Abstract
Background
The present study aimed to investigate the efficacy of a comprehensive rehabilitation program on quality of life, anxiety, fatigue, and functional status in post-COVID-19 patients admitted to a specialized rehabilitation unit. The secondary objective of the study was to compare the differences between vaccinated and unvaccinated patients.
Results
The single-center prospective study was conducted. Demographics, comorbidities, vaccination, clinical signs and symptoms, and oxygen saturation were assessed. The rehabilitative protocol was created considering the condition of patients, age, the direct impact of COVID-19 on the systems, sequelae, severity of disease, and comorbidities. The comprehensive rehabilitation program through a multidisciplinary team is applied in a stepwise graded manner. The Nottingham Health Profile (NHP), Fatigue Severity Scale (FSS) The Functional Ambulation Categories (FAC), the modified Medical Research Council (mMRC), the Modified Borg Scale, post-COVID-19 Functional Status (PCFS) scale, Hospital Anxiety and Depression Scale (HADS), and the Barthel Index (BI) were used. In total, 39 patients (61.5% men, age 59.7.0 ± 15.6 years) participated in the study. They were discharged home after 37.5 ± 17.6 days stay in the hospital. The most frequently reported persistent symptoms were dyspnea (76.9%), fatigue (69.2%), and myalgia (64.1%). There was a statistically significant improvement in baseline outcomes including BI, HADS, PCFS, FSS, MMRC, Modified Borg Scale, FAC, O2 support, and NHP after the comprehensive rehabilitation program (p < 0.001). The vaccinated patients had older age, high BMI, and shorter duration of rehabilitation (p = 0.003, p = 0.040, p = 0.022, respectively), while unvaccinated patients had higher BI, FSS, PCFS, and FAC.
Conclusion
The comprehensive rehabilitation program improves quality of life, reduces fatigue, anxiety, and depression, and regains function in patients with post-COVID-19 syndrome. In addition, vaccinated patients had older ages and shorter duration of rehabilitation, while unvaccinated patients achieved higher functional status and had significantly higher levels of fatigue at discharge.
Similar content being viewed by others
Background
Corona virus disease 2019 (COVID-19) is a severe respiratory disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 is not only a respiratory tract infection but a multiple-organ syndrome including cardiac, renal, gastrointestinal, nervous, endocrine, and musculoskeletal systems. COVID-19 has resulted in significant morbidity and mortality worldwide due to multiple organ dysfunction or failure. The patients were classified into three 3 groups mild, moderate, and severe. 5.0% of patients need admission to intensive care unit (ICU) [1].
After the first wave of the COVID-19 pandemic, the long-lasting symptoms have also been recognized as post-COVID-19 syndrome after the initial recovery from COVID-19, like many viral diseases. The post-COVID-19 syndrome, also called prolonged COVID-19, describes a pathological process that includes persistent physical, medical, and cognitive sequelae following COVID-19. Although there is no consensus on the definition of post-COVID-19 syndrome, it has been defined by the National Institute for Health and Care Excellence (NICE) as ‘‘signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks (3 months) and are not explained by an alternative diagnosis” [2]. The most commonly reported post-COVID-19 manifestations are a wide range of symptoms including dyspnea, chronic widespread musculoskeletal pain, fatigue, sleep disorders, and psychological issues such as anxiety, depression, and concentration problems. These symptoms have a significant effect on a patient’s quality of life, functional capacity, and participation in social life [3].
The available qualitative evidence showed that the early rehabilitative approach benefits recovery from COVID-19 in patients who require hospitalization and intensive care [4, 5]. The respiratory and neuromotor rehabilitation program is needed to prevent complications and long-term sequelae, provide rapid recovery, and increase the quality of life in patients with post-COVID-19 syndrome after discharge from intensive care or hospital. After the devastating impact of the pandemic, healthcare professionals are now endeavoring to absorb the impact of the patients with COVID-19 infection-related long-term sequelae and disability. So, to alleviate the load on the health care system, Physical and Rehabilitation Medicine professionals play a key role in managing long-term sequelae. However, there is limited attention to the effective management of potential long-term post-COVID-19 syndrome sequelae.
