Abstract
Background
Splinting is frequently used in the treatment of CTS (carpal tunnel syndrome) and is mostly preferred at night. On the other hand, there are some studies suggesting the use of splint throughout the day. However, there is still no consensus. The aim of this randomized controlled study was to evaluate the effects of day and night splinting in terms of pain, symptom severity, functional status, and quality of life in patients with CTS.
Results
Seventy wrists of 46 patients with CTS were evaluated. In the day-night splint group, according to without splint group and night-only splint group, a statistically significant improvement was found in terms of pain level assessed by Visual Analogue Scale (p = 0.001, p = 0.015, respectively), Boston Carpal Tunnel Questionnaire-Functional Severity Scale (p = 0.004, p = 0.020, respectively), The Nottingham Health Profile-pain (p = 0.001, p = 0.003, respectively), The Nottingham Health Profile-social isolation (p = 0.001, p = 0.001, respectively), and The Nottingham Health Profile-total score (p = 0.001, p = 0.012, respectively). In addition, it was found that even the use of splint only at night resulted in a significant reduction in pain compared to the control group (p = 0.018).
Conclusions
Continuation of splinting as much as possible during the daytime in addition to night splinting is beneficial in terms of pain, nocturnal symptoms, functionality, and quality of life.
Similar content being viewed by others
Background
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy that can cause pain, numbness, and loss of strength in the hand. The prevalence of CTS is 1–5% of the general population and is more common in women [1]. Clinical evaluation, electrophysiological examination, and ultrasonography can be used in diagnosis [2].
The main goal in the treatment of CTS is to reduce symptoms and increase hand functionality. Its treatment options are splinting, nonsteroidal anti-inflammatory drugs, steroid injection, and surgery [3].
Currently, the most commonly used treatment method other than surgery is to splint the wrist in a neutral position. Repetitive wrist movements and forearm pronation/supination may increase carpal tunnel pressure, and in some cases, the symptoms of CTS [4]. The main goal of splinting is to prevent conditions that increase carpal tunnel pressure [5].
Splinting, which is used in the treatment of CTS, is mostly preferred at night because it does not interfere with daily life and workplace activities. Moreover, using a splint throughout the day may prevent patients from participating in social activities [6]. On the other hand, there are some studies suggesting the use of splint throughout the day [7,8,9]. However, there is still no consensus. In addition, the uncertainty of the optimal treatment duration of splinting in the treatment of CTS has also been the subject of various studies [10, 11]. A review examining the use of splint in CTS patients revealed that the use of splint varied from 2 weeks to a year, with the most common duration being 2–4 weeks [11].
According to our knowledge, there is no randomized controlled study in which the effects of night-only splinting or day-night splinting on pain, functionality, and quality of life in CTS were evaluated together. Therefore, the aim of this study is to investigate the effects of night-only and day-night splinting in patients diagnosed with CTS in terms of patients’ pain, symptom severity, functional status, and quality of life.
Methods
This prospective, randomized controlled trial evaluated patients treated for CTS with no splint, night-only splint, and day-night splint. The study protocol was approved by Health Sciences University Diskapi Yildirim Beyazit Education and Research Hospital Local Ethics Committee (date: 07.02.2022, number: 130/07), and the study was carried out in the same hospital. Informed consent was obtained from all patients at the beginning of the study and it was carried out between February 2022 and July 2022.
Inclusion criteria included the following: (1) to be over 18 years old, (2) patients diagnosed with mild or moderate CTS in electrophysiological examination according to the protocol described by Bland JD [12], (3) the presence of symptoms for more than a month.
Study exclusion criteria included the following: (1) having severe CTS on electrophysiological examination; (2) excluding CTS-related splinting in the past 6 months or have received any treatment (such as injection, physical therapy); (3) having a history of surgery for CTS; (4) endocrine and metabolic diseases (such as diabetes mellitus, hypo-hyperthyroidism, acromegaly), inflammatory rheumatic diseases, alcoholism, history of trauma, or fracture in the affected extremity; (5) presence of accompanying pathology such as thoracic outlet syndrome and cervical radiculopathy; (6) presence of progressive and non-progressive central or peripheral nervous system diseases; (7) history of malignancy; and (8) pregnancy.
