Abstract
Background
Lateral elbow pain is a prevalent musculoskeletal disorder affecting the elbow’s epicondyle region. One form of lateral elbow pain is lateral epicondylitis, which is a degenerative disorder of the musculotendinous system. Adequate levels of vitamin D are essential for maintaining musculoskeletal health. Our study aimed to assess the role of vitamin D in lateral epicondylitis among Egyptians.
Results
Our research revealed that there is a significant correlation between vitamin D deficiency and lateral epicondylitis. Patients with vitamin D deficiency displayed worse patient-rated tennis elbow evaluation score (PTREE), visual analog scale score (VAS), and grip strength. These findings indicate a statistically significant association between lateral epicondylitis patients with deficient vitamin D and each of the PTREE scores (p < 0.001), VAS score (p < 0.001), and hand grip strength (p < 0.001).
Conclusion
The etiology of lateral epicondylitis is not yet fully understood. However, our study provides evidence supporting the notion that low levels of vitamin D may be one of the risk factors in the etiology of lateral epicondylitis among Egyptians.
Similar content being viewed by others
Background
Lateral epicondylitis, a musculotendinous degenerative disorder of the lateral epicondyle of the humerus [1], is a condition that arises from overuse or repetitive use of the forearm extensor muscles leading to tendinopathy [2]. It is a work-related condition that poses a significant public health concern [3].
The prevalence of lateral epicondylitis is approximately 1–3% of the population in the age group of 35–54 years [2] and affects 50% of tennis players, leading it to be commonly referred to as “tennis elbow” [4]. Heavy manual laborers and those whose jobs require repetitive movements, such as forceful forearm pronation or supination, and fine motor skills, such as computer usage, are at a higher risk of developing this condition [5].
The etiology of lateral epicondylitis is not fully understood, but tenocyte proliferation and structurally abnormal collagen production are believed to be the main factors contributing to its development. Severe cases of lateral epicondylitis can result in pain in the epicondyle, which can extend to the shoulder and wrist [6].
An accurate medical history and provocative tests are necessary for the diagnosis of lateral epicondylitis [7]. Clinicians may use radio diagnostic imaging, such as musculoskeletal ultrasound and magnetic resonance imaging, to make a more precise diagnosis [8].
Vitamin D plays a crucial role in maintaining a healthy bone microenvironment and balanced bone turnover [6]. Its role in regulating the metabolism of bone and minerals is critical to musculoskeletal health, with tenocytes containing vitamin D receptors [9]. Globally, vitamin D deficiency affects both adults and children [10] and is associated with diseases such as osteoporosis, rickets, metabolic diseases, and cardiovascular diseases [11].
Other studies have investigated the effect of low vitamin D levels on calcium metabolism and bone pathologies in lateral epicondylitis [12]. To assess the role of vitamin D in lateral epicondylitis among Egyptians, our study was conducted.
Approaches
Patients and study design
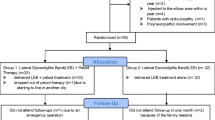
A cross-sectional study sample of 90 non-smoking adult patients affected by lateral epicondylitis was chosen from the outpatient clinics of the University Hospital. Patients with a history of autoimmune or rheumatological diseases, current pregnancies, local infections, endocrinological diseases, chronic obstructive pulmonary disease, malignancy, and severe uncontrolled illness were excluded from the study. The study received approval from the Research Ethics Committee of our university, and all participants provided informed written consent.
Assessment of clinical condition
Each patient underwent a comprehensive medical assessment, including a general and local examination. Pain levels were evaluated using a visual analog scale (VAS), where participants selected a whole number between 0 and 10, with zero indicating the absence of pain and 10 indicating extreme pain [13]. The grip strength of the affected hand was measured using a hand dynamometer. Patients were seated, with abducted shoulders, neutral elbows, and flexed elbows at 90°, with a 30-s interval between measurements. The mean value of three measurements was calculated in kilograms [14]. To evaluate forearm pain and disability in patients with lateral epicondylitis, the PRTEE questionnaire, consisting of 15 items, was employed. The questionnaire employs a numerical scale from 0 to 10 to rate the average pain or difficulty experienced during various activities that are often painful in tennis elbow. The PRTEE questionnaire comprises two subscales.