Vaccination is a key role in preventing SARS-CoV-2 infections in public health. The main achievement of the COVID-19 vaccination program is to reduce COVID-19-related hospitalizations, admission to the ICU, and deaths [6, 7]. The safety and efficacy of vaccination is a good issue, although there is no data about the effect on the rehabilitation process.
A rehabilitation team at Ankara City Hospital, Physical Medicine and Rehabilitation Hospital, was targeted to provide the patient-tailored respiratory and neuromotor rehabilitation program in patients with post-COVID-19 syndrome. Therefore, the aim of the present study was to investigate the efficacy of a comprehensive rehabilitation program on quality of life anxiety, fatigue, and functional status in post-COVID-19 patients admitted to a specialized rehabilitation unit. A secondary objective of the study was to compare the differences between vaccinated and unvaccinated patients.
Materials-methods
Patients and study protocol
The single-center prospective study was conducted in Ankara City Hospital, Physical Medicine and Rehabilitation Hospital from January 2022 to May 2022. The study sample consisted of patients with post-COVID syndrome who had not achieved a complete recovery from acute SARS-CoV-2 infection and patients who required hospital admission due to complications related to COVID-19. NICE guideline was used to diagnose post-COVID syndrome [2].
Inclusion criteria were (1) patients aged ≥ 18 years; (2) confirmed SARS-CoV-2 positivity on RT-PCR and ongoing symptoms > 3 months after the diagnosis of COVID-19; (3) able to read or understand the questionnaire. Exclusion criteria were (1) unwillingness to participate in the study, (2) severe cognitive impairment, (3) cardiovascular and hemodynamic instability, and (4) severe exercise intolerance.
Demographics (age, body mass index (BMI), gender, education period), comorbidities, vaccination, clinical signs and symptoms, and oxygen saturation were assessed at admission to the specialized rehabilitation clinic. The study protocol was approved by the Local Research Ethics Committee (Ankara City Hospital, Protocol of the E2-22–1280 of January 2022). The study adhered to the guidelines of the Declaration of Helsinki and written informed consent was obtained from all participants.
Assessments
Health-related quality of life was assessed by the Nottingham Health Profile (NHP). The NHP is a generic questionnaire to measure perceived distress related to illness. The scores of each component are weighted to give a score from 0 (no problems) to 100 (maximum problems). A low NHP score signifies a high quality of life. Turkish adaptation of the NHP has been performed [8].
Fatigue was assessed with the Fatigue Severity Scale (FSS). The FSS is a 9-item questionnaire scored on a 7-point scale with 1 = strongly disagree and 7 = strongly agree designed to measure fatigue severity. Higher scores indicate more severe fatigue [9].
Ambulation status was assessed with The Functional Ambulation Categories (FAC). The FAC is a 6-point functional walking test that evaluates ambulation ability [10].
The modified Medical Research Council (mMRC) scale was used to assess dyspnea in daily living in chronic respiratory diseases. mMRC is a valid five-point (0–4) scale based on the severity of dyspnea [11]. The modified Borg Scale was used to assess the dyspnea level during physical effort [12]. It is a valid scale ranging 0–10.
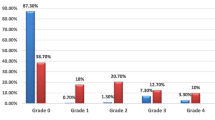
Post-COVID-19 Functional Status (PCFS) scale was developed by Klok to assess functional status to capture the heterogeneity of post-COVID-19 outcomes. The PCFS score ranges between 0 and 5: grade 0 indicates no functional limitation and grade 4 indicates severe functional limitation [13]. Turkish adaptation of the PCFS has been performed [14].
Hospital Anxiety and Depression Scale (HADS) was used to determine the level of anxiety and depression. This scale is a tool for the detection of anxiety and depression in people with physical health problems consisting of a 14-item scale: seven of the items relate to anxiety and seven relate to depression [15].
The Barthel Index (BI) was used to measure performance in activities of daily living (ADL). The score is a 100-point score.