Only the affected hands of the patients were included in the study. If a person had bilateral CTS, both hands were included in the study and assessments were made for both hands separately.
The sample size was calculated with G Power version 3.1.8. (University of Dusseldorf, Germany). The smallest sample size required for the 2-point reduction in VAS, which provides the minimal clinically important difference, was found as 18 participants for each group (a power of 80% at a significance level of 5% and an effect size d = 0.4). However, considering the dropouts, 30 patients were targeted in the study for each group. This sample size was similar to the literature [13,14,15,16].
A physician (Z.K.U.), who was blinded to the treatment allocations, evaluated all measurements (baseline and after 12 weeks). All in-group and intergroup evaluations were made by the same doctor. Demographic characteristics of the participants, features and clinical findings related to CTS (symptom duration, the most prominent symptom, presence and duration of nocturnal symptoms, the Tinnel’s and Phalen’s tests, and electrophysiological severity of CTS), and Visual Analogue Scale (VAS, 0–100) for pain levels were recorded.
The Phalen test was performed with the wrists fully flexed and the backs of the hands touching each other for one minute. The test was recorded as positive if the patient reported paresthesia in the sensory distribution of the median nerve while in this position [17]. The Tinnel test is temporary paresthesia in the sensory region of the median nerve when the patient’s arms are supinated and tapped lightly on the carpal tunnel with a hammer [17]. The positivity of these two tests is associated with CTS [16, 17].
All patients filled in the Boston Carpal Tunnel Questionnaire (BCTQ). The BCTQ is a scoring system developed in 1993 for the clinical standardization of CTS patients. It includes 19 questions and consists of sub-scores of functional severity scale (BCTQ-FSS) and symptom severity scale (BCTQ-SSS). An increase in the score indicates that patients are more affected by CTS [18].
The Nottingham Health Profile (NHP) is a general measure of quality of life that measures the level of health problems a person perceives and the impact of these problems on activities of normal daily living. The questionnaire consists of 38 items and assesses six dimensions related to the status of pain, energy, sleep, emotional reactions (ER), physical activity (PA), and social isolation (SI). Between 0 and 100 for each section scoring is done. 0 best, 100 worst indicates health status. Within the scope of the study, the NHP sub-scores and total NHP score were evaluated [19]. In our study, we evaluated quality of life with NHP.
From the electroneuromyography (ENMG) results of the patients, median sensory conduction velocity (SCV), sensory nerve action potential (SNAP), median nerve compound muscle action potential (CMAP), motor conduction velocity (MCV), and distal motor latency (DML) were noted. The velocity correlates directly with the sensory latency and therefore sensory distal latency was not recorded [20].
Patients were randomly assigned to the without splint group (control group, group 1), night-only splint group (group 2), and day-night splint group (group 3). In addition to use while sleeping, splint use for at least half of the waking times was considered “full-time use” [9]. Randomization was conducted by a clinical secretary who was not involved in the study by using opaque envelope method.
Appropriate treatments were given to the groups by another physician (E.U.) who was blinded to the initial assessments. Modification of daily living activities and 3 × 10 repetitions/day tendon-nerve gliding exercises were recommended to all patients. Splinting groups were recommended to use a neutral soft wrist splint during the night (Fig. 1), and group 3 was recommended to continue using the splint during the day as much as possible in addition to the night. The duration of treatment was determined as 12 weeks. Then, the patients were called for re-evaluation after 12 weeks.
In the second evaluation, the splint usage status of the patients and the average daily splint usage time were noted by E.U. The patients’ current VAS, BCTQ, and NHP questionnaires were also noted by the blinded investigator (Z.K.U.). All participants then underwent a second electrophysiological evaluation by another investigator who was blinded to all initial evaluations and treatments administered (E.U.A.). Second SNAP, SCV, CMAP, MCV, and DML were noted.
