Abstract
Background
Lysophospholipid acyltransferase (LPCAT) is crucial for surfactant biosynthesis. It is encoded by LPCAT genes. We investigated the LPCAT1-rs9728 genotypes in neonatal respiratory distress syndrome (NRDS) cases and their possible association with the cord arterial serum interleukin-10 (IL-10), macrophage migration inhibitory factor (MIF), and vascular endothelial growth factor (VEGF) levels.
Methods
The study included 160 neonates grouped into G1: 60 healthy neonates and G2: 100 NRDS cases. IL-10, MIF, and VEGF levels were measured by their corresponding kits. The Gene JETTM Whole Blood Genomic DNA Purification Mini Kit was used to extract the DNA from the newborn venous blood. The quantitative real-time polymerase chain reaction was carried out for LPCAT1-rs9728 genotyping.
Results
The IL-10 and MIF levels were significantly higher, while VEGF levels were significantly lower in G2 than in G1. The percentages of LPCAT1-rs9728 AA and LPCAT1-rs9728 AG genotypes were significantly higher in G2 than in G1. The IL-10 and MIF levels were significantly higher, while the VEGF levels, birth weight, and APGAR score at 1 and 5 min were significantly lower in neonates with LPCAT1-rs9728 AA genotype than in neonates with LPCAT1-rs9728 AG and LPCAT1-rs9728 GG genotypes and in neonates with LPCAT1-rs9728 AG genotype than in neonates with LPCAT1-rs9728 GG genotype.
Conclusion
There is an association between the LPCAT1-rs9728 AA genotype and its A allele and the NRDS development and severity. Further research may provide a better understanding of this association to help future management.
Similar content being viewed by others
Background
Neonatal respiratory distress syndrome (NRDS) is the most frequent cause of respiratory failure in the first few days after delivery, leading to neonatal mortality [1]. It is a result of the lack of lung surfactant that negatively impacts normal lung function [2]. Pulmonary surfactant is a surface tension-lowering component that comprises lipids (90%) and proteins (10%). Phospholipids represent 80–85% of lipids’ overall mass and are produced and secreted by alveolar type II cells [3]. About 80% of phospholipids are phosphatidylcholine, and the majority of it is dipalmitoyl phosphatidylcholine [4]. The biosynthesis of the lung surfactant and its function are affected by many factors, including genetic, developmental, and environmental ones [5, 6].
Many enzymes contribute to surfactant metabolism. One of them is lysophospholipid acyltransferase (LPCAT), which is crucial for surfactant biosynthesis [7]. The LPCAT1 isozyme is significant for membrane biogenesis and impacts the physiological response of the lung epithelium to damage [5]. It is encoded by the LPCAT1 gene that is placed on chromosome 5p15.33 and is comprising 18 exons [7].
Interleukin-10 (IL-10) is an inhibitory and immunoregulatory cytokine that has a known function in regulating surfactant biosynthesis and metabolism [8]. Its serum levels have been reported as an important indicator of the severity of NRDS [9].
The macrophage migration inhibitory factor (MIF) is a proinflammatory cytokine that is found in the amniotic fluid and is expressed in the placenta and neonatal lungs (alveolar endothelium and macrophages) [10]. It is also expressed in the bronchial epithelial cells, monocytes, and eosinophils [11]. The MIF promotes the synthesis of lots of cytokines such as interleukins 1, 6, and 8, each of which has been related in one way or another to the development of NRDS [12]. Also, high levels of cord blood MIF were reported in cases with NRDS [13].
Vascular endothelial growth factor (VEGF), a crucial regulator of endothelial cells proliferation and angiogenesis, plays an essential role in the development of the lungs and the release of its surfactant. It also augments surfactant protein synthesis. Its cord blood levels were inversely related to the incidence of NRDS [14,15,16].
The current work aimed to investigate the LPCAT1-rs9728 genotypes in cases with NRDS and its possible association with the cord arterial serum levels of IL-10, MIF, and VEGF.
