Abstract
Background
Lung cancer has a very poor prognosis and high mortality. Positive sputum for malignant and/or atypical cells warrants the need for fibreoptic bronchoscopy. White light bronchoscopy (WLB) is usually unable to detect preinvasive lesions; therefore, autofluorescence bronchoscopy (AFB) was introduced as a gold standard for detecting such lesions. The aim of this work was to investigate the role of I-scan as a screening tool for cancer in smoker patients showing positive sputum cytology.
Results
New suspicious findings under I-scan occurred in 11 patients (36.7%). The overall sensitivity of WLB alone to diagnose malignancy is 23.3%, in contrast to an added sensitivity of 50% when I-scan was combined with white light (p value < 0.05). The specificity of I-scan could not be assessed in the absence of control cases (true negatives). No major complications or deaths occurred. Haemorrhage and bronchospasm were the commonest minor complications.
Conclusions
The addition of I-scan to the routine white light examination can increase the overall sensitivity of bronchoscopic screening in cases of sputum suspicious for malignancy if put in experienced hand. The suggested increase in procedure duration due to the combined use of I-scan and white light bronchoscopy is not associated with life-threatening complications.
Similar content being viewed by others
Background
Lung cancer has less than 15% 5-year survival rates with a mortality rate of more than 90% [1]. Despite the early negative recommendations of the United States Preventive Services Task Force (USPSTF) against screening for lung cancer in both 1985 and 1996 [1], the new published screening studies changed the USPSTF recommendations in 2013 to be grade “B” for annual screening with low-dose computed tomography (LDCT) [2].
Positive sputum for malignant and/or atypical cells, especially in risk group patients, is likely an indicator for the need for fibreoptic bronchoscopy to confirm malignancy with a hope of curable resection [3]. White light bronchoscopy (WLB) is usually unable to detect preinvasive lesions; therefore, autofluorescence bronchoscopy (AFB) was introduced as a gold standard for detecting such lesions [4,5,6]. I-scan technology is a novel endoscopic imaging technique based on a digital contrast process involving three modes of image enhancement: surface enhancement, contrast enhancement and tone enhancement [7, 8]. In contrast to AFB, I-scan depends on the use of one light source giving full-spectrum white light followed by image enhancement on real-time basis, which is easier and more convenient [9].
Methods
In this non-controlled prospective interventional study, we recruited 143 patients between September 2018 and till July 2019, with the inclusion criteria of being a current or former smoker and aged 45 years old or more. Patients with any suspicious lung shadow or infiltrate on plain chest radiographs and CT, in addition to those having any contraindication to bronchoscopy procedure (e.g. recent cardiac events, non-corrected hypoxaemia and severe bleeding disorders), were excluded. In all procedures, we strictly followed the faculty ethics committee standards and a written informed consent was taken from each patient.
We took a representative sputum sample (confirmed by the presence of alveolar macrophages or bronchial epithelial cells [3], which if absent, samples were recollected) from each patient and subjected to cytologic examination for atypical or suspicious cells. Some of each sputum sample was crushed on a clean glass slide by another slide in a rotary pattern. Then, the material was distributed evenly over the slide by making overlapping horizontal strokes producing a smear only slightly thicker than that of the blood. For Papanicolaou stain, slides were fixed immediately in 95% ethyl alcohol, while for May-Grunwald stain, slides were air-dried and fixed in 100% methanol.
After inclusion of 30 patients with positive sputum cytology, recruitment was stopped and all positive patients were subjected to endoscopic examination of whole accessible part of the bronchial tree by high-definition white light bronchoscopy then I-scan mode (using Pentax™ videobronchoscope; Pentax EPK-i5000 High-Definition Video Processor, and Pentax EB-1990i HD+ Bronchoscope) [9, 30]. All suspicious bronchoscopic findings were reported first under high-definition white light (HD/WLB) then under I-scan modes, starting with I-scan 1, then I-scan 2 and lastly I-scan 3, applying the default factory settings for each mode.
