Abstract
Background
Presbycusis is known to accelerate mental decline processes and to cause secondary consequences such as social isolation and depression when not intervened. The association of presbycusis and presbyvestibulopathy disorders is likely. These changes in vestibular functions are closely related to cognitive functions. This study investigated the effect of hearing loss on cognitive and vestibular functions in a geriatric population.
Methods
This study was conducted with 200 participants over the age of 65. The study was conducted with three groups: individuals with normal hearing, moderate sensorineural hearing loss, and severe sensorineural hearing loss. The relationship between the participants’ responses to the Cognitive Vestibular Function Scale and their hearing levels was examined.
Results
Of the individuals with hearing loss in the study group, 55 had moderate SNHL, and 45 had severe SNHL. The age range of the participants was 65 to 91 years (71.06 ± 4.92). When the control (Group N) and study groups (Group M and Group S) were compared according to CVFS and subscale scores, they were found to be statistically different (p < 0.05). In pairwise comparisons, a significant difference (p < 0.05) was found in all pairwise combinations except Group N and Group M (p = 0.109) for the VSM subscale.
Conclusions
It was concluded that having a healthy hearing is the most influential factor for maintaining cognitive vestibular functions in the geriatric population. It was found that the degree of hearing loss primarily affects cognitive vestibular functions and that cognitive vestibular functions deteriorate more as hearing loss increases.
Similar content being viewed by others
Background
According to the latest “World Hearing Health Report” (2021) by the World Health Organization (WHO), 5.3% of the world’s population (more than 1.5 billion individuals) suffer from hearing loss. It is projected that by 2050, 2.5 billion people will have some degree of hearing loss [1]. The increase in human lifespan implies aging societies and populations worldwide, with age-related hearing loss being the third most common disorder in older adults. Even individuals without otologic problems experience a minimum of 1 dB loss in hearing thresholds each year after age 60 [2]. Therefore, the relationship between an aging society and presbycusis is gaining importance. Primary changes expected due to hearing loss include impaired auditory processing abilities and speech discrimination. Also, evidence suggests that hearing loss and deterioration in auditory functions accelerate cognitive decline processes [3, 4].
In 2019, the Classification Committee of the Bárány Association reported that older patients with chronic vestibular symptoms due to bilateral peripheral vestibular hypofunction should be diagnosed as “Presbyvestibulopathy” [5]. Therefore, presbycusis has ceased to be an isolated problem and started to be considered as a combined problem. It is foreseeable that presbyvestibulopathy and presbycusis will be among the most critical problems regarding prolonged life expectancy and quality of life. In a retrospective study by Agrawal et al. [6]. investigating the relationship between presbycusis and vestibular functions, they reported that the prevalence of vestibular dysfunction reached up to 35.4% in adults aged 40 years and older. Although there is limited information about secondary medical risk factors that may occur in vestibular dysfunction, whether symptomatic or not, vestibular dysfunction is considered among the essential causes of falls in the elderly [7].
The underlying mechanisms between hearing loss and mobility problems are not fully understood. It has been hypothesized that hearing loss may limit the cognitive resources available for mobility by increasing cognitive load, limit access to auditory cues that support spatial orientation, lead to physical or cognitive decline by causing social isolation, and may be associated with parallel declines in vestibular function (Gabriel et al. 2022). In our country, no study analyzes the effect of age-related hearing loss on cognitive-vestibular functions. The first aim of this study is to investigate the impact of hearing loss on cognitive-vestibular functions in a geriatric population. The second aim of this study is to raise awareness about the additional effects of hearing loss on individual balance, perceptual and visual-spatial abilities, and memory skills.
Methods
This study was conducted with 200 individuals over 65 without diagnosed neuro-otologic or neurodegenerative diseases. Pure tone averages were calculated by averaging the participants’ hearing thresholds at frequencies of 500, 1000, 2000, and 4000 Hz. According to the Clark classification (1981), 100 individuals with hearing thresholds within normal hearing limits were included in the control group (Group N), and 100 individuals with moderate-to-severe sensorineural hearing loss were included in the study group. The individuals in the study group refused to use hearing aids despite being offered them. In the study group, individuals with moderate and severe hearing loss were subdivided into M and S subgroups, respectively (Table 1, Fig. 1).