Pain, functionality, quality of life, and changes in electrophysiological examinations were evaluated in each group. In addition, the changes in the pre- and post-treatment parameters between the three groups were compared, and it was revealed whether the use of splint and its use during the daytime created a significant difference in the success of the treatment.
Statistical analysis
Statistical Package for the Social Sciences (SPSS 25.0 for Windows) was used to analyze the data. Whether the continuous variables showed normal distribution or not was evaluated with the Kolmogorov–Smirnov test. In descriptive statistics, the data were presented as mean (standard deviation [SD]) or median (interquartile range 25% and 75%) for continuous variables, and as frequencies and percentages (%) for nominal and categorical variables. Statistically significant difference among the groups was investigated using the Kruskal–Wallis, Mann–Whitney U, and ANOVA test. χ2 and Fisher’s exact tests were used to analyze the significance of the difference for nominal variables. In addition, the Wilcoxon signed rank test was used for repetitive measurement within the group. Values of p < 0.05 were considered statistically significant.
Results
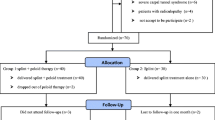
Ninety wrists (30 wrists for each group) of 58 patients were included in the study. Since 12 patients (20 wrists) did not come to the follow-up evaluation, the study was completed with 46 patients (70 wrists). They were divided into 3 groups: without splint group (control group, group 1 = 20 wrists of 14 patients), night-only splint group (group 2 = 28 wrists of 18 patients), and day-night splint group (group 3 = 22 wrists of 14 patients) (Fig. 2).
The mean age of the study group of 46 patients was 47.58 (SD 10.10) years, 40 (87%) of the patients were female and 6 (13%) were male. The patients in the groups were similar to each other in terms of demographic characteristics (p > 0.05) (Table 1).
The distribution and comparison of the disease characteristics of the groups according to the affected wrists are shown in Table 2. The duration of symptoms before treatment, the most prominent symptom, the presence and duration of symptoms at night, Tinnel and Phalen test positivity, and the severity of CTS defined in EMG were similar between the groups. While in group 2, the mediation hours of splint use was 7.0 (4.0–8.0) per day; in group 3, it was 10.0 (7.0–15.0) hours per day. In the comparison between groups before treatment, in group 3, according to groups 1 and 2, BCTQ-SSS (p = 0.037, p = 0.007, respectively), NHP-pain (p = 0.004, p = 0.010, respectively), NHP-ER (p = 0.008, p = 0.023, respectively), and NHP-sleep (p = 0.025, p = 0.004, respectively) scores were worse. There was no difference between the groups in terms of post-treatment evaluation parameters (p > 0.05).
In the comparison of pre- and post-treatment measurements within the groups (Table 3), while no significant change was detected in any parameter in group 1, significant improvement was found in VAS and electrophysiological parameters such as SNAP, SCV, and CMAP in group 2, as well as in BCTQ-SSS, BCTQ-FSS scales, and all quality of life parameters except NHP-energy and NHP-SI detected (p < 0.05). In the 3rd group, the improvement was found in VAS, BCTQ-SSS, BCTQ-FSS, and all quality of life parameters except NHP-energy and this improvement was statistically significant (p < 0.05). Additionally, the decrease in the number of wrists with nocturnal symptoms was significant in groups 2 and 3 (p = 0.006, p = 0.005, respectively).
A comparison of the change in outcome measures between groups is presented in Table 4. In the day-night splint group, according to both without splint and only-night splint groups’ decrease in pain (p = 0.001, p = 0.015, respectively), functional status (p = 0.004, p = 0.020, respectively), pain from quality of life scales (p = 0.001, p = 0.003, respectively), social isolation (p = 0.001, p = 0.001, respectively), and total scores (p = 0.001, p = 0.012, respectively), the improvement was found to be significantly higher. In addition, in terms of pain evaluated by VAS; it was found that even using night-only splint provided a significant reduction in pain compared to without splint (p = 0.018).