Methods
The current case–control study was carried out in the neonatal intensive care unit, and the woman’s health hospital, Assiut University. It was authorized by the Ethics Board, College of Medicine (IRB: 17,200,578). The study included 160 neonates that were grouped into the following: G1: 60 normal healthy control neonates and G2: 100 neonates with RDS.
The diagnosis of NRDS depended on patient’s clinical signs (tachypnea, retraction, flaring of the nasal alae, grunting, and cyanosis), arterial blood gas analysis (hypoxemia and hypercapnia), and chest x-ray findings (low volume lung with a diffuse reticulogranular pattern and visible air bronchograms) [17].
Complete medical and maternal and family histories were taken from the neonates’ mothers. These included the parents’ age, consanguinity, and maternal diseases, especially diabetes and hypertension, and medications taken by the mother during pregnancy. For each neonate, a full medical examination was taken, and anthropometric measurements were done. APGAR scores were observed at 1, 5, and 10 min after delivery.
The neonate was disqualified from the current research when his guardian refused to contribute or when the neonate exhibited neonatal sepsis, pulmonary infections, congenital anomalies, or any other systemic diseases. Written informed consent was taken from the guardians of all neonates.
Sampling and laboratory assays
The umbilical cord was properly washed with an antiseptic solution before being clamped. Then, 4 ml of arterial cord blood was withdrawn in plain tubes, allowed to clot for 20 min, and centrifuged at 3000 rpm for 5 min. The sera were collected and stored at − 70 °C until the measurement of IL-10, MIF, and VEGF using the human IL-10, MIF, and VEGF ELISA Kits (Thermo Fisher Scientific, USA, cat nos. BMS215-2, EHMIF, and KHG0111, respectively).
Genetic work
Two milliliters of venous blood were withdrawn from each neonate and kept at − 70 °C in an EDTA-containing tube for DNA extraction and the genetic work.
Single-nucleotide polymorphism (SNP) selection
Gene database supplied by the NCBI and the Human Genome Project and the Haploview tool was used to choose the SNP of LPCAT1 [7].
Purification of DNA
According to the manufacturer’s guidelines, the GeneJET™ Whole Blood Genomic DNA Purification Mini Kit (Thermo-Fisher Scientific, USA; Cat. No. 0781) was used to extract the genomic DNA from the venous blood of newborns.
Real-time polymerase chain reaction (RT-PCR) for SNP genotyping
An Applied Biosystems 7500 Fast Real-Time PCR System with version 2.3 software was used for the SNP genotyping. Purified genomic DNA, Pre-Designed 20X TaqMan® SNP Genotyping Assay, and TaqMan™ Universal Master Mix II were the three components essential for the genotyping.
A 96-well optical reaction plate was used for the amplification. Each well contained 12.5 ml of TaqMan™ Universal Master Mix II with no UNG Cat. No. 4440043; 1.25 ml of TaqMan® Pre-Designed SNP Genotyping Assays 20 X, Cat. No. 4351379; 5 ml of pure genomic DNA; and 6.25 ml of 1X TE buffer. Using the default parameters, all analyses were done automatically. The RT-PCR protocol for each reaction was as follows: polymerase activation step for 10 min at 95 °C, denaturation stage for 15 s at 95 °C, and 40–45 annealing/extension cycles at 60 °C for 1 min.
The main components of TaqMan® Pre-Designed SNP Genotyping Assays are two TaqMan® minor groove binder probes, one labeled with VIC® dye to detect the allele 1 sequence and the other with FAM™ dye to detect the allele 2 sequence, along with sequence-specific forward and reverse primers. The TaqMan™ Universal Master Mix II with no UNG contains AmpliTaq Gold® DNA Polymerase, ultra-pure, deoxyribonucleotide triphosphates, ROX™ passive reference dye, and components of an optimized buffer. The Pre-Designed TaqMan® SNP Genotyping Assays and the TaqMan™ Universal Master Mix II with no UNG were manufactured by Thermo-Fisher Scientific (USA). The SNP ID of LPCAT1-rs9728 is at Chr.5:1,461,983 on Build GRCh38.
