Abstract
Background
Damage to the inner ear or cochlear nerve results in sensorineural hearing loss (SNHL), which is typically persistent deafness. SNHL can range in severity from mild to profound. The shape of the audiogram is used to categorise it as high-frequency hearing loss, low-frequency, flat, peaked, or notched. Pure tone audiometry can be used to diagnose SNHL.
Objective
To summarise the recent updates in the usage of stem cells in sensory neural hearing loss (SNHL).
Methods
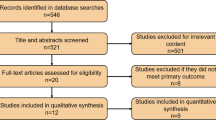
Published studies about using stem cell therapy in ENT practice through comprehensive PubMed, EKG, and Google Scholar search (from 2010 to 2022). Including studies in English, experimental studies, and studies that discuss the application of regenerative medicine in SNHL.
Results
Progenitor stem cells may be employed to repair damaged cells and restore sensorineural hearing function, according to 36 of the publications. The majority of these articles—about 90%—discussed animal model-based experimental investigations; the remaining 10% were clinical trials.
Conclusion
The application of stem cells in the treatment of SNHL will be a significant step in the future since it will change the way that patients are now treated in the hopes of regaining their hearing. The application to the clinical setting is still in its early stage, although a number of encouraging researches illustrate how progenitor stem cells differentiate into sensorineural cells.
Similar content being viewed by others
Background
A persistent sensory disorder known as sensorineural hearing loss (SNHL) affects about 270 million people globally. In newborns, the frequency of SNHL is 2/1000; in children between the ages of 3 and 17, it is 5/1000; in adults between the ages of 65 and 74, it is 33%; and in people over the age of 85, it is 50% [1]. Modern therapies (such as hearing aids and cochlear implants) aim to boost remaining sensory hair cells from Corti organ’s damage in order to lessen SNHL’s symptoms. The depletion of sensory hair cells within the organ of Corti limits the effect of cochlear implants. As they transform sound mechanical waves into electrical signals that are then sent to the brain. So, inner, outer, and structural hair cells are crucial for hearing [2].
Hearing impairment is caused by a reduction in auditory input to the brain, which is brought on by the loss of sufficient hair cells. Because the organs of Corti are post-mitotic at birth in animals, there is no future spontaneous hair cell regeneration. Genetic mutations account for between 23 and 50% of SNHL in babies and young children (Connexin 26 mutations deafness, Lange-Nielson syndrome, Pendred syndrome, Usher syndrome, Waardenburg syndrome, etc.). The remaining newborns and kids are affected by SNHL, which is commonly brought on by premature birth, illness during or after delivery, loud exposure, or the use of ototoxic medicines [3]. Regenerative medicine has dramatically improved in the previous 10 years, as has its use in surgical disorders. The therapeutic applications of regenerative science are currently pushing the limits of every surgical specialty [4].
Intravascular infusion of mesenchymal progenitor cells in acute neuropathologic disturbances has been studied in preclinical and clinical studies (traumatic brain haemorrhage, stroke, spinal cord injury, etc.) and has shown great promise. Cochlear repair was observed in intentionally deafened mice that received mononuclear cells from human umbilical cord blood (HUCB) [5].
In mucopolysaccharidosis patients, the SNHL has improved after myeloablation and HUCB transplantation. The cell populations that are most frequently used in this research are the bone marrow mononuclear fraction and the HUCB mononuclear fraction. For the bone marrow therapies, a bone marrow harvest is required. The HUCB therapy utilises a heterogeneous cell population rich in progenitor cells that are collected and cryopreserved at birth. A paediatric population typically has access to enough cells and only requires minimal cell processing. We can prevent cell rejection, the spread of blood-borne diseases, and the possibility of graft vs. host disease by using an autologous cell product. A neuropathologic injury to the organ of Corti known as acquired SNHL may be responsive to HUCB therapy [6].
Aim of the work
This systematic review/meta-analysis aims to summarise the recent updates in the usage of stem cells in sensory neural hearing loss (SNHL).
Methods
Criteria for considering studies for this review
-
Types of studies: Any type of study was included.
-
Types of participants: Review of animal studies and analysis of human studies
-
Types of interventions: Stem cell therapy
-
Types of outcome measures: Otoacoustic distortion product emissions (DPOAE). Auditory brainstem response to sound (ABR).
