sannino A, Packer M. Proportionate and disproportionate functional mitral regurgitation: a new conceptual framework that reconciles the results of the MITRA-FR and COAPT Trials. JACC Cardiovasc Imaging. 2019;12(2):353–62.
Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632. https://doi.org/10.1093/eurheartj/ehab395.
The Carillon Trial—assessment of the carillon mitral contour system in treating functional mitral regurgitation associated with heart failure. https://clinicaltrials.gov/ct2/show/NCT03142152. Accessed 05 Oct 21.
Deferm S, Bertrand PB, Verhaert D, et al. Mitral annular dynamics in AF versus sinus rhythm: novel insights into the mechanism of AFMR. JACC Cardiovasc Imaging. 2022;15(1):1–13.
Gertz ZM, Raina A, Saghy L, et al. Evidence of atrial functional mitral regurgitation due to atrial fibrillation: reversal with arrhythmia control. J Am Coll Cardiol. 2011;58(14):1474–81.
Witte KK, Lipiecki J, Siminiak T, et al. The REDUCE FMR trial: a randomized sham-controlled study of percutaneous mitral annuloplasty in functional mitral regurgitation. JACC Heart Fail. 2019;7(11):945–55.
Witte KK, Kaye DM, Lipiecki J, et al. Treating symptoms and reversing remodelling: clinical and echocardiographic 1-year outcomes with percutaneous mitral annuloplasty for mild to moderate secondary mitral regurgitation. Eur J Heart Fail. 2021;23(11):1971–8. https://doi.org/10.1002/ejhf.2310.
Acknowledgements
This study was conducted at the National Institute of Health Research Cardiovascular Clinical Research Facility at the Leeds Teaching Hospitals NHS Trust.
Funding
This study was supported by a British Heart Foundation Clinical Research Training Fellowship awarded to Dr Sam Straw (FS/CRTF/20/24071).
Author information
Authors and Affiliations
Contributions
KJ, AG and SS collected the data. SS analysed the data. SS produced the first draft of the manuscript. All other authors provided critical revision.
Corresponding author
Ethics declarations
Competing interests
SS is supported by the British Heart Foundation. KJ is supported by the New Zealand Heart Foundation. JG is supported by the National Institute of Health Research. CAC is supported by the Leeds Hospitals Charity. SS has received speaker’s fees and honoraria from AstraZeneca. KKW has received speaker’s fees and honoraria from Medtronic, Cardiac Dimensions, Novartis, Abbott, BMS, Pfizer, Bayer and has received an unconditional research grant from Medtronic. JG has received speaker’s fees and honoraria from Abbott, Medtronic and Microport and has received an unrestricted research grant from Medtronic. None of the other authors have conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Mitral valve procedures divided by aetiology of mitral regurgitation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Straw, S., Gupta, A., Johnson, K. et al. Atrial secondary mitral regurgitation: prevalence, characteristics, management, and long-term outcomes. Echo Res Pract 10, 4 (2023). https://doi.org/10.1186/s44156-023-00015-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44156-023-00015-y