Abstract
Background
Systemic sclerosis (SSc)-systemic lupus erythematosus (SLE) overlap syndrome is rarely described in the literature, and its morbidity and mortality remain high after the early onset of pulmonary arterial hypertension (PAH), which determines its severity. The epidemiology of SSc-SLE overlap syndrome is not well known. It is characterized by high clinical polymorphism, making its diagnosis difficult. Through this case, we underline the difficulty and delay in the diagnosis of this syndrome in a country with limited resources, as well as the difficulty of its management given the specificity of the treatment for each pathology and the risk of infections, which could limit their use.
Case presentation
We report the case of a 49-year-old North African female patient, initially followed for SSc for 8 years, whose diversity of symptoms masked the distinct disease. Indeed, her initial clinical presentation was in favor of SSc, but the discovery of a pericardial effusion stimulated us to carry out more investigations and correct the initial diagnosis. The involvement of the myocardium and pericardium, as well as the positive antibody serology tests, make it possible to retain the diagnosis of SSc-SLE overlap syndrome. Despite the introduction of treatment, the patient unfortunately died a month later after developing a multi organ failure following an opportunistic infection.
Conclusions
The management of SSc-SLE overlap syndrome can be complex, requiring good knowledge of these two pathologies, especially in immunocompromised patients with complications. Treatments based on corticosteroids and immunosuppressants may differ from one case to another, making their use difficult in a patient developing a cytomegalovirus (CMV) infection. These patients require urgent treatment before the onset of complications, at the risk of worsening the prognosis, with close collaboration between a cardiologist and an internist, given the multisystem involvement.
Similar content being viewed by others
Background
Systemic sclerosis (SSc) is characterized by multisystem inflammation and fibrosis affecting several systemic organs. This disease can present alone or be associated with other autoimmune diseases, such as systemic lupus erythematosus (SLE), constituting SSc-SLE overlap syndrome. This association is rare and occurs in 7% of SSc cases [1, 2]. Its epidemiology is poorly understood, preferentially affecting young people with a high prevalence of pulmonary hypertension (PAH), interstitial lung damage (ILD), renal damage, and digital ulcers [2]. Cardiac signs constitute one of the multiple manifestations characterizing these two diseases: the endocardium being the least affected [1].
We report, through this case, the appearance of lupus myopericarditis in a patient treated for SSc who was diagnosed with SSc/lupus overlap syndrome.
Case presentation
A North African 49-year-old female patient was admitted to the cardiology department for large pericardial effusion. The history of the disease dates back to 2 weeks before, with the onset of dyspnea at rest associated with edema of the lower limbs. The patient has been known to have diffuse SSc for 8 years, featuring skin changes, Raynaud’s syndrome, ILD, swallowing disorders, arthralgia, and myalgia, as well as positive anti-Scl 70 antibodies and poorly monitored PAH. She had a score of 19 based on the ACR-EULAR criteria for SSc [3] with no history of malar rash, oral ulcers, photosensitivity, or hair loss. She was taking prednisone 5 mg/day and omeprazole 20 mg/day without any treatment for her ILD and PAH due to a lack of resources, with no relevant family or psychosocial history. The initial examination revealed a patient with an altered general condition and a notion of weight loss not quantified during the last months (48 kg on admission); her blood pressure was 100/60 mmHg with a heart rate of 87 bpm, muffled heart sounds, and digital necrosis of the left 4th and 5th fingers. Her skin was thickened and tightened over her face and fingers. She has a slight hair loss, without skin rash, with tenderness mainly on her knees at the slightest movement, and with no signs of inflammation nearby. She presented a slight bilateral decrease in air entry and muffled heart sounds without a heart murmur on auscultation. Her abdomen was soft, and the neurological examination was normal.