Search strategy for identification of studies: Published studies about using stem cell therapy in ENT practice through comprehensive PubMed/Google Scholar/ EKB search (from 2010 to 2022) using a variety of medical subject headings and free text words: Regenerative Medicine; Stem Cells; Pluripotent; biohybrid; Head and neck cancer, sensory neural hearing loss (SNHL), tissue engineering, reconstructive surgical techniques, otorhinolaryngology, otology, audiology. We looked at studies in English and made no translation attempts.
Methods of the review
Locating and selecting studies: Articles that appear to meet the inclusion requirements were retrieved in full after utilising the aforementioned search approach to view the articles. Each identified article was examined and put into one of the following groups:
-
Included: Studies in English, experimental studies, and studies that discuss the application of regenerative medicine in SNHL.
-
Excluded: Not in English language, duplicated material & Review articles.
-
Data extraction: Two reviewers independently extracted the data and cross-checked it.
Statistical considerations
Software called Review Manager was used to combine the results from the included trials. The causes of study heterogeneity were investigated, and if necessary, a sensitivity analysis based on the use of random versus fixed effects modelling and methodological quality was carried out. Subgroup analyses are planned based on timing of interventions and duration of the follow-up.
Evidence of publication bias was sought using the funnel plot method.
Results
Analysis of animal studies
Between 2010 and 2022, eleven studies were published; nine studies met the inclusion criteria: four from South Korea, one from the USA, two from Japan, one from Australia, and one from China. Animal and mesenchymal stem cell (MSC) features are summarised in Table 1, whereas specific study findings are presented in Table 2. Animals used in the studies were guinea pigs (n = 3), rats and mice (n = 8), and pigs (n = 1) as illustrated in Table 3. Half of the studies included gender information, and three of them used only male animals. Pharmacologic induction was the most popular technique for obtaining SNHL (n = 7). The auditory brainstem response was the most popular functional hearing test (n = 11). There were only six studies with quantifiable data to be included in the review, despite the bulk of articles suggesting the usefulness of ABR as a hearing test. Labelling assays, optical microscopy, and immunohistochemistry can be used to evaluate the secondary effects of MSC and cochlear colonisation (n = 6). To assess the immunological response to MSC delivery, inflammatory cytokine profiles and T-helper cell activation (n = 3) were analysed.
The origin of MSCs was very varied, with the majority of studies (n = 9, 75%) obtaining them from a xenogeneic source. In most trials, MSCs generated from bone marrow or foetal tissue were given as a one-time dosage. MSCs were given in doses ranging from 4103 to 1107 cells.
Half of the studies satisfied all of the international society for cell and gene therapy (ISCT) criteria for defining an MSC. Positive indicators (n = 9) and distinction capabilities (n = 9) were the most often mentioned criteria. Dulbecco’s Eagle medium with fetal bovine serum was the most popular MSC growing medium, and cell passage numbers ranged from 3 to 15.
The auditory function
The two tests used to evaluate auditory function were the auditory brainstem response (ABR) and the distortion product otoacoustic emissions (DPOE) (N = 832 animal comparisons; 6 investigations; 95% confidence interval [17.62, 12.82]; Fig. 1). Performance of the ABR as a whole improved by − 15.22db spl. The ABR tests showed low variability [I 2 = 37%, p = 0.005] (N = 700 animal comparisons across 4 trials; 95% CI [8.07, 10.13]; Fig. 2). DPOAE performance as a whole improved by 9.10. The amount of heterogeneity in DPOAE was considerable [I 2 = 88%, p 0.0001]. None of the research looked at brainstem summating potentials, compound action potentials, tympanometry, electrocochleography, or auditory evoked potentials.
MSC recovery/engraftment
To gauge MSC recovery, spiral ganglion neuron (SGN) density was used. The average number of cells that were different overall was 14.79 (95% confidence interval: [14.01, 15.57]; 4 investigations, n = 107 animal comparisons; Fig. 3). Significant heterogeneity was discovered (I 2 = 97%, p 0.00001).