Discussion
In this study, while no statistically significant improvement was observed in the without splint group, significant improvements were observed in nocturnal symptoms, pain level evaluated by VAS, symptom severity and functionality, and quality of life in both splint groups. In addition, the improvement observed in the electrophysiological findings in the night-only splint group was also significant. Looking at the comparison of changes in outcome measures between groups, it was found that even using night-only splint resulted in a significant reduction in VAS compared to without splint. In addition, the change in functionality and quality of life in the day-night splint group with treatment was statistically significant compared to the other two groups.
Similar to the literature, in our study, the use of splints, whether used only at night or all day, had a positive effect on the level of pain assessed by VAS [21]. Although the pre-treatment NHP-pain was worse in the day-night splint group than the other 2 groups, when the change in the outcome measures between groups was examined, a statistically significant change was observed in the day-night group compared to the other 2 groups and this shows that the use of the splint during the day may also be important in pain and related quality of life in CTS.
When researched, only one article was found comparing the effects of day-night splinting and night-only splinting in CTS [9]. In this study, the amount of decrease in symptom severity was higher in the day-night splint group than in the night-only splint group, while the functional status improved more in the night-only splint group. These findings are quite different from our study, in which the change in BCTQ-FSS was found to be statistically significantly better in the day-night splinting group. The differences in the design of the studies and the number of patients may have been effective in the different results.
While BCTQ-SSS was worse in the day-night splint group in the pre-treatment evaluation, it showed improvement in repeated measures in both night-only and day-night splint groups, but the change was not statistically significant. This result is similar to the result of the previously mentioned study comparing the use of night-only and day-night splinting. Walker et al. suggested the use of splints in groups for 6 weeks, unlike our study [9]. On the other hand, in the study by Gatheridge et al., it was emphasized that the use of splint for an additional 6 weeks after an initial period of 6 weeks did not have a significant effect on electrophysiological findings, symptom severity, and functionality [10].
In studies on splinting in CTS, it is seen that only DML and sensory distal latency (DSL) are examined among electrophysiological findings [6, 9]. In our study, however, DSL was not recorded; SNAP, CMAP, SCV, and MCV were noted in addition to DML. While significant improvements were achieved in these parameters before and after treatment in the night-only group, no statistically significant difference was observed in all 3 groups when the post-treatment changes were compared. The differences in the number of patients in the studies, the differences in the clinical, electrophysiological and demographic characteristics of the patients before splinting, and the short follow-up period may be the reasons for the lack of significant difference between the groups at follow-up.
Quality of life in CTS is often the focus when reviewing surgical outcomes [22]. In this study, while there was no significant change in the control group, significant improvements were obtained in the various subscores of NHP and total scores in both splint groups. In addition, when these changes were compared between the groups, they were statistically significant in the NHP-pain, NHP-SI, and NHP-total scores in the day-night splint group.
After all these literature comparisons, although the use of splint is more effective in day-night use, night use is an important factor. The reason for this result may be during night sleep, our control over the body is lost. Incorrect positioning of the wrist causes increased pressure in the carpal tunnel and prolonged pressure on the median nerve. Studies have reported that incorrect positioning during sleep exacerbates CTS symptoms acutely, resulting in nighttime symptoms [23, 24]. For this reason, keeping the pressure in the carpal tunnel under control during the night with a correct positioning (splint), we think that it will reduce nighttime symptoms, which will increase the person’s daytime functionality and quality of life as well as good sleep quality.
Limitations of the study
Although it is one of the rare studies comparing night-only and day-night splinting from various aspects, our study also has some limitations. The first is the small number of our patients and the second is the lack of long-term follow-up results. It is not known whether the gains achieved will continue in the long term. Another limitation is that the use of splint cannot be monitored, so it is not objective. The durations of use were noted in line with the information given by the patients.