Rehabilitation program
Led by physiatrists, the multidisciplinary team of occupational therapists, social workers, rehabilitation psychologists, speech and language therapists, and dietitians focused on targeted interventions to improve functional independence and deal with secondary complications. The type, dose/duration, timing, and methods of an individualized rehabilitative protocol were created considering the condition of patients, age, the direct impact of COVID-19 on the body systems, sequelae, severity of disease, and comorbidities. The comprehensive rehabilitation program through a multidisciplinary team was applied in a stepwise graded manner.
The neuromuscular rehabilitation program consisted of mobilization, progressive muscle strengthening, balance and coordination exercises. The program was applied to all patients one hour a day, 5 days a week, totaling 30 sessions. An early mobilization program including posture changes, bed mobility, sitting out of bed, sitting balance, sit-to-stand, tilt table, and walking was performed. Passive, active-assisted, or resisted exercises were performed to improve the range of motion and muscle strength. Muscle strengthening exercises of upper and lower limbs, trunk, and gluteus muscles, abdominal muscles were performed. Functional electrical stimulation (FES) cycling was used to assist with strengthening the upper and lower extremities. FES cycling with an 8-channel stimulator applied on both sides of the quadriceps, hamstring, tibialis anterior, and gastrocnemius muscles between 20 and 40 revolutions per minute (rpm). All sessions were 30 min. The pulse width was 200–300 μs, the intensity was 100 mA, and the frequency was ranging from 30 to 45 Hz. FES cycling was performed on patients who have muscle weakness twice a week, totaling 10 sessions.
The exercise capacity was assessed with cardiopulmonary exercise testing. Cardiopulmonary rehabilitation program consisting of aerobic exercise, muscle strengthening, and breathing exercises was determined according to the guidelines [16, 17]. Aerobic exercise was performed on a cyclo-ergometer lasting 30 min for 3–5 days at least 4 weeks. The breathing exercise program consisted of inspiratory muscle training, thoracic expansion, mobilization of respiratory muscles, airway clearance techniques, and controlled breathing techniques such as diaphragmatic, alternate, and pursed-lip breathing. In addition to the breathing exercises, high-frequency chest wall oscillation devices (HFCWO) were applied for secretion mobilization. HFCWO was applied by a respiratory physiotherapist at 10–15 Hz oscillating frequency, based on the patient’s tolerance. The session was performed lasting 20 min and twice a day during 2 weeks.
The blood pressure, heart rate, and oxygen saturation were monitored during each exercise session. The rehabilitation program was stopped in case of tachypnea (> 30 breaths/min), worsening dyspnea, decreasing (≥ 4%) of peripheral SpO2 and SpO2 of < 90%, bradycardia, tachycardia, and variable arrhythmias.
Speech and language therapists evaluated and managed dysphagia and voice impairments. Rehabilitation psychologists support patients with depression, anxiety, or post-traumatic stress disorder. Occupational therapists promoted activities of daily living to fulfill their daily routines and prepare patients for discharge. To detect potential nutrient deficiencies, patients were evaluated individually by a dietitian.
Statistical analyses
SPSS 22.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Shapiro–Wilk tests were used to determine the normal distribution. In descriptive analyses, means and standard deviations were used for normally distributed variables, medians and interquartile range (IQR) for non-normally distributed and ordinal variables, and number and percentage for nominal variables. Patients were divided into two groups based on their vaccination status. To compare the two groups, the Student t test was performed for normally distributed data, and the Mann–Whitney U test was used for ordinal and non-normally distributed data. A paired t-test was used to compare parametric variables within groups, while the Wilcoxon test was used to compare non-parametric variables. Delta analyses were also performed using the Student t test or Mann–Whitney U test to assess the differences between the groups (from baseline to discharge). The statistical significance level was set at p ≤ 0.05.
Results
In total, 39 patients (61.5% men, age 59.7.0 ± 15.6 years, BMI 24.4 ± 3.9 kg/m2) participated in the study. They were discharged home after 37.5 ± 17.6 days stay in the rehabilitation hospital. The most frequently reported persistent symptoms were dyspnea (76.9%), fatigue (69.2%), and myalgia (64.1%). Pulmonary involvement was diagnosed in 74.4%, cerebrovascular disease in 17.9%, and CIP/CIM in 17.9% of the patients. The most comorbidities were HT (46.3%), DM (25.7%), and cardiovascular disease (25.7%). About 38% of the patients needed oxygen support when they were discharged home. All demographic and clinical characteristics of the patients are presented in Table 1.