For studies that used ABR testing, additional stratifications were carried out with indications of significant variations in effect size. People, who employed MSCs from the umbilical cord or placenta, did better than those who employed cells from other sources, for instance (27; 95% CI [36, 17.5]). In the trials that were taken into consideration, research on guinea pigs (27; 95% CI [36, 17.5]), animals 4–8 weeks old (25; 95% CI [30, 20]), inducing SNHL pharmacologically (17; 95% CI [20, 14.6]), and xenogeneic studies are all included (− 18.96; 95% CI [21.71); the effect size was greatest after an injection of more than 107 cells (27; 95% confidence interval [CI]: [36, 17.5]), between 1 and 2 weeks after SNHL induction and when it was delivered extracochlearily (25; 95% CI [30, 21.5]) (23.2; 95% CI [27, 19.7]). Additionally, numerous administrations resulted in a higher ABR (25; 95% CI [30, 20.7]). The DPOAE-based study was not capable of subgroup analysis.
Analysis of human studies
In 2014, Hua Liu et al. presented a case of SSNHL in a 48-year-old male in a conference in Wuhan, China, who was not responding to medical treatment for 1 month. An alternative approach with human umbilical cord-derived mesenchymal stem cells (UC-MSCs) was applied to this patient by intravenous injection. After the second injection of UC-MSCs, the patient presented significant improvement in hearing compared to that 1 month ago.
Human mononuclear cells were disengaged from bone marrow BM-MNC by Roemer et al. in 2016. To make a speedy and productive cell covering process for cochlear embed electrode, fibrin glue was utilised as a transporter for BM-MNC. Utilising this technique, biohybrid wire for intracochlear cell-based drug conveyance may be made in that area in the operation theatre. The presentation of the biohybrid electrode beat the ordinary, non-covered cochlear implant utilised in the other ear. Between the two operated ears, the impedances and discourse insight were differentiated.
All patients had equivalent impedances on both sides and had acceptable hearing (Fig. 4). In one patient, hearing with the biohybrid implant was better than on the other ear; in other hearing was similar, and in the last one the standard cochlear implant was preferable than the biohybrid implant. Five months after implantation, none of the individuals manifested any regrettable side effects.
In 2018, Ho Seok et al. carried out multiple pilot experimental trials for sensorineural hearing loss patients. They set up a subclavian line before the transplant to ensure a secure infusion. Under general anaesthetic, bone marrow-derived stem cells were mixed with regular saline, then administered by intravenous infusion. To ensure that the stem cells were successfully transferred to the cochlea, they applied electrical currents measuring 1.5 mA to the cochlear promontory.
Case 1
A woman aged 67 years who had had a retro-sigmoid craniotomy was found to have hearing loss. Her pure tone thresholds on the right were off by 15 dB and out of scale on the left. The left and right auditory brainstem response thresholds were both off by 30 dB. Prior to surgery, the safety evaluation was also examined. Her urine, coagulation, haematology, and biochemistry tests all came back negative. The outcomes demonstrated that there were no problems or negative consequences associated with stem cell therapy. The outcomes of the haematology, biochemistry, and coagulation laboratory tests did not change either. However, throughout a 12-month period, they did not observe any alterations in their hearing (attributed to individual sensations, PTA, and ABR). After 3 years of administration, there were no problems with the stem cell transplantation.
Case 2
A man aged 55 years old reported having hearing loss on both sides of his hearing. The right and left audiometry thresholds were 47.5 dB and 46 dB, respectively. The ABR result was the same as the pure tone average when both thresholds were set to 60 dB. For the aim of safety evaluation, haematology, biochemistry, coagulation, and urine tests were looked at and found to be all within normal range.
Additionally, there were no systemically related complications. He underwent hearing tests (PTA, OAE, and ABR) every month for the next 12 months, but they were unable to detect any improvement in his hearing. After 3 years of infusion, there was no adverse effect with stem cell therapy.