In this study, the Cognitive Vestibular Function Scale (CVFS) was used to examine the effect of hearing loss on vestibular and cognitive functions [8]. The scale developed by Ozkul and Konukseven (2023) to examine cognitive functions in the geriatric population with imbalance problems examines 20 questions and four sub-factors. The CVF scale is a measurement tool that allows detailed evaluation of the effects of age-related hearing loss in terms of vestibular function (VF), spatial memory (SM), visuospatial memory (VSM), and temporal memory (TM) functions. Accordingly, the first seven items question “vestibular” skills, the following five items question “SM” skills, and the following four items question “VSM and TM” skills. The scoring table of the scale is given in Fig. 2 [8]. In our study, the CVFS was adapted to the Google Forms online platform to assess the cognitive vestibular functions of the participants. The scale was administered to the participants face-to-face, and the researcher recorded the answers online. The responses of the participants were statistically analyzed based on the scale sub-factors.
Statistical analysis
IBM SPSS Statistics 25.0 package program was used for analysis (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). According to Kolmogorov–Smirnov test the parameters did not show normal distribution. Data not showing normal distribution were evaluated with non-parametric tests. The Kruskal–Wallis test was used to compare CVFS and subscale scores. For the tests found to be significantly different between the three groups (normal hearing, moderate hearing loss, and severe hearing loss), the Dunn test was performed with Bonferroni correction to make pairwise comparisons. To illustrate the results boxplots were included, ROC curves were drawn and based on the area under the curve the sensitivity and the specificity parameters were calculated. Spearman correlation analysis was used to find if the CVFS and its subscales were related to each other and age. All tests were performed at the 0.05 significance level.
Results
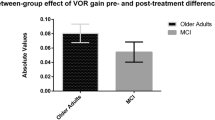
Participants’ responses to the CVFS were compared within and between groups regarding VF, SM, VSM, and TM subscale scoring and total scoring. The descriptive statistics of the CVFS and its subscales are shown in Table 2, and the boxplot chart of the scales is shown in Fig. 3.
According to CVFS and subscales scores, control (Group N) and study groups (Group M and Group S) were found to be statistically different (p < 0.05). The Mann-Whitney U test was performed using Bonferroni correction for pairwise group comparisons (Table 3). For the VSM subscale, a significant difference (p < 0.05) was found in all pairwise combinations except Group N and Group M (p = 0.109).
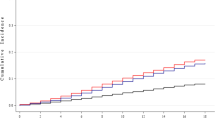
A receiver operating characteristic (ROC) curve was constructed for CVFS and its subscales, where the x-axis represents sensitivity and the y-axis defines specificity [1– − Specificity]. Sensitivity was calculated as [number of actual positive subjects] / [(number of faithful positive subjects) + (number of false negative subjects)] at various cut-off values. In contrast, Specificity was calculated as [number of faithful negative subjects] / [(number of actual negative subjects) + (number of false positive subjects)] for each cut-off value. The areas under the ROC curve (AUC) were then calculated (Fig. 4).
A larger area under the ROC curve indicates that the diagnostic test provides good measurements. An area of 1.0 represents an excellent test; an area of 0.5 represents an inappropriate test (Habibzadeh et al. 2016). The sensitivity and specificity for CVFS and its subscales are shown in Table 4. AUCs for CVFS and subscale scores were relatively large (> 0.7). These values indicate that the CVFS scale is usable.
The AUC, cut-off values, sensitivity, and specificity of CVFS and its subscales are summarized in Table 4. In the discrimination of cognitive vestibular functions according to the presence or absence of hearing loss, the cut-off value for the vestibular subscale was 17.5 (sensitivity 69%, specificity 27%); the cut-off value for the SM subscale was 11. 5 (sensitivity 74%, specificity 33%); cut-off value for VSM subscale was 8.5 (sensitivity 68%, specificity 41%); cut-off value for TM subscale was 11.5 (sensitivity 72%, specificity 28%); cut-off value for CVFS total scale was 48.5 (sensitivity 74%, specificity 28%).