There was a statistically significant improvement in baseline outcomes including BI, HADS, PCFS, FSS, MMRC, FAC, Modified Borg Scale, O2 support, and NHP after the comprehensive rehabilitative program (p < 0.001) (Table 2). Table 3 presents the difference in outcome measures between vaccinated and unvaccinated patients with post-COVID-19. The vaccinated patients had older age, high BMI, and shorter duration of rehabilitation compared with unvaccinated patients (p = 0.003, p = 0.040, p = 0.022, respectively). At discharge, unvaccinated patients had higher BI, FSS, PCFS, and FAC. There was no significant improvement in quality of life between vaccinated and unvaccinated patients after discharge (Table 4). The relationship between the length of stay in a rehabilitation center and changes in function and quality of life was examined, NHP-pain (r = 0.326, p = 0.043) and NHP-sleep (r = 0.336, p = 0.036) were shown to be correlated with the length of stay (Table 5).
Discussion
It is clear that the rehabilitation program is recommended for the patients discharged from hospital and intensive care to reduce the complications related to COVID-19 syndrome [18, 19]. The results of our study showed that the comprehensive rehabilitation program improves quality of life, reduces fatigue, anxiety, and depression, and regains function in patients with post-COVID-19 syndrome. In our study, dyspnea was the most common post-COVID-19 symptom, followed by fatigue and myalgia. In addition, vaccinated patients had older ages and shorter duration of rehabilitation, while unvaccinated patients achieved higher functional status and had significantly higher levels of fatigue at discharge.
We showed that dyspnea, fatigue, and myalgia are the most common post-COVID-19 symptoms. This is consistent with data from previous studies. Romero-Duarte et al. [20] revealed that dyspnea and fatigue are the most frequent persistent symptoms after COVID-19 in their cohort report. In addition, Huang et al. [21] found that fatigue, muscle weakness, and sleep difficulties were common persistent symptoms at 6 months after symptom onset. They also revealed that the patients had remarkably pulmonary diffusion abnormality and abnormal CT findings 6 months after symptom onset. They also showed that these findings correlate with the disease severity. So, rehabilitation teams undertaking the treatment of post-COVID-19 patients may obtain clues about the severity of the disease when faced with symptoms such as dyspnea, fatigue, and myalgia.
Although the most common clinical presentation of COVID-19 is a respiratory disease, neurologic manifestations have been reported and recognized increasingly. In our study, 25.6% of the 39 patients had various neurological complications such as cerebrovascular disease, CIP/CIM, transverse myelitis, GBS, and anoxic brain injury. Mao et al. [22] reported that 36.4% had neurological manifestations involving the central nervous system, peripheral nervous system, and skeletal muscles. Romero-Sánchez et al. [23] showed that 57.4% of 841 patients hospitalized with COVID-19 developed some form of neurologic symptoms.
The older than 60 years, concomitant comorbidities, and smoking history are major factors that contribute to mortality associated with COVID-19 and the need for ICU care. In our sample, the most comorbid conditions are HT, DM, and cardiovascular disease. Similarly, the review, which analyzed 1458 patients, showed that the leading comorbid conditions are hypertension, cardiovascular and cerebrovascular disease, and diabetes in COVID-19 patients [24]. The estimation of prognosis can be considered concomitant comorbidities.
Exercise is a well-documented issue with profound therapeutic effects on health that prevent many diseases such as metabolic, pulmonary, cardiovascular, and musculoskeletal diseases. It can support physical health as well as mental health. Furthermore, it is clearly shown to improve quality of life, reduce psychological stress, and improve physical function [25]. Our results showed that a combined neuromuscular and cardiopulmonary exercise program could improve quality of life and decrease anxiety and depression levels in patients with post-COVID-19 syndrome. These results are in line with a randomized controlled study, which was conducted by Liu [26]. It was shown that improving respiratory functions in elderly patients with COVID-19 plays a key role in maintaining high QoL after a 6-week respiratory rehabilitation program. Individualized and appropriate exercise programs could help provide high QoL in patients with post-COVID-19 syndrome.