“De novo” inspected lesions under any of the I-scan modes, which were not initially noticed under high-definition white light, were clearly reported. Biopsies were taken as indicated using forceps, brush and/or needle with a minimum of five samples [10]. Besides, bronchoalveolar washings by injecting at least 100–120 mL of sterile saline [11] were taken.
Monitoring was continued after the procedure for possible complications which may be major life-threatening (cardiorespiratory arrest, respiratory failure requiring mechanical ventilation, shock, pneumonia, pneumothorax, arrhythmias and pulmonary oedema) or minor non-life-threatening (vasovagal reactions, laryngospasm, bronchospasms, fever, haemorrhage, nausea and vomiting).
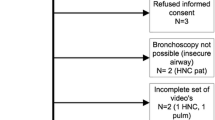
Obtained samples were sent for histopathological and cytological analysis where the pathologist was blind to mode under which biopsy was taken. Pathological results of all sent samples were recorded and categorized as positive or negative for malignancy, and then this was followed by making correlations between pathological yield and the mode under which each biopsy was taken and statistical analysis of all obtained data using the chi-squared test for independence to detect statistically significant difference in sensitivity of each bronchoscopic mode to diagnose malignancy, available at https://www.socscistatistics.com/tests/chisquare2/default2.aspx. Study flow chart is shown in Fig. 1.
Results
Demographics of the study population are grouped in Table 1. Significant endobronchial findings, suspicious for malignancy, were visualized in 21 patients (70%). I-scan showed “de novo” endoscopic suspicious lesions, which were not noticed initially under WLB, in 11 patients, i.e. 36.7% of the study cohort (Fig. 2). The addition of I-scan to WLB gave a significantly higher number of positive endobronchial results (the chi-squared test for independence result was 8.0756. The p value is 0.004486, so this is significant at p < 0.05).
None of the major complications occurred in any of the patients. The only two minor complications that we encountered were haemorrhage (11 patients, 36%) and bronchospasm (4 patients, 13%); however, both were self-limited and had no any clinical significance. No mortalities were found in our study.
Fifty percent of cases (15 patients) showed positive results for malignancy. The distribution of positive pathological results according to histological type is shown in Table 2. Biopsies taken under WLB (without new lesions to be biopsied under I-scan) were positive in 4 patients, in addition to another 3 patients that showed positive results in biopsies taken from both endoscopic lesions seen under both bronchoscopic techniques. Thus, WLB could diagnose all the 7 patients without added benefit from I-scan. Meanwhile, I-scan succeeded to give additional positive results in 8 patients (Fig. 1). Thus, the overall sensitivity of WLB alone is 23.3%, in contrast to an added sensitivity of 50% when I-scan was combined with white light (the chi-square test for independence result was 4.5933; the p value is 0.032097, so this is significant at p < 0.05). The specificity of I-scan could not be assessed in the absence of control cases (true negatives).
Discussion
Many, relatively old, studies have shown a wide range of sensitivities of sputum cytology screening for atypical and/or malignant cells in different study populations with different risks and exposures. Positive results were ranging down to 40% in peripheral tumours and up to 90% in more central cancers [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. We found positive sputum results in 21% of our recruited patients. We could not report our sensitivity rate due to the absence of false negative cases in the absence of a follow-up of sputum negative cases.
Lam et al. studied 181 high-risk patients and detected atypia in 47% of them. Positive cases underwent bronchoscopy and CT scans of the chest with consequent diagnosis of primary lung cancer in 15% of these patients, and almost half of them were at stage I or II. Sputum cytology sensitivity for lung cancer detection was 71% for all histologic types and 100% for squamous cell carcinoma [27]. Because of the “short follow-up” nature of our study, we cannot accurately compare our results to those of the latter study. However, in the same context, we can appreciate that nearly half of our patients who proved to be malignant were of squamous cell type (47%). Obviously, this can be easily anticipated due to the “centrally located” nature of squamous cell carcinomas. In 1985, Risse et al. reported that cytologic typing accuracy was 67% for large cell carcinomas, 73% for adenocarcinomas, 91% for small cell lung cancers and 98% for squamous cell carcinomas. In addition, they pointed to another very important factor to be considered when talking about sputum cytology sensitivity as the concluded that in patients with primary lung cancer, the proportion of correct positive diagnoses increased from 0.47 to 0.87 with one to five sputum specimens examined [28]. We collected and analysed just one sample of sputum from our study patients as this was just a preparatory step before going to the main focus of our research, namely, I-Sacn bronchoscopy.