In 2018, Linda S. Baumgartner et al. conducted research on the effects of intravenous autologous hUCB on eleven children with moderate to severe acquired SNHL, aged 6 months to 6 years. Five individuals are categorised as having “acquired SNHL” because they underwent neonatal screening but later experienced hearing loss. The six cases are categorised as having “congenital SNHL” since they failed neonatal screening. Genetic testing for SNHL markers was unfavourable in nine patients. The other two subjects contracted CMV while still in the womb. There were no negative outcomes and eleven patients made it. Haemodynamic alterations unrelated to the infusion did not take place. There was no evidence of infusion-related toxicity. Thresholds for the auditory brainstem response (ABR) decreased in five participants. Cochlear nerve latencies also improved in four of those five patients. When MRI with diffusion tensor imaging (DTI) sequences from before and after treatment were compared, three of five participants with lower ABR thresholds had higher fractional anisotropy (FA) in the primary auditory cortex. There have been ABR threshold reductions that are statistically significant (p 0.05).
Discussion
Stem cells may be embryonic origin or from adult tissues, as a product of multicellular organism. Within the developing embryo, stem cells can be differentiated into any type of specialised animal tissue and also can be utilised to exchange specialised cells and maintain the traditional turnover of regenerative organs as in blood, skin, intestines, and the body’s repair system within the adult organs [16].
Undifferentiated cells, additionally called pluripotent stem cells, will give any of the 3 germinal layers (ectoderm, mesoderm, and endoderm) and may differentiate into various types of specialised cell sorts. They even have a limitless capability for self-renewal through multiple cycles of mitotic cell division [17,18,19]. These qualities of pluripotent stem cells indicate a variety of potential clinical applications, like recombinant protein therapy, drug discovery and development, and regenerative medicine [20, 21]. The best source of pluripotent stem cells up till recently were embryonic stem cells or cells from the inner cell mass of the blastula around biological process days 5 to 8 [17]. Pluripotent stem cells, which are comparable to embryonic stem cells, can be produced by genetically reprogramming human or mouse cells to cause the generation of pluripotent stem cells. These cells can be found in a variety of tissues, including umbilical cord blood [22,23,24,25,26,27].
Compared to embryonic stem cells, which have the capacity to give rise to all functional cell types, including neurons, cardiomyocytes, and hemopoietic cells, these induced pluripotent stem cells are more potent [28,29,30]. In addition to resolving the moral dilemma surrounding the use of human embryonic stem cells from aborted embryos, the genetic induction of adult mouse or human tissues to produce induced pluripotent stem cells has also resolved the difficulty of producing disease-specific embryonic stem cells [31].
As proven in mice models of sensorineural hearing loss, direct genetic processing provides an indisputable method of producing sufficient quantities of patient-specific induced pluripotent stem cells for stem cell therapy [32]. In the inner ear, stem cells were used in experiments to differentiate into hair cells and regenerate auditory neurons. In the labyrinth, stem cells are used by experimentation with the hope that they would someday turn out to be hair cells and audile neurons, foetal dorsal root neural cells [33, 34], neural ancestor cells [35, 36], labyrinth stem or progenitor cells [37,38,39], immortalised audile formative cell cells [40, 41], embryonic stem cells and their derived somatic cell cells [34, 37, 42], and additionally as marrow stromal cells treated with sonic hedgehog and retinoic acid [43].
Stem cells with the ability to differentiate into auditory neurons can be used to replace degenerated nerve fibres after the onset of sensorineural hearing loss [44]. Coleman et al. [44] tested two models for their own ability to differentiate mice embryonic stem cells in vitro. Stem cells were stimulated to generate neural precursors using retinoic acid before it is co-cultured with detached rat auditory neurons or hair cells derived from postnatal day 5 rat pups. The cultivation of entire embryoid tissues with hair cell explants produced a large number of bipolar cells with structure and neural protein expression similar to human auditory neurons cultured in vitro. As a result, hair cell tissue and embryoid body co-cultures are likely to be useful or powerful for obtaining data that promote auditory neuron development in vitro. Consequently, further research is needed to discover if the neuron-like cells generated by these therapies are successful and exhibit the electrical characteristics of auditory neurons developed in vivo.