Conclusion
In conclusion, night splints are beneficial in mild to moderate CTS patients. Extended usage during daytime significantly improved pain, nocturnal symptoms, functionality, and quality of life of patients. Day and night splints could be recommended in CTS patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Abbreviations
- BCTQ:
-
Boston Carpal Tunnel Questionnaire
- CMAP:
-
Compound Muscle Action Potential
- CTS:
-
Carpal tunnel syndrome
- DML:
-
Distal motor latency
- ENMG:
-
Electroneuromyography
- ER:
-
Emotional reactions
- FSS:
-
Functional Severity Scale
- MCV:
-
Motor conduction velocity
- NHP:
-
The Nottingham Health Profile
- PA:
-
Physical activity
- SCV:
-
Sensory conduction velocity
- SI:
-
Social isolation
- SNAP:
-
Sensory nerve action potential
- SSS:
-
Symptom Severity Scale
- VAS:
-
Visual Analogue Scale
References
Roquelaure Y, Ha C, Pelier-Cady MC, Nicolas G, Descatha A, Leclerc A et al (2008) Work increases the incidence of carpal tunnel syndrome in the general population. Muscle Nerve 37:477–482. https://doi.org/10.1002/mus.20952
Kokubo R, Kim K (2021) Carpal tunnel syndrome: diagnosis and treatment. No Shinkei Geka 49(6):1306–1316. https://doi.org/10.11477/mf.1436204516
Pourmokhtari M, Mazrooyi M, Vosoughi AR (2021) Conservative or surgical treatment of carpal tunnel syndrome based on the severity and patient risk factors. Musculoskelet Surg 105(3):315–319. https://doi.org/10.1007/s12306-020-00663-x
Rempel D, Bach JM, Gordon L, So Y (1998) Effects of forearm pronation/supination on carpal tunnel pressure. J Hand Surg [Am] 23:38–42. https://doi.org/10.1016/S0363-5023(98)80086-5
Weiss ND, Gordon L, Bloom T, So Y, Rempel DM (1995) Position of the wrist associated with the lowest carpal-tunnel pressure: implications for splint design. J Bone Joint Surg Am 77:1695–1699. https://doi.org/10.2106/00004623-199511000-00008
Šošić L, Bojnec V, Lonzarić D, JesenšekPapež B (2020) An advanced stage of carpal tunnel syndrome- is night-time splinting still effective? Int Occup Med Environ Health 33(6):771–780. https://doi.org/10.13075/ijomeh.1896.01611
Hall B, Lee HC, Fitzgerald H, Byrne B, Barton A, Lee AH (2013) Investigating the effectiveness of full-time wrist splinting and education in the treatment of carpal tunnel syndrome: a randomized controlled trial. Am J Occup Ther 67(4):448–459. https://doi.org/10.5014/ajot.2013.006031
Kruger VL, Kraft GH, Deitz JC, Ameis A, Polissar L (1991) Carpal tunnel syndrome: objective measures and splint use. Arch Phys Med Rehabil 72:517–520
Walker WC, Metzler M, Cifu DX, Swartz Z (2020) Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Arch Phys Med Rehabil 81(4):424–429. https://doi.org/10.1053/mr.2000.3856
Gatheridge MA, Sholty EA, Inman A, Pattillo M, Mindrup F, Sanderson DL (2020) Splinting in carpal tunnel syndrome: the optimal duration. Mil Med 185(11–12):2049–2054. https://doi.org/10.1093/milmed/usaa222
Page MJ, Massy-Westropp N, O’Connor D, Pitt V (2012) Splinting for carpal tunnel syndrome. Cochrane Database Syst Rev 7:CD010003. https://doi.org/10.1002/14651858.CD010003
Bland JD (2000) A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve 23(8):1280–1283. https://doi.org/10.1002/1097-4598(200008)23:8%3c1280::aid-mus20%3e3.0.co;2-y
Geler Külcü D, Bursali C, Aktaş İ, Bozkurt Alp S, Ünlü Özkan F, Akpinar P (2016) Kinesiotaping as an alternative treatment method for carpal tunnel syndrome. Turk J Med Sci 46(4):1042–1049. https://doi.org/10.3906/sag-1503-1504
Boyacı A, Tutoğlu A, Koca İ, Kocatürk Ö, Çelen E (2014) Comparison of the short-term effectiveness of short-wave diathermy treatment in patients with carpal tunnel syndrome: a randomized controlled trial. Arch Rheumatol 29:298–303. https://doi.org/10.5606/ArchRheumatol.2014.4246