Bronchoscopic imaging techniques, such as AFB or narrow-band imaging (NBI), facilitate the detection of premalignant lesions and early lung cancer [7, 29]. However, the majority of lung cancer patients are diagnosed in an advanced stage. I-scan, which is an image-digital processing technique, succeeded in the detection of new suspicious endoscopic findings in 67.5% of the patients with a radiologically evident lung mass. Van der Heijden et al. in 2015 did not report significant differences in the average number of tumour sites detected per patient under WLB, HD/WLB, AFB or I-scan modes [9]. While in 2018, the same research group in addition to other investigators from another four centres reported that additional lesions were detected with I-scan in one-third of all patients and 22% of these lesions had a clinical relevant pathology outcome, potentially influencing treatment [30].
For a closely related bronchoscopic modality which is AFB, many studies showed that it increased the sensitivity to diagnose moderate-to-severe dysplasia from 9 to 65% and for CIS, this reached up to 100%. However, AFB did not gain much popularity in daily practice. This may be explained by the decreasing prevalence of central tumours, in combination with the need for a specifically wave-lengthed light source (390–440 nm) [4,5,6, 31,32,33,34,35,36,37,38,39,40,41,42]. Therefore, the results of the published series did not support its general routine use as a diagnostic tool for lung cancer [43].
For another commonly addressed bronchoscopic technique in the field of lung cancer screening which is NBI, a relatively recent meta-analysis published in 2017 and based on four studies found that the pooled sensitivity of NBI to detect lung cancer was 91% (both CIS and invasive lesions) compared to a pooled sensitivity of WLB of 70% [44,45,46,47,48]. In one of these four studies, Herth et al. compared AFB and NBI in the detection of intra-epithelial neoplasia. Both techniques were more sensitive than WLB alone (3.7 and 3.0 times, respectively). However, there was not a significant diagnostic value of combining AFB and NBI together [45]. The commonest histological type that we encountered was squamous cell carcinoma. This may be attributed to the nature of these tumours being more central than other types, and this finding matches many other similar studies; one of the closest was that conducted at the bronchoscopy unit in Abbasia Chest Hospital [49].
Obviously, this presenting study has some limitations. A larger number of cases would give more reliable and reproducible results. A direct comparison of I-scan with other common image processing devices (especially, AFB and NBI) would be very beneficial in terms of drawing conclusions about relative sensitivity and specificity of each technique. Unfortunately, the non-availability of these devices in our department prevented this valuable comparison. The inability to follow up the sputum negative cases hindered the final conclusion for the sensitivity of I-scan.
Conclusion
From all previously mentioned, we can conclude that the addition of I-scan to the routine white light examination can increase overall sensitivity of bronchoscopic screening for lung cancer in smoker patients with positive sputum for malignancy. If put in experienced hand, the suggested increase in procedure duration due to combined use of I-scan and white light bronchoscopy does not lead to major complications or deaths. Minor complications like bleeding and bronchospasm are common in bronchoscopy procedures, but they are usually tolerated and are not associated with significant adverse events.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- USPSTF:
-
United States Preventive Services Task Force
- LDCT:
-
Low-dose computed tomography
- WLB:
-
White light bronchoscopy
- AFB:
-
Autofluorescence bronchoscopy
- CT:
-
Computed tomography
- HD/WLB:
-
High-definition white light bronchoscopy
- NSCLC:
-
Non-small cell lung cancer
- SCLC:
-
Small cell lung cancer
- NBI:
-
Narrow-band imaging
- CIS:
-
Carcinoma in situ
References
Gulland Anne (2014). Global cancer prevalence is growing at “alarming pace,” says WHO. BMJ.;348:1338
Final Update Summary: Lung Cancer: Screening. U.S. Preventive Services Task Force (2015). Available from https://www.uspreventiveservicestaskforce.org /Page/ Document/ UpdateSummaryFinal/lung-cancer-screening?ds=1&s=lung cancer. Accessed 15 Aug 2019.