The type of polymorphism is transversion substitution (A/G), and the relevant sequence is [VIC/FAM]: CAACACGCCAAGAGCCCTGAAATTG[A/G] CTTCGGTTTACTCCATCCCTGTCG.
Statistical analysis
The gathered data were analyzed by SPSS (v.26). A chi-square test was used for the comparison of qualitative data. Student t-test and one-way ANOVA were applied for the comparison of continuous variables. The receiver operating characteristic (ROC) curve was done to investigate the capability of the cord arterial serum levels of IL-10, MIF, and VEGF to differentiate cases with NRDS from healthy neonates. The test was considered significant when its p-value was ≤ 0.05 [18].
Results
The mean of birth weight; APGAR scores at 1, 5, and 10 min; and the percentages of mothers who reported antenatal care and antenatal steroids were significantly lower in G2 than in G1. On the other hand, the percentages of preterm neonates and mothers who had complicated pregnancies were significantly higher in G2 than in G1 (Table 1).
The cord arterial serum IL-10 and MIF levels were significantly high, while the levels of VEGF were significantly low in G2 compared to G1 (Table 2).
The cord arterial serum IL-10 and MIF levels correlated negatively, while VEGF levels correlated positively with birth weight values and APGAR scores at 1, 5, and 10 min (Table 3).
The use of antenatal steroids did not significantly affect the cord IL-10, MIF, or VEGF levels measured in this study, either in the cases or control groups.
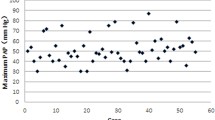
From the ROC curve analysis, the cord arterial serum levels of IL-10 showed an excellent ability to differentiate cases with NRDS from healthy neonates. The cord arterial serum levels of MIF and VEGF showed a good ability to do this (Fig. 1).
The LPCAT1-rs9728 AA and LPCAT1-rs9728AG genotypes were significantly high in the G2 compared to G1 (Table 4 and Fig. 2).
There was significantly lower birth weight and APGAR score at 1 and 5 min in the LPCAT1-rs9728 AA genotype than in the LPCAT1-rs9728 AG and LPCAT1-rs9728 GG genotypes and in the LPCAT1-rs9728 AG genotype than in the LPCAT1-rs9728 GG genotype. There was a significantly lower APGAR score at 10 min in the LPCAT1-rs9728 AA genotype than in the LPCAT1-rs9728 GG genotype (Table 5).
The LPCAT1-rs9728 AA genotype group exhibited significantly higher values for both days of hospitalization (33.04 ± 3 days) and mortality percentage (53.1%) compared to the LPCAT1-rs9728 AG (30.54 ± 3.4 days, 45.4%) and LPCAT1-rs9728 GG (19.44 ± 1.9 days, 22.2%) genotypes, with p-value < 0.001.
The cord arterial serum IL-10 and MIF levels were significantly higher, while the VEGF levels were significantly lower in the neonates with LPCAT1-rs9728 AA genotype than the neonates with LPCAT1-rs9728 AG and LPCAT1-rs9728 GG genotypes and in the neonates with LPCAT1-rs9728 AG genotype than the neonates with LPCAT1-rs9728 GG genotype (p < 0.001 for all) (Fig. 3).
Discussion
The findings of the current work emphasize the previously reported associations of the cord arterial serum IL-10, MIF, and VEGF levels with the development and severity of the NRDS [13,14,15, 19,20,21,22]. Also, our findings are the 1st to report an association between the LPCAT1-rs9728 AA genotype and its A allele with the severity of the NRDS as indicated by their accompanying low APGAR score values at 1, 5, and 10 min and VEGF and the high levels of IL-10 and MIF.