Spearman correlation analysis was used for age, CVFS, and subscale scores, and p < 0.05 was considered statistically significant. The results of the analysis are given in Table 5. The correlation between scale scores and age is also shown in the Fig. 5. According to Table 5, age has a very weak positive correlation with the vestibular subscale score (r = 0.193; p < 0.01), SM subscale score (r = 0.204; p < 0.01), and CVFS total score (r = 0.181; p < 0.05). The vestibular subscale score was highly positively correlated with the SM subscale score (r = 0.769; p < 0.01), VSM subscale score (r = 0.742; p < 0.01), and temporal memory subscale score (r = 0.716; p < 0.01) and highly positively correlated with the CVFS total score (r = 0.932; p < 0.01). The SM subscale score has a highly positive relationship with the VSM subscale score (r = 0.741; p < 0.01) and CVFS total score (r = 0.890; p < 0.01) and a moderate positive relationship with the temporal memory subscale score (r = 0.652; p < 0.01). The VSM subscale score was highly positively correlated with the temporal memory subscale score (r = 0.739; p < 0.01) and CVFS total score (r = 0.886; p < 0.01). The temporal memory subscale score positively correlates with the CVFS total score (r = 0.840; p < 0.01).
The chi-square test requires an adequate sample size. The test result is valid only when no more than 20% of cells have an expected frequency value < 5 and no cell has an expected frequency value < 1 (Barceló, 2018). When the chi-square test was applied to the data set, it was seen that it did not meet the above criteria. The distribution of diagnoses related to CVFS and its subgroups by groups is given in Table 6.
According to the CVFS total score, 43% (43) of the normal hearing group were diagnosed with “normal function,” 49% (49) with “mild dysfunction,” and 8% (8) with “moderate dysfunction.” There were no individuals diagnosed with “severe dysfunction” in this group. In the group with moderate hearing loss according to CVFS total score, 18.2% (10) were diagnosed with “normal function,” 61.8% (34) with “mild dysfunction,” and 20% (11) with “moderate dysfunction.” There were no individuals diagnosed with “severe dysfunction” in this group. According to the CVFS total score, 8.9% (4) of the group with severe hearing loss was diagnosed with “normal function,” 6.7% (3) with “mild dysfunction,” 82.2% (37) with “moderate dysfunction,” and 2.2% (1) with “severe dysfunction.” According to the CVFS total score, 28.5% (57) of all participants were diagnosed with “normal function,” 43% (86) with “mild dysfunction,” 28% (56) with “moderate dysfunction,” and 0.5% (1) with “severe dysfunction.”
Discussion
This study was conducted to evaluate the cognitive vestibular function of individuals over 65 years of age with hearing loss and individuals with normal hearing. Participants’ responses to the CVF scale were analyzed comparatively.
Aging is a universal process that causes a gradual decline in the functions of various body cells, tissues, and organs. It is expected that the degree of hearing loss increases with age, which in turn may lead to impairments in cognitive vestibular functions. Our study demonstrates that the degree of hearing loss affects cognitive vestibular functions and that as the degree of hearing loss increases, there is a significant deterioration in vestibular-cognitive functions. This finding indicates that having a healthy hearing is an effective factor in maintaining cognitive vestibular functions in the geriatric population.
With age, damage to the sensory hair cells of the inner ear leads to hearing loss in the cochlea (presbycusis) and balance disturbance in the vestibular system (presbyvestibulopathy) [9]. The degree of hearing loss usually depends on the damage to the hair cells in the cochlea. Moderate hearing loss usually involves damage to the outer hair cells, whereas severe hearing loss involves damage to both the outer and inner hair cells [10, 11]. Our study revealed that 61.8% of individuals with moderate hearing loss have mild vestibular dysfunction, whereas 82.2% of individuals with severe hearing loss have moderate vestibular dysfunction. These findings support our opinion that total inner ear aging should be considered in the presence of presbycusis.
