Abstract
Purpose
This study aimed to identify the current practices and challenges faced by speech-language pathologists (SLPs) in managing dysphagia among head and neck cancer patients undergoing radiotherapy (RT) in Malaysia.
Method
A sequential, mixed-method study design was utilized in this research. Quantitative data were collected using a survey among 65 SLPs from 34 government hospitals throughout Malaysia. Additionally, 10 SLPs were selected using maximum variation sampling and interviewed for this study.
Results
The survey showed that only 7.8% of SLPs conducted therapy on all patients before RT. Moreover, the frequency of therapy during and after RT has significant relationships with the variable of time to provide intervention [χ2 (3, 63) = 13.93, p = 0.004; χ2 (3, 64) = 12.58, p = 0.007]. This study also revealed varying responses from SLPs regarding the frequency and intensity of performing home therapy programs for patients undergoing RT. Furthermore, SLP practices were divided based on the type of treatments for patients who did not experience dysphagia or mild dysphagia upon the completion of RT. Nevertheless, this study had a high agreement on the type of treatment given to patients who had completed the RT. Qualitative results showed that SLPs faced challenges in terms of a lack of awareness of their role, the establishment of multidisciplinary teams, insufficient SLPs, and inadequate equipment for assessment.
Conclusion
The study findings indicated a low standard of care in managing dysphagia among head and neck cancer patients undergoing RT and urgently call for improvements toward evidence-based practices.
Similar content being viewed by others
Background
Dysphagia management for head and neck cancer patients can be challenging due to the extensive impacts on their health and overall quality of life. Specifically, dysphagia effects are divided into three aspects: medical, psychological, and implications on the patient’s family or caregivers. Medically, dysphagia causes dehydration and malnutrition among patients, in addition to mental confusion and organ system dysfunction in the long term [1]. Malnutrition weakens the patient’s immune system, thus becoming susceptible to other diseases [2]. Consequently, their healing period is prolonged, leading to longer hospital stays. Furthermore, dysphagia can lead to aspiration pneumonia, a lung infection caused by aspirating bolus down to the trachea [3]. Psychologically, dysphagia can impact patients’ emotions and their social life. Patients who cannot eat and drink normally may suffer from depression and try to keep away from involving themselves in any social gathering [3,4,5,6]. In addition, dysphagia can impact the emotion of their carers as they might feel frustrated in scrutinising safe diet types for patients and worry about the risk of choking during mealtime [7].
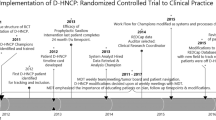
The National Cancer Registry, Ministry of Health Malaysia, reported 11,920 cases of head and neck cancer between 2012 and 2016 [8]. It is crucial to design therapy programs for head and neck cancer patients undergoing RT due to the high prevalence of swallowing problems [9]. This effort should involve a team of multidisciplinary professionals to ensure the best swallowing management, such as ENT surgeons, oncologists, phoniatricians, staff nurses, dieticians, radiologists, and SLPs [10]. The SLPs are essential in assessing and providing the optimum swallowing therapy for dysphagia patients, including assisting patients with oral consumption via swallowing rehabilitation and teaching them about compensatory techniques, such as diet modification [11]. Despite the lack of a standard guideline for effective swallowing therapy for head and neck cancer patients [12], the recommended practice is to provide swallowing therapy before and during radiotherapy (RT) [13, 14]. However, previous studies revealed that only a few SLPs provide swallowing therapy before and during RT. Lawson et al. [14] showed that only 23.5% of SLPs intervened before their head and neck cancer patients developed dysphagia, while only 18.3% intervened proactively [15]. Proactive intervention by SLPs entails swallowing intervention before or during RT, which is not exclusive to dysphagic patients [15]. Conversely, reactive intervention refers to the swallowing intervention by SLPs solely for patients who complain of dysphagia. The issue of dysphagia in patients with head and neck cancer undergoing RT is easily overlooked [16, 17] as there can be only subtle changes to lingual function [18]. Therefore, it is important to ensure all head and neck cancer patients who are undergoing RT receive ongoing monitoring and evaluated for dysphagia. To date, only two local studies have been performed by Sharma et al. [19] and Mustaffa Kamal et al. [20], but they focused on dysphagia management by SLPs in general. It is crucial to assess how well the standard practice for managing dysphagia by SLPs complies with the best practices recommended by ASHA and NICE [11, 13]. The present study aimed to identify the common practices by SLPs and the challenges they face in executing the best practices when managing dysphagia among head and neck cancer patients undergoing RT in Malaysia.