Surprisingly, regardless of the cause of sensorineural hearing impairment, the degenerative alterations are frequently comparable; hence, molecular production of the damaged neurons and later implantation shows promise. The next step in this process may be to figure out how to protect the regenerated organelles against further pathological destruction, particularly as a consequence of autoimmune illness. At the same time, the fact that some individuals with autoimmune illnesses have effective organ transplant surgeries is thought-provoking human ethical considerations that have vigorously fought progress in this scientific sector. Nonetheless, new technologies have offered alternatives to the usage of embryos, utilising various stem cell research methods. Once these new methods are allowed, stem cell research ought to be able to move further without the need for embryo bodies.
Clinically, such technical advancement is expected to enable significant progress in gene therapy and the therapeutic treatment of several disputable genome-related disorders, such as sensorineural deafness.
Future directions
There are clinical difficulties involved with the management of noise-related hearing impairment as contrasted to considerations for abrupt hearing loss. In contrast to a one-time incidence, most noise-induced deafness is the product of decades of continuous workplace exposure. As a result, the most typical suggestion is to avoid exposure to loud noises. Treatment for NIHL must begin in a quiet location away from high amplitude noises, since any improvement brought about by treatment may be countered by ongoing noise. This presents the dilemma of treating an old hearing impairment vs the desired outcomes from a younger person’s ear. The urgent need for technological advances such as gene editing and regenerative medicine research may aid in treating these difficulties, leading to improved hearing results even in the elderly ear.
Regardless of the apparent power of genetic engineering and stem cell treatment, one likely challenge that must be addressed is defining the strategy and vehicle of delivery. Direct injection into the round window membrane, oval window, and lastly to the scala tympani or scala vestibuli through cochleostomy are the three primary techniques investigated for gene therapy [45, 46]. The blood-labyrinthine barrier’s integrity may hypothetically retain the medicinal agent concentration inside the cochlea, while convection diffusion across the organ should allow for equitable distribution of the active ingredient to distal parts of the inner ear [47].
However, any of these ways has the potential to disrupt the high potassium concentration of the endolymph to the perilymph, which may affect the integrity of these spaces. Viral vectors have been proposed as a promising delivery method, with effectiveness demonstrated in lab animals. Adenovirus and lentiviruses have been utilised in vitro and in vivo among many others [46, 47]. However, their safety and efficacy have not yet been validated in human studies because of the possibility of unanticipated mutations and long-term biological effects at the site of transplantation. More research is needed before these types of treatment can be considered a viable therapeutic technique in clinical settings.
Multiple experiments used auditory brainstem response (ABR) for measuring the efficacy of stem cell treatment in improving hearing function. However, the findings of several studies varied. In addition to the experiments included in the review, three investigations revealed a significantly decreased ABR threshold at all frequencies tested [12,13,14], and one study discovered visible waveforms in animals on day 3 following MSC implantation [14]. Regarding histological evidence of MSC migration of the cochlea, one study discovered no statically big difference in ABR thresholds in primed recipient animals [10].
Significant research has revealed that MSCs can differentiate into cochlear tissue, indicating that implanted stem cells can repair hearing and promote hair cell healing. High noise or ototoxic damage to the cochlea, according to Choi et al., induces the synthesis of mediators that encourage stem cell attachment and penetration [10]. This is demonstrated by the recruitment of stem cells toward the spiral (cochlear) ganglion, as well as the production of brain-derived neuroprotective factor (BDNF). On the other hand, Pandit investigated whether direct stem cells injection into the cochlea stimulates convergence into cochlear tissue and discovered that olfactory stem cells were not found in the organ of Corti and spiral ganglia but accumulated in the scala vestibuli and tympani [7]. Ma, on the other hand, discovered that MSCs introduced into the subarachnoid space diffuse to several parts of the cochlea about 4 weeks after implantation including the basal membrane, stria vascularis, and spiral ganglion [14].
According to current research, MSCs may be able to reduce inflammatory process. Two studies suggest that after MSC treatment, the generation of IL-10 produced by T regulatory cells suppresses T helper 1 and 17 [9, 13]. Some of the experiments were conducted on immune-compromised animals, and the authors ignored to describe any major side effects or implications of cellular rejection.