It is important to remember that the vestibular system comprises peripheral vestibular organs and their associated central nervous system projections; therefore, vestibular signals are often present together with other sensory and motor signals [12]. Several studies have examined the relationship between presbycusis and vestibular function. These studies have shown that increasing age causes degeneration of vestibular hair cells and otoliths, with a consequent decrease in vestibular ganglion cells [5, 7, 13,14,15,16]. Therefore, vestibular deficits are closely associated with balance disorders and spatial disorientation, commonly seen in neurodegenerative diseases [12, 17]. Our study has demonstrated a correlation between the degree of hearing loss and the level of vestibular insufficiency. This finding supports the view that age-related decline in vestibular sensory cells is faster in the presence of hearing loss.
Social isolation and depression are expected outcomes in individuals with hearing loss [18]. Therefore, with the aging of the world population, the relationship between hearing loss, impairments in cognitive skills, and dementia has become more critical [3, 4, 19,20,21]. The findings of our study and the existing literature suggest that the association of presbycusis and presbyvestibulopathy may cause difficulties in multimodal sensory integration and functional impairments in cognitive skills, thus increasing the risk of dementia [22,23,24]. From this perspective, presbycusis is a significant public health problem.
In a 6-year cohort study by Lin et al. [25] investigating the link between hearing loss and cognitive decline, they reported a linear change between hearing loss and spatial memory, visuospatial memory, and processing speed. Since their study mainly included individuals with mild and moderate hearing loss, they could not clearly show the correlation between the degree of hearing loss and cognitive impairments. Decreases in SM are functions closely related to a person's ability to be self-sufficient. A decrease in SM functions may lead to a loss of autonomy [26]. Various studies examining the relationship between hearing loss and SM indicate that spatial Memory deteriorates as hearing loss increases [27, 28]. There is also evidence in the literature that SM is significantly affected in older adults with vestibular hypofunction [13, 29]. The findings of our study show that spatial memory is impaired by hearing loss, and according to the subscale correlations, spatial memory is more affected when vestibular insufficiency is present.
Garami et al. [30] and Jayakody et al. [31] reported that spatial visual memory is affected by increasing hearing loss. Garami et al. [30] claimed that mild hearing loss is at least as crucial as age-related cognitive decline. Individuals with hearing loss have impaired visual-spatial memory because they cannot analyze auditory scenes well. Guidetti et al. [32] reported that individuals with normal hearing showed better VSM performance compared to individuals with hearing loss and/or vestibular deficits. Furthermore, it was shown that individuals with only vestibular deficits had worse VSM performance compared to individuals with both hearing loss and vestibular deficits. This was explained by the fact that individuals with hearing loss have improved memory functions due to their lip-reading competence and the positive effect of lip-reading on visuospatial memory. In Utoomprurkporn et al.’s [33] study, it was emphasized that lip reading is generally used by individuals with hearing loss for communication purposes, and it was stated that lip reading improves visual-spatial memory and creates the advantage of cross-model integration. Our study showed no difference between individuals with normal hearing and individuals with moderate hearing loss. However, it was observed that visual-spatial memory was impaired when hearing loss reached a severe degree. Considering that the individuals included in our study were individuals who refused auditory amplification, we concluded that there is a correlation between the degree of hearing loss and VSM disorders.
Temporal memory functions as an intermediate stop for spatial-visual and SM-processed input before it reaches the hippocampus. It is suggested that the hippocampus provides the impulse that causes short-term memory to be converted into long-term memory. Therefore, long-term memory consolidation is impossible without the hippocampus (Glasper and Gould, 2013). On account of this, any impairment in temporal memory functions has a decisive impact on quality of life, including self-sufficiency. Based on our findings, hearing loss primarily affects vestibular functions, followed by SM and VSM. Temporal memory functions are affected when all these sub-functions are affected. It should be remembered that functional impairments in temporal memory may result from this chain reaction. Studies in the literature need to examine the relationship between vestibular functions and temporal memory. Further studies in this direction will help us understand our data better.