Methods
The current mixed-method research utilized the sequential explanatory study design comprising quantitative and qualitative approaches. First, quantitative data were collected using a cross-sectional study design. In total, there are 112 SLPs working in government hospitals throughout Malaysia. Of these, 71 SLPs have managed and/or are currently seeing patients with head and neck cancer and were selected to complete a questionnaire. There was a high response rate; 65 (91.5%) SLPs from 34 government hospitals completed the survey forms. For the qualitative study, ten SLPs were shortlisted via maximum variation sampling for individual interviews and semi-structured and physical face-to-face interviewing sessions. Selection of participants was based on responses obtained from questionnaires and had different characteristics such as different work setting and work experience.
Study instrument
The qualitative data was retrieved using a questionnaire adapted from Krisciunas, Sokoloff, Steps, and Langmore [15]. The questionnaire was presented in Bahasa Malaysia and divided into four parts: (1) sociodemographics (ten questions), (2) usual dysphagia practices (17 questions), (3) multidisciplinary team (five questions), and (4) infrastructure (five questions). The survey questions were in the form of demographic items, Likert scale, and multiple-choice items. First, the English version of the questionnaire was validated by an experienced English language expert to ensure the accuracy of interpretation based on the original survey in Bahasa Malaysia. Subsequently, the questionnaire was subjected to a pre-study involving four SLPs with more than 10 years of experience to get their feedback about the questions and confirm that the items were clear and precise. The questions were later improved based on their feedback. Upon completion, a pilot study involving ten SLPs who were not respondents to the study was conducted to ensure the reliability and validity of the questionnaire. As a result, high reliability (0.74) was obtained compared to before the pilot study (0.67). Lastly, a group interview session was conducted in the pilot study by two SLPs with more than 10 years of experience to ensure that the interview questions could provide the desirable answers from the respondents.
Study procedure
The ethical approval for this study was obtained from the Medical Research & Ethics Committee of the Universiti Kebangsaan Malaysia (UKM PPI/111/8/JEP-2018–570) and the Ministry of Health Malaysia (NMRR-17–3460-34710). The questionnaires were distributed physically and online to all SLPs in 34 selected hospitals after obtaining written permission from the hospital directors and heads of departments. The respondents who met the inclusion criteria were selected to answer the questionnaire. A reminder was given, via e-mail or phone call, a week after the forms were distributed. Two weeks later, the researchers collected the questionnaires from the respondents.
A 45-min, semi-structured interview was then conducted face to face with each respondent. The interview was performed using the prepared questions and several additional items to get an explanation from the respondents for incomplete answers. Specific questions were also asked as a follow-up to the questionnaire. All interviews were recorded using an MP3 audio recorder and transcribed verbatim, followed by data analysis to obtain the themes and subthemes.
Data analysis
The data that was analyzed descriptively includes the respondent’s sociodemographic data, dysphagia management practices, multidisciplinary team status, level of communication with medical and dental practitioners, and availability of assessment tools and therapy tools. A chi-square test was performed to determine the correlation between the clinical factors (referral policies) and intervention time (proactive and reactive). Furthermore, the t-test was conducted to identify the differences between the intervention time and treatment protocol. Thematic analysis with ATLASti was used in qualitative analysis.
Results
Quantitative analyses
A total of 65 SLPs completed the survey in this study (Table 1). Most SLPs were females (n = 61, 93.8%), under the age of 40 (n = 34, 52.4%), and served in the ENT departments (n = 59, 90.8%). While most SLPs had attended a general dysphagia course, only 13.8% were explicitly for head and neck cancer patients.
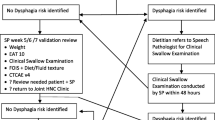
Information regarding intervention time, availability of multidisciplinary teams, and availability of assessment and therapy tools is presented in Table 2. Results showed that only 7.8% of SLPs performed intervention for all patients before RT. The majority of SLPs in this study receive written referrals (46.2%) and have basic screening (86.1%) and therapy tools (56.9%) for patient management.
The summary of chi-square analysis examining the relationship between gender, age, work site, working experience, course, and the number of patients with intervention time is presented in Table 3. Sociodemographic factors as well as dysphagia training and the total number of head and neck cancer patients did not correlate significantly with intervention time.