Furthermore, the fact that the majority of these delivery methods are dependent on surgical approaches, as well as their uncertain long-term effectiveness, may compel the creation of a less disruptive and generally applicable form of delivery. The possible delivery techniques for stem cells are really being evaluated, and we are still making gradual but steady progress toward developing a clinically viable procedure. Finding the complicated differentiation process relevant to restore inner ear hair cellular function is another significant issue for stem cell-based treatment. Wnt, catenin, and Notch are among the most well-documented signalling pathways [46], but there are still several interplays and cross-interactions to be defined in order to make stem cells implantation to the host simple and, most importantly, safe with no negative consequences.
Despite these obstacles, genome editing and regenerative medicine can be utilised in conjunction with conventional medicines. Given the large number of people affected by SNHL, it is critical that we keep pushing this barrier by investigating the clinical applications of gene and stem cell therapy. Another potential issue is the lack of a documented clinical guideline for SNHL, indicating that there is room for improvement in terms of clinician agreement and comprehension. Given the likely impact on a broad population pool in addition to its impact on health care costs, it is more important than ever to study innovative treatment methods for SNHL in order to minimise its terrible socioeconomic impact while also increasing the people’s quality of life with NIHL. With technological advancements, genome editing and stem cell treatments will open up new possibilities for developing successful treatment solutions for SNHL.
Conclusion
Human studies have not yet largely succeeded. Yet, stem cell therapy and other regeneration technologies appear to be the way of the future for treating resistive sensorineural hearing loss. As a result, there is a must for more clinical trial research in this field of regenerative medicine.
Availability of data and materials
All data are provided in this study and raw data can be requested to the corresponding author.
References
Lin FR, Niparko JK, Ferrucci L (2011) Hearing loss prevalence in the United States. Arch Intern Med 171(20):1851–1852
Mehra S, Eavey RD, Keamy DG (2009) The epidemiology of hearing impairment in the United States: newborns, children, and adolescents. Otolaryngol Head Neck Surg 4(140):461–472
Sheearer AE, Shibata SB, Smith RJH (2020) Genetic sensorinerual hearing loss. In: Flint PW, Haughey BH, Lund VJ, Niparko JK, Robbins KT, Thomas JR, et al, editors. Cummings Otolaryngology—Head and Neck Surgery, 7th edn. Saunders, an imprint of Elsevier, Philladepphia, p 2279-2292
Orlando G, Baptista P, Birchall M, De Coppi P, Farney A, Guimaraes-Souza NK, ..., Soker S (2011) Regenerative medicine as applied to solid organ transplantation: current status and future challenges. Transpl Int 24(3):223–232
Cox CS, Baumgartner JE, Jimenez F, Gee A, Harting MT (2011) Autologous Bone Marrow Mononuclear Cell Therapy for Severe Traumatic Brain Injury in Children. Neurosurgery 68(3):588–600
van Velthoven CT, Dzietko M, Wendland MF, Derugin N, Faustino J, Heijnen CJ, ..., Vexler Z S (2017) Mesenchymal stem cells attenuate MRI-identifiable injury, protect white matter, and improve long-term functional outcomes after neonatal focal stroke in rats. J Neurosci Res 5(95):1225–1236
Pandit SR, Sullivan JM, Egger V, Borecki AA, Oleskevich S (2011) Functional effects of adult human olfactory stem cells on early-onset sensorineural hearing loss. Stem Cells 29(4):670–677
Zhou Y, Yuan J, Zhou B, Lee AJ, Lee AJ, Ghawji M Jr, Yoo TJ (2011) The therapeutic efficacy of human adipose tissue-derived mesenchymal stem cells on experimental autoimmune hearing loss in mice. Immunology 133(1):133