Attentional resources play an essential role in maintaining postural control. Decreases in attentional and cognitive resources caused by hearing loss may make it challenging to maintain postural balance and increase the risk of falls (Lin and Ferrucci, 2012). In this context, hearing loss is thought to play a role as a factor that increases the risk of falling. Our study’s findings support a decrease in cognitive vestibular functions in older adults with hearing loss. In order to prevent or reduce this situation, cognitive support or rehabilitation programs to increase the attention levels of older adults with hearing loss may be considered. In addition, technological solutions such as hearing aids may help alleviate the effects of hearing loss and provide a better postural balance in daily life. Thus, necessary corrective and preventive measures can be taken against possible traumas in the geriatric population, and various interventions can be made to improve quality of life.
Limitations
This study is the first to use the CVF scale for research purposes other than the normalization study. However, our study was conducted during the COVID-19 pandemic. The individuals included in the study were over 65 years of age. Since it was not appropriate to invite this age group to hospitals and clinics under pandemic conditions, objective vestibular measurement methods could not be used. Including objective vestibular methods in future studies may contribute more to the literature.
Investigating the effect of auditory amplification on CVFs in future studies is recommended. Studies including hearing aid and non-hearing aid users and older adults with normal hearing may provide a better understanding of age-related CVF changes.
Conclusion
Our results showed that hearing loss also affects cognitive vestibular functions in older adults.
Consistent with the literature, both cognitive function and subscales, vestibular function, SM, VSM, and temporal memory showed significant differences due to the analysis. Providing amplification to individuals with hearing loss as soon as their hearing loss is detected may be of great importance in cognitive vestibular function. Further research on this subject is needed.
Especially in neurodegenerative diseases such as Alzheimer’s and dementia, auditory evaluations and amplification are recommended if necessary. Amplification has been recognized to slow the progression of these diseases [21, 34, 35].
Vestibular functions are affected depending on age. Vestibular functions are significantly impaired, especially in the presence of hearing loss. We consider that using the CVF scale to collect preliminary data about CVFs in clinics where patients over the age of 65 are examined may be a valuable tool in preventing traumatic consequences such as falls.
Since more than 5% of the world’s older adults, regular audiology evaluation, regular vestibular evaluation, regular control of cognitive functions, and auditory amplification in the presence of hearing loss may help to prevent social isolation and depression in older adults in the future.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CVF:
-
Cognitive vestibular function
- SM:
-
Spatial memory
- TM:
-
Temporal memory
- VF:
-
Vestibular function
- VSM:
-
Visuospatial memory
References
Sensory Functions (2021) DaRS, WHO-Hearing Report, WH Organization, Editor
Fischer N, Weber B, Riechelmann H (2016) Presbyakusis–altersschwerhörigkeit. Laryngorhinootologie 95(07):497–510
Völter C et al (2020) Impact of hearing loss on geriatric assessment. Clin Interv Aging. 15:2453–2467
Thomson RS et al (2017) Hearing loss as a risk factor for dementia: a systematic review. Laryngoscope Investig Otolaryngol 2(2):69–79
Agrawal Y et al (2019) Presbyvestibulopathy: diagnostic criteria consensus document of the classification committee of the Bárány Society. J Vestib Res 29(4):161–170
Agrawal Y et al (2009) Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med 169(10):938–944
Tan J et al (2016) Investigating the risk factors of vestibular dysfunction and the relationship with presbyacusis in Singapore. J Laryngol Otol 130(9):816–821
Ozkul A, Konukseven O (2023) The development of the cognitive vestibular function scale in the elderly complaints of imbalance: a study on validity and reliability. Braz J Otorhinolaryngol 89(4):101282
Furman JM, Raz Y, Whitney SL (2010) Geriatric vestibulopathy assessment and management. Curr Opin Otolaryngol Head Neck Surg 18(5):386
Huang Q, Tang J (2010) Age-related hearing loss or presbycusis. Eur Arch Otorhinolaryngol 267:1179–1191