Chi-square test results in Table 4 show that the frequency of home programs after RT correlated significantly with intervention time [χ2 (3, 63) = 12.58, p = 0.007]. Specifically, most SLPs who intervened reactively are more likely to prescribe weekly sessions to head and neck cancer patients undergoing RT. From the t-test findings, there was no significant difference between intervention time and treatment protocol. Nevertheless, a significant relationship was observed between the treatment protocol and SLPs who underwent dysphagia course [χ2 (2, 64) = 6.35, p < 0.05]. Specifically, 91.5% of SLPs who attended dysphagia courses between 7 and 14 days and those who attended specific head and neck cancer courses would recommend swallowing exercises to patients without dysphagia after RT [χ2 (1, 62) = 5.02, p < 0.05]. The chi-square analysis also indicated that the percentage of compliance level for the patient without dysphagia (confirmed by instrumental procedure) did not correlate with the frequency of the home therapy program [χ2 (2, 56) = 0.54, p = 0.84] and intensity of the home therapy program [χ2 (1, 56) = 0.52, p = 0.71]. In addition, there was no significant relationship between the compliance level of a patient who had moderate to severe dysphagia (level of severity confirmed by instrumental procedure) with the frequency of home therapy [χ2 (2, 64) = 3.68, p = 0.36] and intensity of the therapy programme, χ2 (2, 64) = 3.66, p = 0.13.
Qualitative analysis
Personal interviews were conducted with 10 SLPs. They were all females; eight obtained bachelor’s degrees, and two have a master’s degree. Most respondents have reported working experiences of more than 6 years and have attended dysphagia courses. However, none has participated in courses specifically for dysphagia among head and neck cancer patients. The number of challenges faced by SLPs can be divided into six major themes and subthemes as follows.
Lack of infrastructure
In the present study, most respondents agreed that the lack of assessment and therapy equipment was the major challenges in managing head and neck cancer patients with dysphagia. Respondents specifically noted that “There is no VFSS” or “We do not have a visual feedback tool” or having lack of proper equipment, “… the equipment is available but incomplete,” and “we lack variety in the food type for testing, we only have rice porridge” that hinders overall patient care.
Speech-language pathologists (SLPs)
SLPs face four major challenges in managing head and neck cancer patients with dysphagia. First is the lack of knowledge about head and neck cancer which is a common challenge faced by SLPs. Respondents stated that this problem stemmed from the lack of exposure during their undergraduate training at the university “because we lack exposure during university time” and the lack of further specialised training as stated by the following excerpts: “….I think (I) need more hands-on training” and “…..not enough training in managing head and neck cancer patients with dysphagia.” The second challenge highlighted by the SLPs is the absence of a dysphagia specialist, “at this time, we do not have a senior expert that we can refer to specializing in dysphagia for stroke and head and neck cancer,” and they require support from external sites, “Yes, we usually ask external sources, an expert from outside.” The third challenge is time constraints. SLPs in government hospitals in Malaysia cater for all types of cases, “we handle many types of cases,” and are not able to focus on swallowing cases as their numbers are small, “… the swallowing cases are not many.” Respondents also mentioned time constraints as demand on SLPs to also conduct other managerial and administrative tasks, “…besides clinical work, we are required to perform management tasks. This situation is caused by the lack of clinic assistants to help us.” Fourth is shortage of SLPs. Respondents stressed that there were an insufficient number of SLPs to treat head and neck cancer patients in hospitals: “… insufficient SLP’s” as well as “… staff shortages”.
Medical and dental practitioners
The most common challenge faced by SLPs was the lack of knowledge among medical and dental practitioners about their roles. Respondents mentioned “….do not know the role of a speech therapist” and the “…lack of exposure” in the interviews. The lack of knowledge about the role of SLPs caused delays in patient referrals in the early stages of head and neck cancer diagnosis as shown in the following excerpt: “… they don't refer earlier…..”. The study findings suggest that SLPs found it challenging to fulfil the expectations of medical and dental practitioners, “ENT doctors would ask why their patients are still not improving yet,” and “specialists often demand that we see patients immediately….”.