Choi BY, Song J, Chang SO, Kim SU, Oh SH (2012) Intravenous administration of human mesenchymal stem cells after noise- or drug- induced hearing loss in rats. Acta Otolaryngol 5(3):50–55
Choi BY, Song JJ, Chang SO, Kim SU, Oh SH (2012) Intravenous administration of human mesenchymal stem cells after noise-or drug-induced hearing loss in rats. Acta Otolaryngol 132(SUPPL. 1):S94–S102
Kasagi H, Kuhara T, Okada H, Sueyoshi N, Kurihara H (2013) Mesenchymal stem cell transplantation to the mouse cochlea as a treatment for childhood sensorineural hearing loss. Int J Pediatr Otorhinolaryngol 6(77):936–942
Yoo TJ, Du X, Zhou B (2015) The paracrine effect of mesenchymal human stem cells restored hearing in β-tubulin induced autoimmune sensorineural hearing loss. Hear Res 330(Pt A):57–61
Kil K, Choi MY, Kong JS, Kim WJ, Park KH (2016) Regenerative efficacy of mesenchymal stromal cells from human placenta in sensorineural hearing loss. Int J Pediatr Otorhinolaryngol 100(91):72–81
Ma Y, Guo W, Yi H, Ren L, Zhao L, Zhang Y, ..., Yang S (2016) Transplantation of human umbilical cord mesenchymal stem cells in cochlea to repair sensorineural hearing. Am J Transl Res 8(12):5235
Chen W, Jongkamonwiwat N, Abbas L, Eshtan SJ, Johnson SL, Kuhn S, ..., Rivolta MN (2012) Restoration of auditory evoked responses by human ES cell-derived otic progenitors. Nature 490(7419):278
Coleman B, Fallon JB, Gillespie LN, de Silva MG, Shepherd RK (2007) Auditory hair cell explant co-cultures promote the differentiation of stem cells into bipolar neurons. Exp Cell Res 313(2):232
Munsie MJ, Michalska AE, O’Brien CM, Trounson AO, Pera MF, Mountford PS (2000) Isolation of pluripotent embryonic stem cells from reprogrammed adult mouse somatic cell nuclei. Curr Biol 10(16):989–992
Nichols J, Smith A (2012) Pluripotency in the embryo and in culture. Cold Spring Harb Perspect Biol. 4(8):a008128. https://doi.org/10.1101/cshperspect.a008128. PMID: 22855723; PMCID: PMC3405859.
Ulloa-Montoya F, Verfaillie CM, Hu W (2005) Culture systems for pluripotent stem cells. J Biosci Bioeng 100:12–27
McNeish IA, Bell SJ, Lemoine NR (2004) Gene therapy progress and prospects: cancer gene therapy using tumour suppressor genes. Gene Ther 11:497–503
Vats A, Tolley NS, Bishop AE, Polak JM (2005) Embryonic stem cells and tissue engineering delivering stem cells to the clinic. J R Soc Med 98:346–350
Ratajczak MZ, Zuba-Surma EK, Machalinski B, Kucia M (2007) Bone-marrow-derived stem cells – our key to longevity? J Appl Genet 48:307–319
Takahashi K, Yamanaka S (2006) Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126:663–676
Maherali N, Sridharan R, Xie W, Utikal J, Eminli S, Arnold K et al (2007) Directly reprogrammed fibroblasts show global epigenetic remodeling and widespread tissue contribution. Cell Stem Cell 7:55–70
Wernig M, Meissner A, Foreman R, Brambrink T, Ku M, Hochedlinger K et al (2007) In vitro reprogramming of fibroblasts into a pluripotent ES-cell-like state. Nature 448:318–324
Barrilleaux B, Phinney DG, Prockop DJ, O’Connor KC (2006) Ex vivo engineering of living tissues with adult stem cells. Tissue Eng 12:3007–19
Scheper W, Copray S (2009) The molecular mechanism of induced pluripotency: a two-stage switch. Stem Cell Rev 5:204–23
Wernig M, Lengner CJ, Hanna J, Lodato MA, Steine E, Foreman R et al (2008) A drug-inducible transgenic system for direct reprogramming of multiple somatic cell types. Nat Biotechnol 26:916–24
Hanna MC, Calkins DJ (2007) Expression of genes encoding glutamate receptors and transporters in rod and cone bipolar cells of the primate retina determined by single-cell polymerase chain reaction. Mol Vis 13:2194–208
Dimos JT, Rodolfa KT, Niakan KK, Weisenthal LM, Mitsumoto H, Chung W et al (2008) Induced pluripotent stem cells generated from patients with ALS can be differentiated into motor neurons. Science 321(12):18–21