Jay SJ, Wehr K, Nicholson DP, Smith AL (1980) Diagnostic sensitivity and specificity of pulmonary cytology. Acta Cytol. 24:304–312
Lam S, Kennedy T, Unger M, Miller YE, Gelmont D, Rusch V et al (1998) Localization of bronchial intraepithelial neoplastic lesions by fluorescence bronchoscopy. Chest. 113:696–702
Haussinger K, Becker H, Stanzel F, Kreuzer A, Schmidt B, Strausz J et al (2006) Autofluorescence bronchoscopy with white light bronchoscopy compared with white light bronchoscopy alone for the detection of precancerous lesions: a European randomised controlled multicentre trial. Thorax. 60:496–503
Lam S, MacAulay C, Hung J, LeRiche J, Profio AE, Palcic B (1993) Detection of dysplasia and carcinoma in situ with a lung imaging fluorescence endoscope device. J Thorac Cardiovasc Surg. 105:1035–1040
Tajiri H, Niwa H (2008) Proposal for a consensus terminology in endoscopy: how should different endoscopic imaging techniques be grouped and defined? Endoscopy. 40:775–778
Shinya K, Mitsuhiro F (2010) Novel image-enhanced endoscopy with I-scan technology. World J Gastroenterol. 16:1043–1049
Van der Heijden EH, Hoefsloot WT, van Hees HW, Schuurbiers OC (2015) High definition bronchoscopy: a randomized exploratory study of diagnostic value compared to standard white light bronchoscopy and autofluorescence bronchoscopy. Respir Res. 16:33
Gellert AR, Rudd RM, Sinha G, Geddes DM (1982) Fibreoptic bronchoscopy: effect of multiple bronchial biopsies on diagnostic yield in bronchial carcinoma. Thorax. 37:684–687
Dreisin RB, Albert RK, Talley PA, Kryger MH, Scoggin CH, Zwillich CW (1978) Flexible fiberoptic bronchoscopy in the teaching hospital: yield and complications. Chest. 74:144–149
Koss LG, Melamed MR, Goodner JT (1964) Pulmonary cytology. Acta Cytol. 8:104–113
Umiker WO (1960) Diagnosis of bronchogenic carcinoma: an evaluation of pulmonary cytology, bronchoscopy and scalene lymph node biopsy. Dis Chest. 37:82–90
Allan WB, Whittlesay P (1960) The results of the experimental use of sulfur dioxide in the production of material for cell studies in lung cancer. Ann Intern Med. 52:326–330
Erozan YS, Frost JK (1970) Cytopathologic diagnosis of cancer in pulmonary material: a critical histopathologic correlation. Acta Cytol. 14:560–565
Hinson KFW, Kuper SWA (1963) The diagnosis of lung cancer by examination of sputum. Thorax. 18:350–359
Ng ABP, Horak GC (1983) Factors significant in the diagnostic accuracy of lung cytology. Acta Cytol. 27:397–402
Diguid HLD, Huish DWI (1963). Clinical evaluation of cytodiagnosis in bronchial carcinoma. Br Med J.;ii:287-91
Oswald NC, Hinson KFW, Canti G, Miller AB (1971) The diagnosis of primary lung cancer with special reference to sputum cytology. Thorax. 26:623–631
Cagneten CB, Geller CE, Saenz MC (1976) Diagnosis of bronchogenic carcinoma through cytological examination of the sputum. Acta Cytol. 20:530–536
Bedrossian CWM, Rybka DL (1976) Bronchial brushing during fiberoptic bronchoscopy for the cytodiagnosis of lung cancer: comparison with sputum and bronchial washings. Acta Cytol. 20:446–453
Payne CR, Hadfield JW, Stovin PG, Barker V, Heard BE, Stark JE (1981) Diagnostic accuracy of cytology and biopsy in primary bronchial carcinoma. J Clin Pathol. 34:773–778