Patients
The patients’ subthemes identified in this study were commitment and lack of psychosocial support. The following are excerpts from respondents on the commitment, particularly on the exercises to prevent swallowing problems (preventative exercise), “…Patients who do not have a problem, even though we asked them to do (the exercise), they questioned; why do it if there was no problem,” “…when we are ready to meet the patient, the patient defaults (the session),” “… patient’s commitment, the motivation is not there.” “… Patients face difficulty coming because of the difficulty parking,” “and then many patients could not work, …financially they could not attend follow-up often.” Respondents also noted the lack of psychosocial support for patients: “Poor family support and also poor social support like public support….”.
Lack of referral of cancer cases
As cancer cases were less likely to be referred to SLPs, they lacked the experience and skills to handle head and neck cancer cases. The following are some excerpts from the respondents: “… because we rarely do it and do not know,” “… the skill is not well established due to the lack of practice,” and “…not all hospitals manage large-scale swallowing cases”.
Lack of clinical practice guidelines
Respondents also stated that the lack of clinical practice guidelines is one of the challenges faced by SLPs: “… there is no clear guideline that works for head and neck patients”.
Discussion
The current study discovered that only 7.8% of SLPs conducted therapy for all head and neck cancer patients before RT, much lower than previous studies (18.3 to 23.5%) and is a cause for concern. Furthermore, 44.4% of SLPs did not perform a proper treatment protocol during RT, which was higher than previous literature (20 to 30%). Thus, most head and neck cancer patients received no intervention from SLPs. On the other hand, more than 80% of SLPs recommended compensatory techniques and stretching exercises to head and neck cancer patients undergoing RT treatment. In addition, this study showed varying responses from SLPs regarding the frequency and intensity of home therapy programs for patients undergoing RT. The study findings indicated that 42.9% of SLPs recommended therapy for 7 days per week, while 25.4% of SLPs did not recommend a home therapy program for patients undergoing RT. In contrast, Lawson et al. [14] reported that most SLPs (89.4%) recommended a weeklong therapy, and only 2% of SLPs did not prescribe the home therapy program for their patients.
This study findings also revealed a high agreement among SLPs on the type of treatment given to head and neck cancer patients with dysphagia who had completed RT. Notably, 92% of the SLPs recommended compensatory techniques, 89% suggested stretching exercises, 88% prescribed non-swallowing exercises, and 86% instructed their patients to perform swallowing exercises, consistent with Lawson et al. [14] and Krisciunas et al. [15]. Nevertheless, there were discrepancies among SLPs regarding the type of treatment for patients who did not experience dysphagia or mild dysphagia after completing their RT. The SLPs (49.2%) also highlighted the lack of a treatment protocol for head and neck cancer patients who did not experience dysphagia or mild dysphagia and have completed RT, which aligned with Lawson et al. (45%) [14] and Krisciunas et al. (52.6%) [15]. Additionally, 33 to 41.3% of SLPs expressed uncertainty in recommending other therapies (E-stim, massages, and acupuncture) to head and neck cancer patients with or without dysphagia due to their lack of exposure to these treatments. In addition, most SLPs (90.5%) recommended a home therapy program of 7 days per week to patients with dysphagia after RT, which was higher than previous studies [14, 15].
The SLP work experience did not affect the intervention time and treatment protocol recommendations in this study, consistent with Lawson et al. [14]. In contrast, Krisciunas et al. [15] reported that work experience had a significant relationship with the recommended intervention time. The results indicated that SLPs with working experience of 5 years and above provided 3.5 times more proactive interventions than those who have been in service for less than 5 years. In addition, the former were five times more likely to recommend some dysphagia therapy during RT than the latter. This study also discovered that work experience had no significant relationship with proactive interventions and types of therapy for dysphagia, which may be caused by the small sample size. Nevertheless, this study demonstrated that the number of dysphagia courses attended by SLPs influenced the types of dysphagia therapy they prescribed. For instance, SLPs who have attended a dysphagia course are more likely to provide swallowing exercises than those without prior training.