Yamanaka S (2007) Strategies and new developments in the generation of patient-specific pluripotent stem cells. Cell Stem Cell 1:39–49
Bodmer D (2008) Protection, regeneration and replacement of hair cells in the cochlea: implications for the future treatment of sen- sorineural hearing loss. Swiss Med Wkly 138:47-8-708–12
Hu Z, Ulfendahl M (2006) Cell replacement therapy in the inner ear. Stem Cells Dev 15:449–459
Regala C, Duan M, Zou J, Salminen M, Olivius P (2005) Xenografted fetal dorsal root ganglion, embryonic stem cell and adult neural stem cell survival following implantation into the adult vestibu- locochlear nerve. Exp Neurol 193:326–333
Corrales CE, Pan L, Li H, Liberman MC, Heller S (2006) Edge AS Engraftment and differentiation of embryonic stem cell- derived neural progenitor cells in the cochlear nerve trunk: growth of processes into the organ of Corti. J Neurobiol 66:1489–500
Ito A, Shinkai M, Hakamada K, Honda H, Kobayashi T (2001) Radiation-inducible TNF-alpha gene expression under stress- inducible promoter gadd 153 for cancer therapy. J Biosci Bioeng 92:598–601
Li CQ, Liu D, Wu XQ (2004) Differentiation of rat bone marrow stromal cells into neuron-like cells [in Chinese]. Zhong Nan Da Xue Xue Bao Yi Xue Ban 29:18–20
Doetzlhofer A, White PM, Johnson JE, Segil N, Groves AK (2004) In vitro growth and differentiation of mammalian sensory hair cell progenitors: a requirement for EGF and periotic mesenchyme. Dev Biol 272:432–47
Rask-Andersen H, Boström M, Gerdin B, Kinnefors A, Nyberg G, Engstrand T et al (2005) Regeneration of human auditory nerve. In vitro/in video demonstration of neural progenitor cells in adult human and guinea pig spiral ganglion. Hear Res 203:180–91
Nicholl AJ, Kneebone A, Davies D, Cacciabue-Rivolta DI, Rivolta MN, Coffey P et al (2005) Differentiation of an auditory neuronal cell line suitable for cell transplantation. Eur J Neurosci 22:343–53
Hildebrand MS, de Silva MG, Klockars T, Rose E, Price M, Smith RJ et al (2004) Characterization of DRASIC in the mouse inner ear. Hear Res 190:149–60
Sekiya T, Kojima K, Matsumoto M, Kim TS, Tamura T, Ito J (2006) Cell transplantation to the auditory nerve and cochlear duct. Exp Neurol 198:12–24
Kondo T, Johnson SA, Yoder MC, Romand R, Hashino E (2005) Sonic hedgehog and retinoic acid synergistically promote sensory fate specification from bone marrow-derived pluripotent stem cells. Proc Natl Acad Sci U S A 102:4789–94
Coleman B, de Silva MG, Shepherd RK (2007) Concise review: the potential of stem cells for auditory neuron generation and replacement. Stem Cells 25:2685–94
Shu Y, Tao Y, Wang Z, Tang Y, Li H, Dai P, Gao G, Chen Z-Y (2016) Identification of adeno-associated viral vectors that target neonatal and adult mammalian inner ear cell subtypes. Hum Gene Ther 27:687–699
Mittal R, Debs LH, Nguyen D, Patel AP, Grati M, Mittal J, Yan D, Eshraghi AA, Liu XZ (2017) Signaling in the auditory system: implications in hair cell regeneration and hearing function. J Cell Physiol 232(10):2710–2721
Ahmed H, Shubina-Oleink O, Holt JR (2017) Emerging gene therapies for genetic hearing loss. JARO 18:649–670
Acknowledgements
The authors are gratefully indebted to Allah the most kind and the most merciful, otherwise not applicable.
Funding
No funding agency was granted for this study at any stage of work.
Author information
Authors and Affiliations
Contributions
Conceptualisation, WF; methodology, WF; validation, AA; formal analysis, OM; resources, OM; data curation, AA; writing—original draft preparation, GE; writing—review and editing, OM; supervision, WF; all authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Committee of Scientific Research, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mady, O.M., Ezzat, W.F., Askoura, A.M. et al. Stem cell therapy in sensorineural hearing loss: a systematic review. Egypt J Otolaryngol 39, 153 (2023). https://doi.org/10.1186/s43163-023-00452-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00452-w