Pilotti S, Rilke F, Gribaudi G, Spinelli P (1982) Cytologic diagnosis of pulmonary carcinoma on bronchoscopic brushing material. Acta Cytol. 26:655–660
Castella J, de la Heras P, Puzo C, Martinez C, Lopez A, Cornudella R (1981) Cytology of postbronchoscopically collected sputum samples and its diagnostic value. Respiration. 42:116–121
Johnston WW, Bossen EH (1981) Ten years of respiratory cytopathology at Duke University Medical Center. I. The cytopathologic diagnosis during the years 1970-74. Acta Cytol. 25:103–107
Clee MD, Sinclair DJM (1981) Assessment of factors influencing the results of sputum cytology of bronchial carcinoma. Thorax. 36:143–146
Lam B, Lam SY, Wong MP, Ooi CG, Fong DY, Lam DC et al (2009) Sputum cytology examination followed by autofluorescence bronchoscopy: a practical way of identifying early stage lung cancer in central airway. Lung Cancer. 64:289–294
Risse EK, van't Hof MA, Laurini RN, Vooijs PG (1985) Sputum cytology by the Saccomanno method in diagnosing lung malignancy. Diagn Cytopathol. 1:286–291
Zaric B, Becker HD, Perin B, Jovelic A, Stojanovic G, Ilic MD et al (2009) Narrow band imaging videobronchoscopy improves assessment of lung cancer extension and influences therapeutic strategy. Jpn J Clin Oncol. 39:657–663
Van der Heijden EHFM, Candoli P, Vasilev I, Messi A, Pallarés JP, Yablonskii P et al (2018) Image enhancement technology in bronchoscopy: a prospective multicentre study in lung cancer. BMJ Open Respir Res. 5:e000295
Lam S, MacAulay C, Leriche JC, Ikeda N, Palcic B (1994) Early localization of bronchogenic carcinoma. Diagn Ther Endosc. 1:75–78
Venmans BJ, Van Boxem TJ, Smit EF, Postmus PE, Sutedja TG (1999) Results of two years expenience with fluorescence bronchoscopy in detection of preinvasive bronchial neoplasia. Diagn Ther Endosc. 5:77–84
Vermylen P, Pierard P, Roufosse C, Bosschaerts T, Verhest A, Sculier JP et al (1999) Detection of bronchial preneoplastic lesions and early lung cancer with fluorescence bronchoscopy: a study about its ambulatory feasibility under local anaesthesis. Lung Cancer. 25:161–168
Van Rens MT, Schramel FM, Elbers JR, Lammers JW (2001) The clinical value of lung imaging fluorescence endoscopy for detecting synchronous lung cancer. Lung Cancer. 32:13–18
Shibuya K, Fujisawa T, Hoshino H, Baba M, Saitoh Y, Iizasa T et al (2001) Fluorescence bronchoscopy in the detection of preinvasive bronchial lesions in patients with sputum cytology suspicious or positive for malignancy. Lung Cancer. 32:19–25
Sato M, Sakurada A, Sagawa M, Minowa M, Takahashi H, Oyaizu T et al (2001) Diagnostic results before and after introduction of autofluorescence bronchoscopy in patients suspected of having lung cancer detected by sputum cytology in lung cancer mass screening. Lung Cancer. 32:247–253
Moro-Sibilot D, Jeanmart M, Lantuejoul S, Arbib F, Laverrière MH, Brambilla E et al (2002) Cigarette smoking, preinvasive bronchial lesions, and autofluorescence bronchoscopy. Chest. 122:1902–1908
Beamis JF Jr, Ernst A, Simoff M, Yung R, Mathur P (2004) A multicenter study comparing autofluorescence bronchoscopy to white light bronchoscopy using a non-laser light stimulation system. Chest. 125:148S–149S