The studies have focused their investigations on clinical characteristics and treatment options of COVID-19 during the first time of the pandemic; however, Taboada et al. [27] evaluated the functional status and the presence of persistent symptoms after hospitalization. They revealed that most hospitalized patients with COVID-19 have low functional status at 6 months after hospitalization. In our study, functional status was assessed using the PCFS and there was an improvement in functional status after a comprehensive rehabilitation program. The physical exercise program may be a potent treatment option that improves physical performance and functionality in patients with post-COVID-19 syndrome.
In our sample analyses, the present study highlights that vaccinated patients had older age and shorter duration of rehabilitation in comparison with unvaccinated patients. In addition, while unvaccinated patients achieved higher functional status, they had significantly higher levels of fatigue at discharge. In line with our study, Chiumello et al. revealed that vaccinated patients were older and with more comorbidities [28]. Similarly, it was shown that fully vaccinated patients with COVID-19 in Norway had a shorter length of stay in hospital [6]. The results supported that vaccination may prevent persistent long-term sequela and decrease the duration of rehabilitation.
Patients treated in the ICU experience severe muscle weakness and atrophy. Muscle atrophy in the ICU is associated with sarcopenia, increased burden of care, poor prognoses such as prolonged hospital stay, low quality of life, poor rehabilitation outcomes, and mortality [29,30,31]. About 84% of our sample consisted of patients admitted to an ICU. So, the most common complications were muscle weakness-atrophy and pressure ulcers in our study. It was noticed that combined exercise training with protein supplements improves muscle strength, physical performance, and quality of life in patients with muscle atrophy, older COVID-19, and frail patients [32,33,34]. In line with the literature, early mobilization and nutritional interventions including protein supplements were used to prevent intensive care complications in our study. All patients were evaluated by a dietitian in terms of calorie and protein support.
The results indicated that the pain and sleep categories of NHP are correlated with the length of stay in the hospital. While up to 50% of the general population may experience chronic pain, 63.3% of patients with post-COVID-19 syndrome reported experiencing chronic pain. It was shown that chronic pain is related to psychological stress and the results of admission to the hospital or ICU [35]. In line with our study, Demirel et al. showed that a high VAS score is an indicator of longer hospital stays [36]. So, the pain and sleep disorder may be used as an indicator to estimate the prognosis.
This study provides a model for comprehensive rehabilitation to manage the post-COVID-19 symptoms. However, the present study has some limitations. First, the study did not include a control group. So, the effectiveness of comprehensive rehabilitation could be better evaluated with case–control studies in the future. Second, the study sample size is small. Therefore, the results may not be sufficient to reflect all post-COVID-19 populations. To demonstrate the effect of rehabilitation on post-COVID-19 syndrome, a larger sample size with control group studies is needed in the future.
Conclusion
The long-term management of post-COVID-19 syndrome is still a challenge, which affects multiple organ systems, with significant impacts on morbidity, quality of life, and mortality. The diversity of sequelae may be associated with the disease and a prolonged stay in the ICU. A comprehensive rehabilitation program may support accelerating the return to normal life, reducing sequelae, increasing the quality of life and functionality, and removing obstacles in recovering from COVID-19. This study may be a guide for rehabilitation clinicians in other pandemics or viral infection outbreaks (Supplementary Data).
Availability of data and materials
The corresponding author will provide the datasets used and analyzed during the current work upon reasonable request.