Cunningham LL, Tucci DL (2017) Hearing loss in adults. N Engl J Med 377(25):2465–2473
Trinus K, Claussen CF (2017) International clinical protocol on vestibular disorders (dizziness). Int Tinnitus J 21(2):168–178
Previc FH et al (2014) The relationship between vestibular function and topographical memory in older adults. Front Integr Neurosci 8:46
Soto-Varela A et al (2020) Presbyvestibulopathy, comorbidities, and perception of disability: a cross-sectional study. Front Neurol 11:582038
Müller KJ et al (2022) Chronic vestibular syndromes in the elderly: Presbyvestibulopathy—an isolated clinical entity? Eur J Neurol 29(6):1825–1835
Hong JP, Kim MB (2024) Application of the Barany society's presbyvestibulopathy criteria in older adults with chronic dizziness. Otolaryngol–Head Neck Surg 170(2):515–521
Coto J et al (2021) Peripheral vestibular system: age-related vestibular loss and associated deficits. J Otol 16(4):258–265
Parham K et al (2011) Challenges and opportunities in presbycusis. Otolaryngol Head Neck Surg. 144(4):491–495
Griffiths TD et al (2020) How can hearing loss cause dementia? Neuron 108(3):401–412
Lin FR, Albert M (2014) Hearing loss and dementia–who is listening?. Aging Ment Health 18(6):671–673
Livingston G et al (2017) Dementia prevention, intervention, and care. Lancet 390(10113):2673–2734
Bosmans J et al (2024) Evidence of vestibular and balance dysfunction in patients with mild cognitive impairment and Alzheimer’s disease. Ear Hear 45(1):53–61
Smith PF (2024) Aging of the vestibular system and its relationship to dementia. Curr Opin Neurol 37(1):83–87
Zwergal A, Grabova D, Schöberl F (2024) Vestibular contribution to spatial orientation and navigation. Curr Opin Neurol 37(1):52–58
Lin FR et al (2013) Hearing loss and cognitive decline in older adults. JAMA Intern Med 173(4):293–299
Lopez A, Caffò AO, Bosco A (2021) The impact of age and familiarity with the environment on categorical and coordinate spatial relation representations. Scand J Psychol 62(2):125–133
Humes LE et al (2012) Central presbycusis: a review and evaluation of the evidence. J Am Acad Audiol 23(08):635–666
Glyde H et al (2013) The effects of hearing impairment and aging on spatial processing. Ear Hear 34(1):15–28
Caixeta GCdS, Doná F, Gazzola JM (2012) Cognitive processing and body balance in elderly subjects with vestibular dysfunction. Braz J Otorhinolaryngol 78:87–95
Garami L et al (2020) Orienting attention to auditory and visual short-term memory: The roles of age, hearing loss, and cognitive status. Exp Aging Res 46(1):22–38
Jayakody DM et al (2018) A novel study on association between untreated hearing loss and cognitive functions of older adults: baseline non-verbal cognitive assessment results. Clin Otolaryngol 43(1):182–191
Guidetti G, GuidettiR QS (2021) Sport as a factor in improving visual spatial cognitive deficits in patients with hearing loss and chronic vestibular deficit. Audiol Res 11(2):291–300
Utoomprurkporn N et al (2022) The impact of hearing loss and hearing aid usage on the visuospatial abilities of older adults in a cohort of combined hearing and cognitive impairment. Front Aging Neurosci 14:138
Bucholc M et al (2021) Association of the use of hearing aids with the conversion from mild cognitive impairment to dementia and progression of dementia: a longitudinal retrospective study. Alzheimers Dement 7(1):e12122
Dawes P (2019) Hearing interventions to prevent dementia. Hno 67(3):165
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EU: study design, supervision, data collecting, and writing—review and editing. BU: study design, data collecting, data curation and formal analysis, writing—review and editing. ÇA: study design, data collecting, and writing—review and editing. TAG: study design, data collecting. BOK: study design, supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Non-interventional Clinical Research Ethics Committee of Istanbul Aydin University, no. 2021/635 (Approval Number/Protocol Number: B.30.2.AYD.0.00.00.050.06.04/635). The participants had provided written informed consent.
Consent for publication
The study was fully explained to all the participants, and they signed an informed consent to share their data for scientific purposes.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uğur, E., Uludag, B., Aydın, Ç. et al. Evaluation of the effect of hearing loss on cognitive-vestibular functions in the geriatric population. Egypt J Otolaryngol 40, 97 (2024). https://doi.org/10.1186/s43163-024-00656-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-024-00656-8