The exact causes of NRDS are yet unknown, but it is believed to be multi-factorial including both genetic and nongenetic causes [23]. Of these factors, pro-inflammatory and anti-inflammatory cytokines are particularly involved in the pathogenesis of RDS [24]. Indeed, cytokines regulate surfactant metabolism in preterm neonates [25]. IL-10 is one of these cytokines that is synthesized by monocytes, macrophages, and T and B lymphocytes [26]. It has inhibitory and immunoregulatory effects on macrophages and plays a role in the pathogenesis of many inflammatory conditions including RDS [9]. The significantly high levels of IL-10 found in the cases with NRDS, the current study, emphasize the results of many previous studies. Capasso et al. reported that the increased IL-10 production was correlated with the RDS severity in preterm neonates [24]. Other studies have reported similar results with an inverse correlation between the cord blood IL-10 and the gestational age at birth [19,20,21].
Macrophage migration inhibitory factor (MIF) is a cytokine released by various cell types and involved in diverse physiological and immunological responses [27]. Its expression begins before birth and has been detected in serum, urine, amniotic fluid, human milk, and cord blood [28]. The MIF role in lung development appears complex and potentially context dependent. In agreement with our findings, Park et al.’s found an association between increased MIF in preterm infants and the development of prematurity-related disorders [29]. Bayraktar et al.’s reported a positive correlation between high cord blood MIF levels and the severity of the RDS in newborns, suggesting a detrimental effect [13]. Interestingly, in vitro experiments contradict these findings, suggesting a positive role for MIF in surfactant production by lung epithelial cells, and even reporting negative impacts of reduced intrapulmonary MIF levels on lung development, including the development of RDS [11].
The VEGF is a significant angiogenic factor that regulates endothelial cell proliferation. Type II alveolar cells are a major source of pulmonary VEGF [30]. VEGF contributes to the release of lung surfactants and pulmonary development, particularly pulmonary circulation [14, 30]. The variations in the VEGF levels in cord plasma help the early detection and treatment of RDS in preterm neonates [22]. Our results are in accordance with many previous studies that reported declines in cord blood VEGF levels in infants with RDS, and these declines correlated with the severity of RDS [14, 15, 22]. In contrast to our findings, Lassus et al. reported a significant increase in the levels of VEGF in tracheal aspirate fluid in the lungs of premature infants with RDS [31].
Genetics and individual variability and heterogeneity play crucial roles in NRDS pathogenicity [32]. The genetic basis of NRDS involves the polymorphism of many genes, including LPCAT1 [7].These genetic polymorphisms are also essential in the mapping, development, and outcomes of NRDS [7, 33]. The increased risk of NRDS in preterm newborns has been associated with mutations and polymorphisms in several genes, particularly in surfactant-associated genes [7]. In the current study, the percentage of LPCAT1-rs9728 AA and LPCAT1-rs9728 AG genotypes were significantly higher in cases suffering from NRDS than in the control group. These results go with Shen et al. who reported a significant difference in the LPCAT1-rs9728 genotypes and its allelic distribution between the NRDS cases and the healthy neonates. Also, they found a protective role of the GG genotype and the G allele of LPCAT1-rs9728 against the development of NRDS. In the same study, RDS cases who had the G allele had a lower risk of intraventricular hemorrhage and a shorter stay in the hospital than those with the A allele [7]. On the other hand, some studies declined the contribution of LPCAT1 polymorphism in the incidence of RDS [34].
The current study showed a significantly lower gestational age and a higher percentage of complicated pregnancy in the NRDS cases than the healthy neonates. As RDS is a complex and multigenic disorder, it is influenced by maternal diseases, gender, ethnicity, and the degree of prematurity [35].
Glucocorticoids significantly enhance the expression of LPCAT1 in the late stages of embryonic development and promote phospholipid biogenesis in alveolar type II cells [33, 36]. The antenatal use of steroids in high-risk pregnancies was found to decrease the incidence and severity of NRDS [37, 38] which goes with our findings.
Conclusion
This study identified a positive association between the LPCAT1-rs9728 AA genotype and both the development and severity of NRDS. Neonates with NRDS and the AA genotype experienced longer hospital stays, higher mortality rates, and higher cord blood levels of IL-10 and MIF, but lower cord blood levels of VEGF, compared to the other two LPCAT1-rs9728 genotypes. This suggests that the A allele may be a potential risk factor for NRDS development.