Abbreviations
- ADL:
-
Activities of daily living
- BI:
-
The Barthel Index
- BMI:
-
Body mass index
- CIP/CIM:
-
Critical illness myopathy and/or critical illness neuropathy
- COVID-19:
-
Corona virus disease 2019
- CT:
-
Computerized tomography
- DM:
-
Diabetes mellitus
- FAC:
-
The Functional Ambulation Categories
- FSS:
-
Fatigue Severity Scale
- GBS:
-
Guillain-Barre syndrome
- HADS:
-
Hospital Anxiety and Depression Scale
- HFCWO :
-
High-frequency chest wall oscillation
- HT:
-
Hypertension
- ICU:
-
Intensive care unit
- mMRC:
-
Medical Research Council
- NICE :
-
The National Institute for Health and Care Excellence
- NHP:
-
The Nottingham Health Profile
- PCFS:
-
Post-COVID-19 Functional Status
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
References
Gamal DM, Ibrahim RA, Samaan SF (2022) Post COVID-19 syndrome in a prospective cohort study of Egyptian patients. Egypt Rheumatol Rehabil 49(1):12
Venkatesan P (2021) NICE guideline on long COVID. Lancet Respir Med 9(2):129
Ramakrishnan RK, Kashour T, Hamid Q, Halwani R, Tleyjeh IM (2021) Unraveling the mystery surrounding post-acute sequelae of COVID-19. Front Immunol 12:686029
Andrenelli E, Negrini F, de Sire A, Arienti C, Patrini M, Negrini S et al (2020) International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action. Systematic rapid living review on rehabilitation needs due to COVID-19: update to May 31st. Eur J Phys Rehabil Med 56(4):508–514
Curci C, Pisano F, Bonacci E, Camozzi DM, Ceravolo C, Bergonzi R et al (2020) Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur J Phys Rehabil Med 56(5):633–641
Whittaker R, Bråthen Kristofferson A, Valcarcel Salamanca B, Seppälä E, Golestani K, Kvåle R et al (2022) Length of hospital stay and risk of intensive care admission and in-hospital death among COVID-19 patients in Norway: a register-based cohort study comparing patients fully vaccinated with an mRNA vaccine to unvaccinated patients. Clin Microbiol Infect 28(6):871–878
Estella Á, Cantón ML, Muñoz L, Higueras IR, Recuerda Núñez M, TejeroAranguren J et al (2021) On behalf of the group of infectious diseases of the Andalusian Society of intensive care and coronary units Samiuc. Vaccinated patients admitted in ICU with severe pneumonia due to SARS-CoV-2: a multicenter pilot study. J Pers Med 25(11):1086
Kücükdeveci AA, McKenna SP, Kutlay S, Gürsel Y, Whalley D, Arasil T (2000) The development and psychometric assessment of the Turkish version of the Nottingham Health Profile. Int J Rehabil Res 23(1):31–38
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46(10):1121–1123
Collen FM, Wade DT, Bradshaw CM (1990) Mobility after stroke: reliability of measures of impairment and disability. Int Disabil Stud 12(1):6–9
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA (1999) Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 54(7):581–586
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–381
Klok FA, Boon GJAM, Barco S, Endres M, Geelhoedet JJM et al (2020) The post-COVID-19 functional status scale: a tool to measure functional status over time after COVID-19. Eur Respir J 56(1):2001494
ÇalıkKütükcü E, Çakmak A, Kınacı E, Uyaroğlu OA, Yağlı NV, SainGüven G et al (2021) Reliability and validity of the Turkish version of post-COVID-19 functional status scale. Turk J Med Sci 51(5):2304–2310
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Besnier F, Bérubé B, Malo J, Gagnon C, Grégoire CA, Juneau M et al (2022) Cardiopulmonary rehabilitation in long-COVID-19 patients with persistent breathlessness and fatigue: the COVID-Rehab Study. Int J Environ Res Public Health 19(7):4133
KurtaişAytür Y, Köseoğlu BF, ÖzyemişçiTaşkıran Ö, Ordu-Gökkaya NK, ÜnsalDelialioğlu S, Sonel Tur B et al (2020) Pulmonary rehabilitation principles in SARS-COV-2 infection (COVID-19): a guideline for the acute and subacute rehabilitation. Turk J Phys Med Rehab 66(2):104–120
Korupolu R, Francisco GE, Levin H, Needham DM (2020) Rehabilitation of critically ill COVID-19 survivors. J Int Soc Phys Rehabil Med 3(2):45–52
Major ME, Kwakman R, Kho ME, Connolly B, McWilliams D, Denehy L, Hanekom S et al (2016) Surviving critical illness: what is next? An expert consensus statement on physical rehabilitation after hospital discharge. Crit Care 20:1–10
