Abstract
Background
As one of the restrictive lung diseases, scoliosis can be treated by surgical intervention to enhance the pulmonary function of that group of patients. The purpose of the study was to determine the effects of scoliosis correction on pulmonary function after a 6-month duration. Around 30 patients with scoliosis were aged between 10 and 40 years old subjecting to posterior spinal fusion surgery who had been enrolled in the study; all of them were subjected to Cobb’s angle measuring and pulmonary function test before and 6 months after the operation.
Results
Cobb’s angle before the operation was 57.3 ± 13.6°, which significantly corrected and reached up to 21.2 ± 7.2° postoperatively with a mean difference of about 36.13°, P < 0.001. The correlation of Cobb’s angle, forced vital capacity (FVC%), and vital capacity (VC%) was significantly negative. Pulmonary function showed restrictive pattern; forced vital capacity “FVC”, forced expiratory volume 1 “FEV1”, vital capacity “VC”, and forced expiratory flow “FEF 25–75%” were 62.4± 18.06, 65.6±20, 60.7±17.8, and 79.6±28.5, respectively; after 6 months, the reading changed to 60.9± 17.9, 64.04±19.3, 59.16±17.5, and 80.26±28.02 respectively with an insignificant difference, P>0.05.
Conclusion
The pulmonary function showed insignificant changes after 6 months of operation, despite significant changes in Cobb’s angle while the preoperative FVC and VC were inversely correlated with it.
Similar content being viewed by others
Background
Scoliosis is one of the common spine abnormalities. It is considered to be a lateral displacement of the spine and rotation of vertebral bodies. The classification of scoliosis depends on the site of spine affection, either thoracic, lumber, or both [1].
The severity of scoliosis is calculated by measuring “Cobb angle” which is the curvature angle of the spine, hence, increasing the angle by more than 50° denoting significant deformity that needs intervention and correction [2].
Thoracic spine affection either alone or in combination with lumber site has a direct impact on the respiratory and cardiovascular system; hence, the movement of thoracic cavity was limited by the impediment of rib movements, which finally obscure chest wall compliance making the breathing much harder even with normal lung structure [1].
The function of intercostal muscles was limited due to overstretching or inability to stretch during breathing by distortion of the thoracic cage, thus leading to an increase in the work of breathing while the lung is healthy [3, 4]. Early scoliosis surgery can be useful for restoring respiratory function and avoiding curvature magnification of scoliosis [5]. The aim of the work is to determine scoliosis correction operation’s impact on pulmonary functions.
Methods
Prognostic cohort study was conducted on 30 patients aged between 10 and 40 years with idiopathic scoliosis; the patients were admitted to Nasser Institute for Research and Treatment Hospital from November 2018 until December 2019. After meeting the study’s inclusion and exclusion criteria, informed written consent was obtained from the recruited subjects. The study was accepted by the Ethical Committee of the Faculty of Medicine.
The exclusion criteria include smoking, patients with associated comorbidity that affects the lung function, and any contraindication or comorbidity interfering with performing spirometry, e.g., unexplained hemoptysis, pneumothorax, recent myocardial infarction, thoracic, abdominal or cerebral aneurysms, recent eye surgery, recent abdominal or thoracic operations, in addition to other types of scoliosis, e.g., congenital and neuromuscular.
All patients underwent to complete spirometry assessment using the spirometry system (Masterscreen 2001, version 4.5, Erich Jaeger GMBH, Germany). The tests were done before and 20 min after administration of β2-agonist inhaled (400 μg salbutamol), via a metered-dose inhaler. According to American Thoracic Society/European Respiratory Society protocols, the spirometry values were interpreted in all participants [6, 7]. Forced expiratory volume at 1st second “FEV1%”, forced vital capacity “FVC%”, “FEV1/FVC%”, and peak expiratory flow “PEF” 25–75% are measured before surgery and 6 months later.