Lin MT, Liao CL, Hsiao MY, Hsueh HW, Chao CC, Wu CH (2020) Volume matters in ultrasound-guided perineural dextrose injection for carpal tunnel syndrome: a randomized, double-blinded, three-arm trial. Front Pharmacol 11:625830. https://doi.org/10.3389/fphar.2020.625830
Habibzadeh A, Mousavi-Khatir R, Saadat P, Javadian Y (2022) The effect of radial shockwave on the median nerve pathway in patients with mild-to-moderate carpal tunnel syndrome: a randomized clinical trial. J Orthop Surg Res 17(1):46. https://doi.org/10.1186/s13018-022-02941-9
MacDermid JC, Wessel J (2004) Clinical diagnosis of carpal tunnel syndrome: a systematic review. J Hand Ther 17(2):309–319. https://doi.org/10.1197/j.jht.2004.02.015
Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH et al (1993) A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am 75(11):1585–1592. https://doi.org/10.2106/00004623-199311000-00002
Hunt Sonja M, McKenna SP, McEwen J, Jan W, Evelyn P (1981) The Nottingham health profile: subjective health status and medical consultations. Sos Sci Med A 15(3):221–229. https://doi.org/10.1016/0271-7123(81)90005-5
Mallik A, Weir AI (2005) Nerve conduction studies: essentials and pitfalls in practice. J Neurol Neurosurg Psychiatry 76 Suppl 2(Suppl 2):ii23-31. https://doi.org/10.1136/jnnp.2005.069138. PMID: 15961865; PMCID: PMC1765692.
Halac G, Demir S, Yucel H, Niftaliyev E, Kocamn G, Duruyen H et al (2015) Splinting is effective for night-only symptomatic carpal tunnel syndrome patients. J Phys Ther Sci 27(4):993–996. https://doi.org/10.1589/jpts.27.993
Jerosch-Herold C, Houghton J, Blake J, Shaikh A, Wilson EC, Shepstone L (2017) Association of psychological distress, quality of life and costs with carpal tunnel syndrome severity: a cross-sectional analysis of the PALMS cohort. BMJ Open 7(11):017732. https://doi.org/10.1136/bmjopen-2017-017732
McCabe SJ, Uebele AL, Pihur V, Rosales RS, Atroshi I (2007) Epidemiological associations of carpal tunnel syndrome and sleep position: is there a case for causality? Hand 2(3):127–134. https://doi.org/10.1007/s11552-007-9035-5
Patel A, Culbertson MD, Patel A, Hashem J, Jacob J, Edelstein D et al (2014) Adverse effect of carpal tunnel syndrome on sleep quality. Sleep Disord 2014:962746. https://doi.org/10.1155/2014/962746
Acknowledgements
We would like to thank all patients who participated in this research work.
Funding
This research did not receive any specific grant from funding agencies whether public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Z.K.U. and E.U. designed the study. Z.K.U., E.U., and E.U.A. collected the clinical data. Z.K.U., E.U., and E.U.A. analyzed and interpreted the patient data. All authors discussed the results, contributed to the final manuscript, and approved it. E.U. and E.U.A. discussed the results and supervised all the research process. All authors approved the final manuscript and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by Health Sciences University Diskapi Yildirim Beyazit Education and Research Hospital Local Ethics Committee (07.02.2022, 130/07). The participants received oral and written information about the study and gave their written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kirac Unal, Z., Umay, E. & Unlu Akyuz, E. Splinting in carpal tunnel syndrome—should we use it during the daytime?. Egypt Rheumatol Rehabil 50, 46 (2023). https://doi.org/10.1186/s43166-023-00214-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-023-00214-9