Romero-Duarte Á, Rivera-Izquierdo M, Guerrero-Fernández de Alba I, Pérez-Contreras M, Fernández-Martínez NF, Ruiz-Montero RI et al (2021) Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med 19(1):129
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X et al (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397(10270):220–232
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q et al (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan China. JAMA Neurol 77(6):683–690
Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, Sánchez-Larsen Á, Layos-Romero A, García-García J et al (2020) Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology 95(8):e1060–e1070
Kakodkar P, Kaka N, Baig MN (2020) A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus 12(4):e7560
Chen Z, Lan W, Yang G, Li Y, Ji X, Chen L et al (2020) Exercise ıntervention in treatment of neuropsychological diseases: a review. Front Psychol 11:569206
Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y (2020) Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract 39:101166
Taboada M, Cariñena A, Moreno E, Rodríguez N, Domínguez MJ, Casal A et al (2021) Post-COVID-19 functional status six-months after hospitalization. J Infect 82(4):e31–e33
Chiumello D, Tavelli A, Serio L, De Benedittis S, Pozzi T, Maj R et al (2023) Differences in clinical characteristics and quantitative lung CT features between vaccinated and not vaccinated hospitalized COVID-19 patients in Italy. Ann Intensive Care 13(1):24
Nonoyama T, Shigemi H, Kubota M, Matsumine A, Shigemi K, Ishizuka T (2022) Neuromuscular electrical stimulation in the intensive care unit prevents muscle atrophy in critically ill older patients: a retrospective cohort study. Medicine (Baltimore) 101(31):e29451
Wang Y, Tan S, Yan Q, Gao Y (2023) Sarcopenia and COVID-19 Outcomes. Clin Interv Aging 18:359–373
Heesakkers H, van der Hoeven JG, Corsten S, Janssen I, Ewalds E, Simons KS et al (2022) Clinical outcomes among patients with 1-year survival following ıntensive care unit treatment for COVID-19. JAMA 327(6):559–565
Nambi G, Abdelbasset WK, Alrawaili SM, Elsayed SH, Verma A, Vellaiyan A et al (2022) Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia: a randomized controlled trial. Clin Rehabil 36(1):59–68
Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, Chen LK et al (2014) Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 43(6):748–759
Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A et al (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 33(6):929–936
Zis P, Ioannou C, Artemiadis A, Christodoulou K, Kalampokini S, Hadjigeorgiou GM (2022) Prevalence and determinants of chronic pain post-COVID; crosssectional study. J Clin Med 11:5569
Demirel E, Şahin A, Utlu M, Çepni Ş, Veizi E, YavuzVeizi BG (2021) A relationship between musculoskeletal pain and prognosis in hospitalized COVID-19 patients. J Health Sci Med / JHSM 4(3):300–305
Acknowledgements
Not applicable.
Funding
This research did not receive any specific funding from the public or commercial.
Author information
Authors and Affiliations
Contributions
Bilge Kesikburun and Ayşe Merve Ata were involved in conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, writing—original draft, writing—review, and editing. Pınar Borman and Ebru Alemdaroğlu were involved in visualization and supervision. Elif Esen Özdemir, Pınar Borman, and Ebru Alemdaroğlu were involved in validation, review, and editing. Elif Becenen and Nurdan Metin have accessed and verified the data. Bilge Kesikburun and Ayşe Merve Ata were responsible for the decision to submit the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants in this were given the opportunity to provide written consent and the protocol was approved by the ethical committee of Ankara City Hospital no E2-22–1280.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kesikburun, B., Ata, A.M., Borman, P. et al. The effect of comprehensive rehabilitation on post-COVID-19 syndrome. Egypt Rheumatol Rehabil 50, 60 (2023). https://doi.org/10.1186/s43166-023-00227-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-023-00227-4