The Patient-Rated Tennis Elbow Evaluation (PRTEE) questionnaire is a validated tool used to assess pain and functional limitations associated with tennis elbow. The pain subscale of the PRTEE questionnaire includes five items, each rated on a scale from 0 (no pain) to 10 (worst pain), with items assessing resting pain, pain during repetitive arm movements, discomfort during activities such as carrying a plastic grocery bag, the lowest point of pain, and pain at its height. The pain subscale scores range from 0 to 50, with a score of 0 indicating no pain and a score of 50 indicating the worst possible pain.
The PRTEE questionnaire also includes a two-function subscale that measures difficulty in performing specific activities and usual activities. The specific activities subscale includes six items, such as turning a doorknob or key, lifting a full cup of coffee or milk, and opening a jar. The usual activities subscale includes four items, such as personal hygiene, household duties, work, and recreation or sports. Each item is rated on a scale from 0 (no difficulty) to 10 (unable to do). The function subscale scores range from 0 to 50, with a score of 0 indicating no difficulty and a score of 50 indicating the greatest difficulty.
To obtain the functional subscale score, the scores of the specific and usual activities are added and the sum is divided by two. The total score of the PRTEE questionnaire is obtained by adding the scores of the pain and function subscales. The total score ranges from 0 to 100, with a score of 0 indicating no disability and a score of 100 indicating marked disability, where pain and functional problems are equally weighted. The PRTEE questionnaire is a reliable and valid tool for assessing pain and functional limitations associated with tennis elbow [15].
Vitamin D measurement
Blood samples were collected from all participants: a 5-mL venous blood sample was withdrawn under complete aseptic conditions into a plain vacutainer. After clotting, samples were centrifuged at 1500×g for 15 min. The separated serum was placed in aliquots which were stored at – 20 ºC. Hemolyzed samples were discarded. Repeated freezing and thawing was avoided. Serum levels of 25(OH) vitamin D were measured by electrochemiluminescence (REF: 03314847) on Cobas e 411 (Roche Diagnostics GmbH, SandhoferStrasse 116, D-68305 Mannheim). Vitamin D deficiency was defined as a serum level lower than 20 ng/ml and insufficiency as a serum level between 20 and 30 ng/ml and sufficient above 30 ng/ml [16].
Statistical methods
Data collected was revised, coded, tabulated, and imported into a PC using Statistical Package for Social Science version 20 (SPSS-V20) USA. The data were presented and analyzed by the type of data obtained for each parameter. A mean, standard deviation, and range for numerical data, and a frequency and percentage for non-numerical data. Quantitative data were compared using the Student t test. An analysis of nonparametric variables in the same group is conducted using the linear correlation coefficient. In quantitative data, the ANOVA test was used to compare different times within the same group. The results were considered significant at a p value ˂ 0.05, and highly significant at a p value of 0.001.
Results
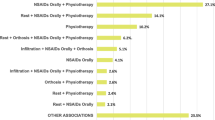
In Table 1, demographic, clinical, and laboratory data are presented along with scoring parameters in patients suffering from lateral epicondylitis Table 2.
The presence of vitamin D deficiency was significantly associated with lateral epicondylitis patients (p 0.001). As a result of vitamin D deficiency, there was a highly significant association between PRTEE score (p 0.001), VAS score (p 0.001), and grip strength (p 0.001).
Discussion
It is a musculoskeletal disorder affecting the epicondyle region of the elbow [17]. Various degenerative and inflammatory conditions affect muscles, tendons, joints, ligaments, peripheral nerves, and blood vessels. There are several types of ligament disorders, tendinopathies, and intra-articular disorders included in this category [8].
It is important to recall that lateral epicondylitis is primarily an inflammatory condition. A more accurate description of the symptoms was provided by the term tendinopathy [18].
Performing repetitive flexion, extension, pronation, and supination movements of the elbow, lifting heavy objects, and frequently extending the wrist against resistance are factors that contribute to the onset of lateral epicondylar tendinopathy [19].
In addition to its biological effects on calcium phosphate chemistry, vitamin D is also a steroid compound. There is evidence that it plays an important role in maintaining calcium homeostasis [20]. Muscle function and immune response are related to its concentrations in both the general population and athletes [21]. The relationship between vitamin D levels and tendinopathy has been studied in a variety of ways. Vitamin D was evaluated in our study to determine whether it plays a role in lateral epicondylitis.