Chhajed PN, Shibuya K, Hoshino H, Chiyo M, Yasufuku K, Hiroshima K et al (2005) A comparison of video and autofluorescence bronchoscopy in patients at high risk of lung cancer. Eur Respir J. 25:951–955
Chiyo M, Shibuya K, Hoshino H, Yasufuku K, Sekine Y, Iizasa T et al (2005) Effective detection of bronchial preinvasive lesions by a new autofluorescence imaging bronchovideoscope system. Lung Cancer. 48:307–313
Lam B, Wong MP, Fung SL, Lam DC, Wong PC, Mok TY et al (2006) The clinical value of autofluorescence bronchoscopy for the diagnosis of lung cancer. Eur Respir J. 28:915–919
Ikeda N, Honda H, Hayashi A, Usuda J, Kato Y, Tsuboi M et al (2006) Early detection of bronchial lesions using newly developed videoendoscopy-based autofluorescence bronchoscopy. Lung Cancer. 52:21–27
Bojan Z, Perin B, Becker D, Herth FF, Eberhardt R, Djuric M et al (2011) Autofluorescence imaging videobronchoscopy in the detection of lung cancer: from research tool to everyday procedure. Expert Rev Med Devices. 8:167–172
Zhu J, Li W, Zhou J, Chen Y, Zhao C, Zhang T et al (2017) The diagnostic value of narrow-band imaging for early and invasive lung cancer: a meta-analysis. Clinics. 72(7):438–448
Herth FJ, Eberhardt R, Anantham D, Gompelmann D, Zakaria MW, Ernst A (2009) Narrow-band imaging bronchoscopy increases the specificity of bronchoscopic early lung cancer detection. J Thorac Oncol. 4:1060–1065
Vincent BD, Fraig M, Silvestri GA (2007) A pilot study of narrow-band imaging compared to white light bronchoscopy for evaluation of normal airways and premalignant and malignant airways disease. Chest. 131:1794–1799
Li M, Izumo T, Zhang G, Peng A, Wang C (2014) Narrow-band imaging bronchoscopy improves assessment of tumor extent and affects therapeutic strategy for central lung cancer. Zhonghua Yi Xue Za Zhi. 94:3497–3500
Bojan Z, Branislav P, Aleksandra J, Goran S, Miroslav ID, Ilija A et al (2009) Influence of narrow band imaging (NBI) videobronchoscopy on the assessment of central lung cancer extension and therapeutic decision. Cancer Invest. 27:918–923
Farrag AM, Diab SH, Khalaf AM (2019) Evaluation of lung cancer patterns and bronchoscopicpresentations in patients admitted to Abbasia Chest Hospital. Egypt J Bronchol. 13:49–54
Acknowledgements
Not applicable
Funding
All the procedures were done using Alexandria medicine faculty resources without any impact of this on the design of the study or collection, analysis and interpretation of data.
Author information
Authors and Affiliations
Contributions
AA collected the sputum samples, performed the bronchoscopy procedure, analysed and interpreted the data and was the major contributor in writing the manuscript. DA performed the cytological examination of the sputum and the histological examination of biopsies. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Alexandria medicine faculty ethics committee (IRB NO: 00007555-FWA NO: 00018699) approved this research on 12 April 2018 with a serial number of 0303912. A written informed consent was taken from each patient.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelhady, A.M., Abdallah, D. Role of I-scan technique in screening for lung cancer in smokers with positive sputum cytology. Egypt J Bronchol 14, 2 (2020). https://doi.org/10.1186/s43168-020-00002-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-020-00002-5