Recommendations
Further research investigating LPCAT1 genetic polymorphisms in conjunction with other relevant genes, particularly those involved in lung surfactant proteins and lipids, could provide a deeper understanding of the mechanisms underlying NRDS and contribute to developing improved management strategies for this condition.
Availability of data and materials
The datasets analyzed during the current study are available in the European Variation Archive repository, Assembly accession GCA_000001405.27(GRCh38.p12), Chromosome/Contig accession CM000667.2, and The European Bioinformatics Institute < EMBL-EBI.
Abbreviations
- LPCAT1:
-
Lysophosphatidylcholine acyltransferase 1
- IL-10:
-
Interleukin-10
- MIF:
-
Macrophage migration inhibitory factor
- VEGF:
-
Vascular endothelial growth factor
- NRDS:
-
Neonatal respiratory distress syndrome
- RDS:
-
Respiratory distress syndrome
- IL-1:
-
Interleukin-1
- IL-6:
-
Interleukin-6
- IL-8:
-
Interleukin-8
- IRB:
-
Institutional review board
- APGAR:
-
Appearance, pulse, grimace, activity, and respiration
- ELISA:
-
Enzyme-linked immunosorbent assay
- EDTA:
-
Ethylenediamine tetraacetic acid
- SNP:
-
Single-nucleotide polymorphism
- NCBI:
-
National Center for Biotechnology Information
- RT-PCR:
-
Real-time polymerase chain reaction
- UNG:
-
Uracil-N-glycosylase
- VIC:
-
Victoria
- FAM:
-
Fluorescein amidites
- GA:
-
Gestation age
- CS:
-
Cesarian section
- ANOVA:
-
Analysis of variance
- SD:
-
Standard deviation
- ROC curve:
-
Receiver operating characteristic curve
- AUC:
-
Area under the curve
References
Xin H, Wang L, Hao W, Hu H, Li H, Liu B (2023) Lung ultrasound in the evaluation of neonatal respiratory distress syndrome. J Ultrasound Med 42(3):713–721
Yi Z, Tan Y, Liu Y, Jiang L, Luo L, Wang L et al (2022) A systematic review and meta-analysis of pulmonary surfactant combined with budesonide in the treatment of neonatal respiratory distress syndrome. Transl Pediatr 11(4):526
Olmeda B, Martínez-Calle M, Pérez-Gil J (2017) Pulmonary surfactant metabolism in the alveolar airspace: biogenesis, extracellular conversions, recycling. ANN ANAT 209:78–92
Agassandian M, Mallampalli RK (2013) Surfactant phospholipid metabolism. Biochim Biophys Acta Mol Cell Biol Lipids BBA-MOL CELL BIOL L 1831(3):612–625
Lin S, Ikegami M, Moon C, Naren AP, Shannon JM (2015) Lysophosphatidylcholine acyltransferase 1 (LPCAT1) specifically interacts with phospholipid transfer protein StarD10 to facilitate surfactant phospholipid trafficking in alveolar type II cells. JBC 290(30):18559–18574
Goss V, Hunt AN, Postle AD (2013) Regulation of lung surfactant phospholipid synthesis and metabolism. Biochim Biophys Acta Mol Cell Biol Lipids BBA-MOL CELL BIOL L 1831(2):448–458
Shen W, Kuang P, Wang B, Zeng Q, Chen C, Lin X (2020) Genetic polymorphisms of LPCAT1, CHPT1 and PCYT1B and risk of neonatal respiratory distress syndrome among a Chinese Han population. Pediatr Neonatol 61(3):318–324
El-Khaleegy HA, Hassan EM, Shehata HA (2018) Diagnostic performance of point of care ultrasonography in identifying etiology of respiratory distress in neonates. Egypt J Hosp Med 73(5):6753–6762
Jalali SZ, Yousefi F. Serum Levels of Interleukin-10 as a Potential Indicator of Outcome in Premature Neonates with Respiratory Distress Syndrome. Iranian J Neonatol. 2022;13(2):106-11.