Surgical intervention
Patients placed on a surgical table under general anesthesia in a prone position. Posterior spinal fusion surgery was done through a midline incision, and then dissection of paravertebral muscle was done to expose the abnormal spine with bilateral implantation of a pedicle screw.
Statistical methods
The statistical analysis was conducted using Minitab 17.1.0.0, windows (Minitab Inc., 2013, Pennsylvania, USA). Continuous data are presented as mean and standard deviation “SD”. Categorical data are presented as number and percentage. The comparison between the two means before and after the intervention was done by paired t-test. The linear relationship between two or more numerical variables was estimated using the Pearson correlation coefficient. All tests were two-tailed, with P considered significant if < 0.05.
Results
Patients had a mean age of 14 years, with a range from 11 to 18 years. Most of them were females (70%), with mean weight and height of about 44.7 kg and 152.6 cm respectively (Table 1).
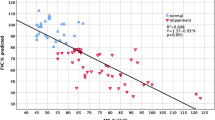
The Cobb angle before the operation was 57.3 ± 13.6°, which significantly correlated with VC and FVC% before the operation in a negative way (Figs. 1 and 2); thus, the angle significantly corrected after the operation to be measured about 21.2 ± 7.2° with a mean difference about 36.13°, P < 0.001 (Table 2 and Fig. 3).
The pulmonary function of patients before the operation showed a restrictive pattern; FVC, FEV1, VC, and FEF 25–75% were 62.4± 18.06, 65.6±20, 60.7±17.8, and 79.6±28.5 respectively, which showed insignificant changes after 6 months of operation (60.9± 17.9, 64.04±19.3, 59.16±17.5, and 80.26±28.02 respectively, with P = 0.15, 0.13, 0.1, and 0.53 respectively) (Table 2).
Discussion
The current study was designed to assess the impact of corrective scoliosis surgery on pulmonary function. Therefore, a prognostic cohort study was conducted on 30 patients admitted to the hospital from November 2018 to December 2019 with idiopathic scoliosis. The pulmonary function was evaluated before the surgery and 6 months later. The present study focuses on the pulmonary function of that group of cases, as the results showed a restrictive pattern in reading. The impact of posterior spinal fusion correction surgery was summarized; hence, the Cobb angle was significantly corrected and reached 21.2 ± 7.2° postoperatively with mean difference of about 36.13°, P < 0.001. Even though the pulmonary function showed an insignificant statistical difference after 6 months of follow-up, that came in consistent with previous studies that reported decreasing in pulmonary function values within 3 months after the operation, but in long-term follow-up, the patients showed significant recovery [8, 9].
A further analysis by Kim et al. did not find any improvement in absolute FVC and FEV1 values after posterior vertebral arthrodesis and costoplasty but showed differences in percentages of estimated values at 2-year follow-up [10].
In the same line, Shi et al., in their study which included 60 patients with thoracic scoliosis (24 males, 36 females), assessed the pulmonary function after thoracoplasty and posterior correction for patients with thoracic scoliosis from June 2001 to June 2010. Their mean age was 17.6 (±5.0) years. All the patients underwent 3-dimensional posterior surgery and thoracoplasty. Pulmonary function was investigated preoperatively, 3 months, and 24 months after surgery. The results showed that the parameters of pulmonary function 2 years after surgery were slightly higher than those of preoperative pulmonary function, but the difference was not significant (P > 0.05). This result indicated that the level of pulmonary function had returned to its level before surgery [2].
A different outcome recorded in a previous study evaluating pulmonary function before and after anterior spinal surgery in adult idiopathic scoliosis included 14 patients, most of whom were female, with a mean age of approximately 26 years (12/14). The mean (±SD) Cobb angle of the thoracic curve was 59° (range 30–119°) for all patients undergoing thoracotomy with anterior or posterior arthrodesis, which showed a significant decrease after the operation to 39° (range 23–88°), with a correction rate of about 31%, P < 0.05. In addition, the FVC decreased substantially from 3.34 (0.80) to 3.13 (0.68), P < 0.05, whereas the FEV1 showed insignificant changes [9].