The demographic data in the patient group of Yaka et al. [6] was in line with our demographic data as regards age and sex. In this study, the mean level of vitamin D was 22.569 ± 15.11. There was a deficiency of vitamin D in 50 patients (55.56%), an insufficient level in 10 patients (11.11%), and a sufficient level in 30 patients (33.33%). In this study, patients with lateral epicondylitis had low vitamin D levels, which proved the existence of lateral epicondylitis is significantly associated with vitamin D deficiency. According to Min et al. [10], vitamin D has beneficial effects on tendons in addition to muscles and bones.
Type I collagen is synthesized by tenoblasts, and type I collagen is maintained by tenocytes. The study by Min et al. [10] found that when tenocytes were suppressed and then exposed to vitamin D, the type I collagen gene expression increased. There is also the possibility that mechanical stretching of the tendon may down-regulate type I collagen through the action of tumor necrosis factor-alpha (TNFα) and metalloproteinase 9 (MMP 9). Vitamin D is an important predictor of tendinitis as it plays a crucial role in the production of type I collagen, indicating that vitamin D plays a crucial role in tendinitis development [22]; however, we believe that vitamin D deficiency alone cannot explain the pathogenesis of lateral epicondylitis.
Our study is the first research to determine the effect of low vitamin D levels on the functional ability, strength, and pain scales in patients suffering from lateral epicondylitis (lateral epicondylar tendinopathy). The mean PTREE score in patients with deficient vitamin D was 69.68 ± 6.85, in patients with insufficient vitamin D was 41.2 ± 9.414, and in sufficient with vitamin D was 27.33 ± 5.208. Lateral epicondylitis patients with vitamin D deficiency, the mean VAS score was 7.52 × 1.11, among those with insufficient vitamin D, it was 4.4 × 0.516, and among those with sufficient vitamin D, it was 3.6 × 1.102. Also, the mean of grip strength in patients with deficient vitamin D was 11.44 ± 4.041, in patients with insufficient vitamin D was 21 ± 1.491, and in sufficient with vitamin D was 33.733 ± 8.149. As a result, patients with vitamin D deficiency have significantly worse PRTEE scores, VAS scores, and grip strength, which has been proven by demonstrating a statistically significant relationship between lateral epicondylitis patients with deficient vitamin D and each of the PRTEE scores, VAS scores, and hand grip strength scores. Deficient levels of vitamin D were more significantly correlated with pain and functional scores than insufficient levels or sufficient levels, indicating that deficiency of vitamin D negatively affected pain and functional scores, which negatively affected quality of life and led to significant reductions in daily activities.
Limitations of the study
There were limited samples due to a lack of funding and the patients were not followed up after receiving vitamin D therapy. Factors of lateral epicondylitis and other vitamin D were not evaluated in this study.
Conclusion
A complete understanding of the etiology of lateral epicondylitis is still pending. Our study concluded that patients with lateral epicondylitis had significantly low vitamin D levels, suggesting that low vitamin D levels may contribute to the etiology of lateral epicondylitis among Egyptians, and could be considered a predictive factor for tendinitis. We have further concluded that patients with severe vitamin D deficiency had poorer outcomes in terms of their functional ability and lifestyle activities.