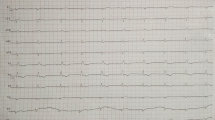
A transthoracic echocardiography (TTE) showed a large pericardial and pleural effusion (Fig. 1). The patient underwent an evacuative pericardial puncture, after pleural puncture, removing 1 L of exudative (total proteins at 36 g/L, normal < 30 g/L) yellow liquid. Its study did not find any cytological (absence of malignant cells, leukocytes at 112 elements/mm3), bacteriological (direct examination as well as negative culture), or anatomopathological abnormalities.
The TTE after control showed a left ventricle with good contractility, a scintillating and hypertrophied appearance, a thickening of the mitral valve leaflets and the interatrial septum, and an altered longitudinal strain suggesting the diagnosis of amyloidosis (Fig. 2). A cardiac MRI was performed showing subepicardial contrast enhancement of the lateral wall (Fig. 3). An initial laboratory assessment found normochromic normocytic anemia (Hb at 10.7 g/Dl), white blood cells at 4360 IU/L with CRP at 10.7 mg/L, normal creatinemia with nephrotic syndrome (proteinuria at 4 g/L, Creat at 9.7 mg/L, < 11.1 mg/L) and microscopic hematuria (red blood cells > 16/mm3) suggesting silent lupus nephritis, and C3 C4 complement lowered. Sputum examination for tuberculosis and serum amyloid assessment came back negative: electrophoresis of plasma proteins, dosage of light chains, Bence-Jones proteinuria, and bone scintigraphy were normal. Tumor markers as well as viral serologies were negative. However, the immunological assessments for SSc and SLE came back positive for anti-nuclear antibodies (ANA), anti-SSA (Ro), anti-double stranded DNA (anti-dsDNA), and anti-topoisomerase (anti-Scl-70).
Thus, the diagnosis of SSc-SLE overlap syndrome was made based on the 2019 criteria of the American College of Rheumatology/European League Against Rheumatism Collaborative Initiative (ACR/EULAR) with a score of 26 featuring a positive ANA, anti-dsDNA, C3 C4 complement lowered, pericardial effusions with pericarditis, arthralgia, and proteinuria > 0.5 g per 24 h [4] and with a Systemic Lupus Erythematosus Disease Activity Index score (SLEDAI score) of 30 featuring a positive anti-dsDNA, C3 C4 complement lowered, pericardial effusions with pericarditis, arthralgia, myalgia, digital necrosis, hematuria > 5 cells/mm3, and proteinuria > 0.5 g per 24 h showing an active flare disease [5]. The patient was immediately started on 1 g of methylprednisolone IV for 3 days, followed by prednisone 1 mg/kg/day orally. Our strategy was to control the inflammatory attack and perform a renal biopsy before introducing an immunosuppressant. The prognosis of the disease was poor given the deterioration of the patient’s general condition, immunosuppression with multisystem involvement, large pericardial effusion at the TTE, the presence of a significant nephrotic syndrome, and positive immunological markers for SSc and lupus in the biology. A renal biopsy was scheduled but the patient presented a decline in visual acuity for which she underwent a fundus examination and an angiogram revealing a cytomegalovirus (CMV) retinitis. Since ganciclovir was not available, she was put on injectable aciclovir. The outcome was unfavorable due to septicemia with multiorgan failure.
Discussion
Autoimmune disorders such as SSc and SLE are characterized by a large clinical polymorphism making their diagnosis difficult. Our patient’s presentation highlighted some of these challenges.
Most of the manifestations such as arthralgia, myalgia, Raynaud’s phenomenon, digital ulcers, pulmonary fibrosis, and the antibodies present in our patient were linked to scleroderma, with a frequency of more than 50% of patients with SSc [6, 7]. However, the discovery of pericardial effusion prompted further investigation.
The confluence of the patient’s symptoms was disguised as separate diseases with a predominance of signs of SSc. The lupus component of overlap syndrome may have been responsible for the myocarditis in this patient. The cardiac involvement of SSc is either primary, linked to the scleroderma itself, or secondary to PAH. Myocardial fibrosis and left diastolic dysfunction are the main features of scleroderma involvement. All other cardiac structures can be affected, notably the pericardium and more rarely the endocardium [8]. Regarding lupus, it is frequently complicated by cardiac abnormalities such as valvular disease, most often mitral regurgitation, pericardial disease, usually asymptomatic effusion, myocardial dysfunction, and coronary artery disease. Lupus myocarditis is rare [9].