Wong et al. concluded that the minor decrease in FVC is clinically undetectable especially in patients with appropriate lung function [11]. In addition, Kumano and Tsuyama found a decrease in vital capacity in two patients after anterior surgery and no change in the other two [12].
Another study identified 33 cases that underwent anterior and posterior fusion and no significant differences were observed in vital capacity after long-term follow-up [13].
A different study reported the impact of thoracoplasty on pulmonary function in adolescent idiopathic scoliosis cases; it included 18 patients who were subjected to posterior spinal fusion and costoplasty [14].
Another study, Sánchez-Márquez et al. evaluate the pulmonary function by forced vital capacity (FVC) and forced expiratory volume in 1st second (FEV1) prior to and 1 and 2 years after surgery. The average preoperative absolute FVC was 77.15% while FEV1 was 79.46%. One year post-surgery, mean FVC and FEV1 values were 79.8% and 85.2% respectively, while the mean FVC and FEV1 values were 81.8% and 89.15%, respectively, 2 years post-surgery, and it was concluded that the pulmonary function of patients with scoliosis had a progressive improvement of FVC and FEV1 at 1 and 2 years after surgery.
Respiratory complications of scoliosis are directly related to the severity of the spinal curvature and the associated respiratory muscle weakness. For patients who have mild-to-moderate scoliosis, their lungs are normal, so specific respiratory therapy is not necessary. The goal is to prevent or at least postpone the spinal curvature progression until a definitive correction can be made [1].
The present study reported a significant negative correlation between FVC% and VC% and Cobb angle, as when Cobb angle increases, FVC% and VC% decrease. Information on whether or not these postoperative pulmonary problems are directly correlated with preoperative pulmonary function tests or spinal curve magnitudes was inconsistent [15].
The current results came in consistent with Rekha and Rao whose study included 33 patients with adolescent idiopathic scoliosis and Cobb’s angle more than 40°. Spirometry was done preoperative for all patients. To evaluate pulmonary function, percentage predictions of total lung capacity, forced vital capacity, and forced expiratory volume in 1st second were studied. These variations were compared against Cobb’s angle, hypokyphosis, number of involved vertebrae, and coronal imbalance. The findings indicate that only a significant correlation with decreased lung function is found in the number of involved vertebrae [16].
In the same line, a clinical study with a multicenter database consisting of 858 patients was done by Johnston et al. They found that if Cobb’s angle was more than 80° in the thoracic curves or if thoracic kyphosis was less than 10°, pulmonary function decreases. Unlike a study evaluating PFT in 38 thoracic and thoracolumbar scoliosis patients. The author therefore attempted to correlate pulmonary function with the degree of coronal plane deformity and apical vertebra site and could not find any significant correlation between Cobb’s angle and pulmonary function, but found that FVC was higher in patients with lumbar scoliosis than thoracic one [17].
Conclusion
In the end, we can conclude that after 6 months of posterior spinal fusion correction surgery for scoliotic patients, the pulmonary function showed insignificant changes, despite significant changes in Cobb’s angle while the preoperative FVC and VC were inversely correlated with it.
Availability of data and materials
The datasets used and/or analyzed during the current study are available on reasonable request.