Recommendations
Further studies should include a longer period and a larger sample size to clarify vitamin D’s role in lateral epicondylitis etiology.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- MMP 9:
-
Matrix-metalloproteinase 9
- PRTEE:
-
Patient-Rated Tennis Elbow Evaluation
- TNFα:
-
Tumor necrosis factor
- VAS:
-
Visual analog scale
References
Tosti R, Jennings J, Sewards JM (2013) Lateral epicondylitis of the elbow. Am J Med 126(4):357
Laura LP, Raguel LR (2022) Physiotherapy treatment of lateral epicondylitis: a systematic review. J Back Musculoskelet Rehabil 35(3):463–477
Lenoir H, Mares O, Carlier C (2019) Management of lateral epicondylitis. Orthop Traumatol Surg Res 105(8):S241–S246
Ollivierre CO, Nirschl RP (1996) Tennis elbow: current concepts of treatment and rehabilitation. Sports Med 22:133–139
Haahr JP, Andersen JH (2003) Physical and psychosocial risk factors for lateral epicondylitis: a population-based case-referent study. Occup Environ Med 60:322–329
Yaka H, Basbug V, Tekin AA, Ozer M (2022) Evaluation of the relationship between lateral epicondylitis and Vitamin D. Jt Dis Relat Surg 33(2):414–418
Barati H, Zarezadeh A, MacDermid JC, Sadeghi-Demneh E (2019) The immediate sensorimotor effects of elbow orthoses in patients with lateral elbow tendinopathy: a prospective crossover study. J Shoulder Elbow Surg 28(1):e10–e17
Filippo LD, Vincenzi S, Pennella D, Maselli F (2022) Treatment, diagnostic criteria, and variability of terminology for lateral elbow pain: Findings from an overview of systematic reviews. Healthcare 10(6):1095
Pludowski P, Takacs I, Boyanov M, Belaya Z, Diaconu CC, Mokhort T et al (2022) Clinical practice in preventing, diagnosing, and treating vitamin D deficiency: a central and eastern European expert consensus statement. Nutrients 14(7):1483
Min K, Lee JM, Kim MJ, Jung SY, Kim KS, Lee S et al (2019) Restoration of cellular proliferation and characteristics of human tenocytes by vitamin D. J Orthop Res 37:2241–2248
Horas K, Fraissler L, Maier G, Jakob F, Seefried L, Konrads C et al (2017) High prevalence of vitamin D deficiency in patients with bone marrow edema syndrome of the foot and ankle. Foot Ankle Int 38:760–766
Ryu KJ, Kim BH, Lee Y, Dan J, Kim JH (2015) Low serum vitamins D is not correlated with the severity of a rotator cuff tear or retear after arthroscopic repair. Am J Sports Med 43:1743–1750
Langley GB, Sheppeard H (1985) The visual analogue scale : its use in pain measurement. Rheumatol Int 5(4):145–8
Lin CL, Lee JS, Su WR, Kuo LC, Tai TW, Jou IM (2011) Clinical and ultrasonographic results of ultrasonographically guided percutaneous radiofrequency lesioning in the treatment of recalcitrant lateral epicondylitis. Am J Sports Med 39(11):2429–35
MacDermid J (2007) The Patient Rated Tennis Elbow Evaluation (PTREE) User Manual. School of Rehabilitation Science, McMaster University, Hamilton, Canada
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930
Helliwell PS, Bennett RM, Littlejohn G, Muirden KD, Wigley RD (2003) Towards epidemiological criteria for soft tissue disorders of the arm. Occup Med 53:313–319
Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF (2002) Time to abandon the tendinitis myth. BMJ 324:626–627
Coombes BK, Bisset L, Vicenzino B (2015) Management of lateral elbow tendinopathy: one size does not fit all. J Orthop Sports Phys Ther 45:939–949
Cardwell G, Bornman JF, James AP, Black LJ (2018) A review of mushrooms as a potential source of dietary Vitamin D. Nutrients 10:1498
Wicinski M, Adamkiewicz D, Adamkiewicz M, Sniegocki M, Podhorecka M, Szychta P et al (2019) Impact of vitamin D on physical efficiency and exercise performance: a review. Nutrients 11(11):2826
Chen K, Li P, Zhao H, Yan X, Ma Y (2017) Effects of tumor necrosis factor inhibitor on stress-shielded tendons. Orthopedics 40:49–55
Acknowledgements
Not applicable.
Funding
This study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
SL wrote the paper with revision. NN followed the patients and collected the patients’ data. SG gave ideas, put study design, and revised the manuscript. They all revised the statistics and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee (REC) of the Faculty of Medicine at Ain Shams University in Egypt. Reference number of approval: FMASU R 244/2023. All patients included in this study gave written informed consent to participate in this research.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests. Dr. Salwa Galal is an author and associate editor in the Egyptian Rheumatology and Rehabilitation Journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Leithy, S.A., Adly, N.N. & Galal, S. Role of vitamin D in lateral epicondylitis among Egyptians. Egypt Rheumatol Rehabil 50, 61 (2023). https://doi.org/10.1186/s43166-023-00231-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-023-00231-8