Thomas W, Seidenspinner S, Kawczyńska-Leda N, Kramer BW, Chmielnicka-Kopaczyk M, Marx A et al (2008) Systemic fetal inflammation and reduced concentrations of macrophage migration inhibitory factor in the tracheobronchial aspirate fluid of extremely premature infants. Am J Obstet Gynecol. 198(1):64 e1-e6
Kevill KA, Bhandari V, Kettunen M, Leng L, Fan J, Mizue Y et al (2008) A role for macrophage migration inhibitory factor in the neonatal respiratory distress syndrome. J Immunol 180(1):601–608
Munshi UK, Niu JO, Siddiq MM, Parton LA (1997) Elevation of interleukin-8 and interleukin-6 precedes the influx of neutrophils in tracheal aspirates from preterm infants who develop bronchopulmonary dysplasia. Pediatr Pulmonol 24(5):331–336
Bayraktar S, Bayraktar B, Kiliç Ü (2021) Umbilical cord levels of macrophage migration inhibitory factor in neonatal respiratorydistress syndrome. Turk J Med Sci. 51(2):722–6
Moawed AT, El Nashar NA, Margoushy E, Mohamed N (2012) Assessment of cord blood vascular endothelial growth factor levels and circulating CD34+ cells in preterm infants with respiratory distress syndrome. Egypt J Hosp Med 47(1):166–175
Tsao PN, Wei SC, Chou HC, Su YN, Chen CY, Hsieh FJ et al (2005) Vascular endothelial growth factor in preterm infants with respiratory distress syndrome. Pediatr Pulmonol 39(5):461–465
Chen CM, Wang LF (2007) High-dose vascular endothelial growth factor increases surfactant protein gene expressions in preterm rat lung. Early Hum Dev 83(9):581–584
Hiles M, Culpan A-M, Watts C, Munyombwe T, Wolstenhulme S (2017) Neonatal respiratory distress syndrome: chest X-ray or lung ultrasound? A systematic review Ultrasound 25(2):80–91
Nelson K, Christopher F, Milton N (2022) Teach yourself SPSS and STATA. IJAPR 7(6):84–122
Blanco-Quirós A, Arranz E, Solis G, Villar A, Ramos A, Coto D (2000) Cord blood interleukin-10 levels are increased in preterm newborns. Eur J Pediatr 159(6):420–423
El-Khodary AR, Aref WM, Mohamed NG, Ali SM (2005) IL-10 and IL-12 in the cord blood of preterm newborns with respiratory distress syndrome. Alexandria Journal of Pediatrics 19(2):395
Park JY, Kim JY, Cho SJ, Kim YJ, Park HS, Ha EH, Park E. Cord blood IL-10, IL-12 in preterm newborns as predictors of respiratory distress syndrome and bronchopulmonary dysplasia. Clinical and Experimental Pediatrics. 2007;50(3):248-54.