The qualitative findings highlighted the challenges faced by SLPs in Malaysia in handling head and neck cancer patients, thus further supporting the survey findings. The most frequent challenge faced by SLPs is the lack of awareness of their role among medical and dental practitioners, which affects the number of head and neck cancer patients referred to them. Likewise, earlier studies reported that the level of awareness about the role of SLPs among medical practitioners remained low [21,22,23]. Secondly, the SLPs emphasized the absence of a multidisciplinary team in managing dysphagia in head and neck cancer patients in Malaysia. There were early signs of an informal multidisciplinary establishment between ENT specialists and SLPs. The study results showed that 43.1% of ENT specialists held oral meetings with SLPs to refer specific cases, while 10.7% held meetings to refer all head and neck cancer cases. Dysphagia programs are most successful when they involve perspectives from a variety of medical disciplines [24]. The results of the study also showed that a common challenge was the low number of SLPs [25, 26]. The insufficient number of SLPs made it difficult for therapists to provide prompt and intensive services to head and neck cancer patients. The next challenge was the inadequacy of assessment equipment. Only 10.8% of SLPs admitted having complete assessment tools, including FEES and VFSS equipment. A local study by Mustaffa Kamal, Ward, and Cornwell [27] found that 13.3% of SLPs had never used VFSS equipment. This indicates the need to establish a VFSS procedure to ensure that dysphagia patients undergo a comprehensive and holistic assessment as well as the absence of skilled internal SLPs in handling head and neck cancer patients. These challenges reflect poorly on overall patient care.
Conclusion
Overall, this study’s findings demonstrated that Malaysian SLPs’ care of head and neck cancer patients is far from optimal, and when it is done correctly, it is limited to a few highly skilled SLPs. This study also identifies the challenges faced by SLPs in providing services beyond the bare basics and suggests that imperative effort be made in the overall management of dysphagia patients through cohesive collaboration with medical practitioners based on evidence and international standards.
Availability of data and materials
The datasets used and/or analyzed in the current study are available from the corresponding author on request.
References
Groher ME, Crary MA (2016) Clinical management in adults and children. Mosby Elsevier, USA
Clavé P, Rofes L, Arreola V, Almirall J, Cabré M, Campins L et al (2011) Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract. https://doi.org/10.1155/2011/818979
Cichero J, Murdoch B (2006) Dysphagia: foundation, theory and practice. John Wiley & Sons Ltd, Chichester
Ekberg O, Hamdy S, Woisard V, Hannig A-W (2002) Social and psychological burden of dysphagia: it is impact on diagnosis and treatment. Dysphagia 17:139–146
Martino R, Beaton D, Diamant NE (2010) Perceptions of psychological issues related to dysphagia differ in acute and chronic patients. Dysphagia 25:26–34
Patterson JM, McColl E, Wilson J, Carding P, Rapley T (2015) Head and neck cancer patients’ perceptions of swallowing following chemoradiotherapy. Support Care Cancer 23(12):3531–3538. https://doi.org/10.1007/s00520-015-2715-8
Nund RL, Ward EC, Scarinci NA, Cartmill B, Kuipers P, Porceddu SV (2014) Carers’ experiences of dysphagia in people treated for head and neck cancer: a qualitative study. Dysphagia 29(4):450–458. https://doi.org/10.1007/S00455-014-9527-8
National Cancer Registry (2019) Malaysian Cancer Statistics: data and figure for Peninsular Malaysia. Ministry of Health Malaysia, Malaysia
Rinkel RN, Verdonck-de Leeuw IM, Doornaert P, Buter J, de Bree R, Langendijk JA, Aaronson NK, Leemans CR (2016) Prevalence of swallowing and speech problems in daily life after chemoradiation for head and neck cancer based on cut-off scores of the patient-reported outcome measures SWAL-QOL and SHI. Eur Arch Otorhinolaryngol 273(7):1849–1855
Licitra L, Keilholz U, Tahara M, Lin J-C, Chomette P, Ceruse P et al (2016) Evaluation of the benefit and use of multidisciplinary teams in the treatment of head and neck cancer. Oral Oncol 59:73–79. https://doi.org/10.1016/J.ORALONCOLOGY.2016.06.002
American Speech-Language-Hearing Association (2008) Communication facts: special population: dysphagia-2008 edition. Retrieved From http://www.asha.org/