In SSc, treatment is targeted to the organ involved, such as interstitial lung disease, skin fibrosis, pulmonary hypertension, and kidney failure [8]. Immunosuppressants are used specifically to control pulmonary and skin complications. In lupus, treatment is based on corticosteroid therapy [9]. In our patient, it was decided to start corticosteroid therapy after elimination of an infection and then to perform a renal biopsy before starting immunosuppressants. On the renal level, the patient had subacute nephrotic proteinuria with no renal symptoms, raising the possibility of developing silent lupus nephritis. Affecting more than half of lupus patients, the Gouda study [10] showed that this group of patients was associated with a higher rate of glomerular lesions on renal biopsy, underlining the interest of carrying it out in any clinically asymptomatic patient. The diagnosis of overlap syndrome allows, in cases of lupus associated with scleroderma, the introduction of hydroxychloroquine and limiting the dose of corticosteroid therapy [11]. The evolution was initially favorable following the introduction of corticosteroids and then marked by the death of the patient who developed a cytomegalovirus infection. CMV infection have been described as exacerbating and starting off SLE as in the clinical case of Amel et al. [12]. The patient was put on corticosteroids and antivirals before developing cerebral vasculitis and only improved after the introduction of immunosuppressants. The diagnosis of this infection is difficult and often combines febrile polyarthralgia and enteritis [13], which is what we found in our patient. Positive anti-dsDNA antibody, hypocomplementemia, high SLEDAI-2 K score, and musculoskeletal involvement were significant clinical markers in SLE with CMV infections, with higher disease activity and poorer outcome [14].
Our case highlights the importance of systematically searching for other associated systemic diseases such as SLE, especially in the presence of suggestive clinical signs such as pericardial effusion or lupus nephritis. The patient’s clinical polymorphism was the cause of a diagnostic delay, in addition to difficulty in accessing certain examinations and the lack of resources in our hospital. Multidisciplinary collaboration is essential for rapid and complete care: our patient was quickly relieved for her epicardial effusion but we were limited for the etiological treatment given her fragile condition as well as our lack of experience in the handling of corticosteroids and for the rest of the assessment. Also, the hypothesis that she could have developed a macrophage activation syndrome was possible given the picture of unexplained multiorgan failure in immunocompromised patients with the appearance and persistence of fever under aciclovir 3 days after the start of treatment [15]. Awasthi and Upreti wrote about a similar case of SLE in which they found both EBV and CMV infections, high-grade fevers that came on quickly, and multiorgan failure despite aggressive treatment that started early [16].
Conclusions
The management of SSc-SLE overlap syndrome can be complex and requires a better therapeutic approach given the high risk of morbidity and mortality associated with these diseases, even though their management remains challenging for patients with compromised immune systems. Interactions between specialties could accelerate the diagnosis and improve the use of corticosteroids and immunosuppressants. Depending on the specificity of each pathology, early detection of their complications is crucial.
Availability of data and materials
Data supporting the study results can be provided followed by request sent to the corresponding author’s e-mail.