Abbreviations
- FVC:
-
Forced vital capacity
- FEV1:
-
Forced expiratory volume 1
- VC:
-
Vital capacity
- FEF 25–75%:
-
Forced expiratory flow
References
Koumbourlis AC (2006) Scoliosis and the respiratory system. Paediatr Respir Rev 7(2):152–160. https://doi.org/10.1016/j.prrv.2006.04.009
Shi Z, Wu Y, Huang J, Zhang Y, Chen J, Guo K, Li M, Ran B (2013) Pulmonary function after thoracoplasty and posterior correction for thoracic scoliosis patients. Int J Surg 11(9):1007–1009. https://doi.org/10.1016/j.ijsu.2013.05.035
Cooper DM, Rojas JV, Mellins RB, Keim HA, Mansell AL (1984) Respiratory mechanics in adolescents with idiopathic scoliosis. Am Rev Respir Dis 130(1):16–22. https://doi.org/10.1164/arrd.1984.130.1.16
AbdelHalim HA, AboElNaga HH, ElMansoury AM (2015) Effect of truncal obesity on airway resistance. Egyptian J Bronchol 9(2):133–139. https://doi.org/10.4103/1687-8426.158043
Korovessis P, Filos KS, Georgopoulos D (1996) Long-term alterations of respiratory function in adolescents wearing a brace for idiopathic scoliosis. Spine. 21(17):1979–1984. https://doi.org/10.1097/00007632-199609010-00008
Miller M (2005) ATS/ERS task force: standardization of spirometry. Eur Respir J 26(2):319–338. https://doi.org/10.1183/09031936.05.00034805
Sabour Faramawy MA, Abdelhalim HA, Mohamad MM (2019) Use of spirometry as an objective tool in diagnosis and management of airway obstruction among patients diagnosed and treated with chronic obstructive lung disease or asthma. Egypt J Chest Dis Tuberc 68:546–551
Chen S-H, Huang T-J, Lee Y-Y, Hsu RW-W (2002) Pulmonary function after thoracoplasty in adolescent idiopathic scoliosis. Clin Orthop Relat R 399:152–161
Steel HH (1983) Rib resection and spine fusion in correction of convex deformity in scoliosis. JBJS. 65(7):920–925. https://doi.org/10.2106/00004623-198365070-00006
Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K (2005) Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. JBJS. 87:1534–1541
Wong CA, Cole AA, Watson L, Webb JK, Johnston I, Kinnear W (1996) Pulmonary function before and after anterior spinal surgery in adult idiopathic scoliosis. Thorax. 51(5):534–1536. https://doi.org/10.1136/thx.51.5.534
Kumano K, Tsuyama N (1982) Pulmonary function before and after surgical correction of scoliosis. JBJS. 64(2):242–248. https://doi.org/10.2106/00004623-198264020-00016
Korovessis PG, Zielke K (1992) Does the combined ventral derotation system (VDS) followed by Harrington instrumentation improve the vital capacity in patients with idiopathic double major curve pattern scoliosis?: An Analysis of 33 Cases and Review of the Literature. Clin Orthop Relat R 283:130–138
Sánchez-Márquez J, Fernández-Baillo N, García-Fernández A, Quintáns J, Pérez-Grueso F (2010) Effect of thoracoplasty on pulmonary function and esthetics in patients with adolescent idiopathic scoliosis. Revista española de cirugía ortopédica y traumatología 54:156–161
Ledonio CGT, Rosenstein BE, Johnston CE, Regelmann WE, Nuckley DJ, Polly DW Jr (2017) Pulmonary function tests correlated with thoracic volumes in adolescent idiopathic scoliosis. J Orthop Res 35(1):175–182. https://doi.org/10.1002/jor.23304
Rekha YB, Rao VSP (2017) Evaluation of pulmonary function in adolescent idiopathic thoracic scoliosis. Int J Orthop Sci 3(2g):665–670. https://doi.org/10.22271/ortho.2017.v3.i2g.67
Johari J, Sharifudin MA, Ab Rahman A, Omar AS, Abdullah AT, Nor S, Lam WC, Yusof MI (2016) Relationship between pulmonary function and degree of spinal deformity, location of apical vertebrae and age among adolescent idiopathic scoliosis patients. Singap Med J 57(01):33–38. https://doi.org/10.11622/smedj.2016009
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HA analyzed and interpreted the patient data regarding the pulmonary function and the degree of scoliosis. RE took history and examination of the patient and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical Committee Board of Faculty of medicine, Ain Shams University (the reference number is not available). A written informed consent was taken from each patient.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, M.M., Abdelhalim, H.A. & Elamir, R.M.M. Pulmonary function before and after surgical correction of scoliosis. Egypt J Bronchol 15, 25 (2021). https://doi.org/10.1186/s43168-021-00071-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-021-00071-0