American Speech-Language-Hearing Association (2018) Head and neck cancer. Retrieved From https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589943346§ion=Treatment
National Institute for Health and Clinical Excellence (2004) Improving outcomes in head and neck cancers. The Manual, Guidance on Cancer Services, 43–47
Lawson N, Krisciunas GP, Langmore SE, Castellano K, Sokoloff W, Hayatbakhsh R (2016) Comparing dysphagia therapy in head and neck cancer patients in Australia with international healthcare systems. Int J Speech Lang Pathol 9507(October):1–11. https://doi.org/10.3109/17549507.2016.1159334
Krisciunas GP, Sokoloff W, Stepas K, Langmore SE (2012) Survey of usual practice: dysphagia therapy in head and neck cancer patients. Dysphagia 27(4):538–549. https://doi.org/10.1007/s00455-012-9404-2
Shune SE, Karnell LH, Karnell MP, Van Daele DJ, Funk GF (2012) Association between severity of dysphagia and survival in patients with head and neck cancer. Head Neck 34(6):776–784
Teguh DN, Levendag PC, Sewnaik A, Hakkesteegt MM, Noever I, Voet P, Est HVD, Sipkema D, Rooij PV, De Jong R, Schmitz PIM (2008) Results of fiberoptic endoscopic evaluation of swallowing vs. radiation dose in the swallowing muscles after radiotherapy of cancer in the oropharynx. Radiother Oncol 89(1):57–63
King SN, Dunlap NE, Tennant PA, Pitts T (2016) Pathophysiology of radiation-induced dysphagia in head and neck cancer. Dysphagia 31(3):339–51. https://doi.org/10.1007/s00455-016-9710-1. Epub 2016 Apr 20. PMID: 27098922; PMCID: PMC5340192
Sharma S, Harun H, Kamal RM, Noerdin S (2006) Pengendalian Disfagia Oleh Patologis Pertuturan-Bahasa di Malaysia. Jurnal Sains Kesihatan Malaysia 4(2):39–51
Mustaffa Kamal R (2012) Exploring dysphagia management practices and barriers to service improvement in Malaysia. PhD Thesis in Speech Language Pathology. The University of Queensland
Kayani SA, Butt AK (2014) Dysphagia; awareness & knowledge of medical practitioners and understanding of role of SLP in its assessment & management. J Riphah Coll Rehabil Sci 3(1):25–29
Mustaffa Kamal R, Ward EC, Cornwell P (2013) Levels of awareness, involvement and training in dysphagia management among other health professionals in Malaysia. Dysphagieforum 3(1):4–15
Xinyi D, Ahmad A, Vesualingam M (2018) Medical officers’ awareness, involvement and training in dysphagia management. Malaysian J Health Sci Jurnal Sains Kesihatan Malaysia 16(1):7–16. https://doi.org/10.17576/JSKM-2018-1601-02
Langmore SE (1999) Issues in the management of dysphagia. Folia Phoniatr Logop 51(4–5):220–230. https://doi.org/10.1159/000021499
Roe JWGG, Carding PN, Rhys-Evans PH, Newbold KL, Harrington KJ, Nutting CM (2012) Assessment and management of dysphagia in patients with head and neck cancer who receive radiotherapy in the United Kingdom - a web-based survey. Oral Oncol 48(4):343–348. https://doi.org/10.1016/j.oraloncology.2011.11.003
Modi N, Ross E (2000) The current practices, training and concerns of a group of hospital-based speech therapists working in the area of dysphagia. S Afr J Commun Disord 47:3–14. https://doi.org/10.4102/sajcd.v47i1.217
Mustaffa Kamal R, Ward E, Cornwell P (2012) Dysphagia training for speech-language pathologists: implications for clinical practice. Int J Speech Lang Pathol 14(6):569–576. https://doi.org/10.3109/17549507.2012.713394
Acknowledgements
We would like to thank the Director General of Health Malaysia for the permission to publish this article.
Funding
This study was funded by the Ministry of Health, Malaysia, under Hadiah Latihan Persekutuan.
Author information
Authors and Affiliations
Contributions
All authors were involved in the concepts and design of the study. HH and ZY were involved in the literature search and data analysis. HH, KA, SEWP, ZY, and HMI edited and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received the ethical approval from the Medical Research and Ethics Committee of the Universiti Kebangsaan Malaysia (UKM PPI/111/8/JEP-2018–570) and the Ministry of Health Malaysia (NMRR-17–3460-34710). Informed written consent to participate in the study was provided by all participants.
Consent for publication
Written consent from the patients was obtained. No images or videos were related to an individual person in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hussain, H., Ahmad, K., Yahaya, Z. et al. Dysphagia therapy for head and neck cancer patients undergoing radiotherapy by speech-language pathologists in Malaysia. Egypt J Otolaryngol 39, 137 (2023). https://doi.org/10.1186/s43163-023-00495-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00495-z