Abbreviations
- ACR/EULAR:
-
American College of Rheumatology/European League Against Rheumatism Collaborative Initiative
- ANA:
-
Anti-nuclear antibodies
- Anti-dsDNA:
-
Anti-double stranded
- Anti-Scl-70:
-
Anti-topoisomerase
- CMV:
-
Cytomegalovirus
- EKG:
-
Electrocardiogram
- HS score:
-
Hemophagocytic syndrome score
- ILD:
-
Interstitial pulmonary disease
- MRI:
-
Magnetic resonance imaging
- PAH:
-
Pulmonary arterial hypertension
- SSc:
-
Systemic sclerosis
- TTE:
-
Transthoracic echocardiogram
References
Balbir-Gurman A, Braun-Moscovici Y (2011) Scleroderma overlap syndrome. Isr Med Assoc J 13:14–20
Alharbi S, Ahmad Z (2018) Bookman AA Epidemiology and survival of systemic sclerosis-systemic lupus erythematosus overlap syndrome. J Rhumatol 45(10):1406–1410
Van den Hoogen F, Khanna D et al (2013) Classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum 65(11):2737–2747. 2013
Aringer M, Costenbader K, Daikh D (2019) 2019 European league against rheumatism/american college of rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol 71(9):1400–1412
Mikdashi J, Nived O (2015) Measuring disease activity in adults with systemic lupus erythematosus: the challenges of administrative burden and responsiveness to patient concerns in clinical research. Arthritis Res Ther 17(1):183. https://doi.org/10.1186/s13075-015-0702-6
Denton CP, Khanna D (2017) Systemic sclerosis. Lancet 390(10103):1685–1699
Van den Hoogen F, Khanna D, Fransen J (2013) 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 72(11):1747–1755
Allanore Y, Kahan A (2006) Heart involvement in systemic sclerosis. Presse Med 35(12 Pt 2):1938–42. https://doi.org/10.1016/s0755-4982(06)74928-4. PMID: 17159720
Ben Achour T, Sayhi S, Boussetta N, Ben Abdelhafidh N, Ajili F, Louzir B (2018) Cardiac manifestations during lupus erythematosus: a study of 80 cases. J Int Med 39:A105–A106. https://doi.org/10.1016/j.revmed.2018.10.016
Gouda W et al (2022) Silent lupus nephritis: renal histopathological profile and early detection with urinary monocyte chemotactic protein 1. Open Access Rheumatol 14(14):161–170
Vermersch C, Osdoit S, Renou F, Bagny K (2019) Le scléro-lupus, une série de 5 cas d’une entité rare. Annales de Dermatologie et de Vénéréologie 146(12):A292. https://doi.org/10.1016/j.annder.2019.09.480
Amel R et al (2016) Systemic lupus erythematous revealed by cytomegalovirus infection. Pan Afr Med J 15(24):241. https://doi.org/10.11604/pamj.2016.24.241.8988. PMID:27800096
Declerck L, Queyrel V, Morell-Dubois S, Dewilde A, Charlanne H, Launay D, Lambert M, Hachulla E, Hatron PY (2009) Cytomegalovirus and systemic lupus: severe infection and difficult diagnosis. Rev Med Interne 30(9):789–793
Tsai WP et al (2012) Cytomegalovirus infection causes morbidity and mortality in patients with autoimmune diseases, particularly systemic lupus: in a Chinese population in Taiwan. Rheumatol Int 32(9):2901–2908. https://doi.org/10.1007/s00296-011-2131-4. Epub 2011 Sep 7
Gouda W et al (2021) Macrophage activation syndrome triggered by systemic lupus erythematosus flare: successful treatment with a combination of dexamethasone sodium phosphate, intravenous immunoglobulin, and cyclosporine: a case report. J Med Case Rep 15(1):497. https://doi.org/10.1186/s13256-021-03072-1
Awasthi S, Upreti S (2020) Macrophage activation syndrome in a patient with systemic lupus erythematosus (SLE) and dual viremia. J Community Hosp Intern Med Perspect 10(5):470–474
Acknowledgements
We would like to acknowledge the radiology department for their involvement with this case.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
GB and SZ performed the examination of the patient and were involved in the review of literature and writing the manuscript. AB helped in writing the manuscript, supervised by AD and RH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from the patient involved in this case.
Consent for publication
Written informed consent has been obtained from the patient(s) to publish this paper.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bennani, G., Zahri, S., Boulahnach, A. et al. Myopericarditis revealing a systemic sclerosis-systemic lupus erythematosus overlap syndrome complicated by fatal cytomegalovirus infection: a case report. Egypt Rheumatol Rehabil 51, 32 (2024). https://doi.org/10.1186/s43166-024-00265-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-024-00265-6