Zhang Y, Shao S, Mu Q, Feng J, Liu J, Zeng C et al (2022) Plasma apelin and vascular endothelial growth factor levels in preterm infants: relationship to neonatal respiratory distress syndrome. J Matern Fetal Neonatal Med 2022:1–8
Ye W, Zhang T, Shu Y, Fang C, Xie L, Peng K et al (2020) The influence factors of neonatal respiratory distress syndrome in southern China: a case-control study. J Matern Fetal Neonatal Med 33(10):1678–1682
Capasso M, Avvisati RA, Piscopo C, Laforgia N, Raimondi F, De Angelis F et al (2007) Cytokine gene polymorphisms in Italian preterm infants: association between interleukin-10–1082 G/A polymorphism and respiratory distress syndrome. Pediatr Res 61(3):313–317
Vayrynen O, Glumoff V, Hallman M (2002) Regulation of surfactant proteins by LPS and proinflammatory cytokines in fetal and newborn lung. Am J Physiol Lung Cell Mol Physiol 282(4):L803–L810
Asadullah K, Sterry W, Volk HD (2003) Interleukin-10 therapy- review of a new approach. Pharmacol Rev 55(2):241–269
Sumaiya K, Langford D, Natarajaseenivasan K, Shanmughapriya S (2021) Macrophage migration inhibitory factor (MIF): a multifaceted cytokine regulated by genetic and physiological strategies. Pharmacol Ther. 233:108024
Ietta F, Todros T, Ticconi C, Piccoli E, Zicari A, Piccione E et al (2002) Macrophage migration inhibitory factor in human pregnancy and labor. Am J Reprod Immunol 48(6):404–409
Park JS, Jun JS, Cho JY, Yeom JS, Seo J-H, Lim JY et al (2022) Difference in macrophage migration inhibitory factor between preterm and term newborns and associating clinical factors: preliminary study. Medicine. 101(34):e30223
Lassus P, Ristimaki A, Ylikorkala O, Viinikka L, Andersson S (1999) Vascular endothelial growth factor in human preterm lung. Am J Respir Crit Care Med 159(5):1429–1433
Lassus P, Turanlahti M, Heikkilä PI, Andersson LC, Nupponen I, Sarnesto A et al (2001) Pulmonary vascular endothelial growth factor and Flt-1 in fetuses, in acute and chronic lung disease, and in persistent pulmonary hypertension of the newborn. Am J Respir Crit Care Med. 164(10):1981–7
Hallman M (2012) Premature birth and diseases in premature infants: common genetic background? J Matern Fetal Neonatal Med 25(sup1):21–24
Bridges JP, Ikegami M, Brilli LL, Chen X, Mason RJ, Shannon JM (2010) LPCAT1 regulates surfactant phospholipid synthesis and is required for transitioning to air breathing in mice. J Clin Investig 120(5):1736–1748
Chen Y-J, Meyer J, Wambach JA, DePass K, Wegner DJ, Fan X et al (2018) Gene variants of the phosphatidylcholine synthesis pathway do not contribute to RDS in the Chinese population. World J Pediatr 14(1):52–56
Somaschini M, Presi S, Ferrari M, Vergani B, Carrera P (2018) Surfactant proteins gene variants in premature newborn infants with severe respiratory distress syndrome. J Perinatol 38(4):337–344
Wang B, Tontonoz P (2019) Phospholipid remodeling in physiology and disease. Annu Rev Physiol 81:165–188
Kajantie E (2023) Point: antenatal corticosteroid treatment in the late preterm period- are the benefits worth the potential risks? Paediatr Perinat Epidemiol 37(1):12
Purandare N, Minchella P, Somayajulu M, Kramer KJ, Zhou J, Adekoya N et al (2021) Molecular mechanisms regulating lysophosphatidylcholine acyltransferase 1 (LPCAT1) in human pregnancy. Placenta 106:40–48
Acknowledgements
The authors express their gratitude to the Research Grant Office, Faculty of Medicine, Assiut University for the participation in this study funding.
Funding
This study was funded by the Research Grant Office, Faculty of Medicine, Assiut University.
Author information
Authors and Affiliations
Contributions
Conceptualization and study design, KMM, OME, and MAE. Supervision, KMM, OME, and MAE. Data curation, KMM, AAS, YFA, and AMF. Investigation, KMM and AAS. Methodology, KMM and AAS. Software, KMM. Validation, KMM and YFA. Visualization, AMA and AMF. Writing — initial draft, KMM, AAS, and YFA. Writing — review and editing, KMM, AAS, and YFA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board at the Faculty of Medicine, Assiut University (IRB: 17200578). A written informed consent was obtained from the parents.
Consent for publications
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohany, K.M., Sayed, A.A., El-Asheer, O.M. et al. The association of LPCAT1-rs9728 polymorphism with cord blood IL-10, MIF, and VEGF levels in neonatal respiratory distress syndrome: a case–control study. Egypt J Bronchol 18, 25 (2024). https://doi.org/10.1186/s43168-024-00273-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00273-2