Abstract
Background
Congenital aural atresia (CAA) and stenosis is a rare defect affecting the external auditory canal which causes varying degrees of hearing impairment. This malformation may be unilateral or bilateral. Timely hearing rehabilitation in these patients is paramount to ensure appropriate speech and language development. Thus, early detection and hearing assessment with timely intervention in the form of hearing device is crucial. There is a wide range of hearing amplification devices available for these patients, catering to individual needs and preferences. This study investigated the options and choices of hearing rehabilitation among patients with CAA in our center. This study also compared the hearing gain of different types of hearing devices and patient satisfaction levels.
Methods
This was a retrospective analysis of 55 patients with congenital aural atresia or stenosis under follow-up at the Otorhinolaryngology and Audiology Clinic of a tertiary academic institution. Data on the timing of hearing loss diagnosis and intervention, type of hearing rehabilitation, hearing gain, Jahrsdoerfer score from temporal bone computed tomography, and patient satisfaction level was collected and analyzed.
Results
Fifty-five patients were recruited with ages between 3.6 months to 58 years old. The majority of patients (63.6%) had moderate hearing loss, followed by severe hearing loss (18.2%), mild hearing loss (9.1%) and profound hearing loss (7.3%). 32.7% of patients had early hearing loss diagnosed by 3 months old, while 67.3% were diagnosed after 3 months of age. Bone anchored hearing implant (BAHA Attract/Connect) gave the highest mean hearing gain of 35.23 dB (SD ± 9.75) compared to air conduction hearing aid, bone conduction hearing aid, and canalplasty. Patients implanted with BAHA Attract/Connect reported the highest average satisfaction scores of 7.74.
Conclusion
A significant proportion of patients have delayed diagnosis and intervention. Bone-anchored hearing implants provide excellent hearing improvements in patients with CAA with good patient satisfaction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Congenital aural atresia (CAA) and stenosis is a malformation of the external auditory canal in which there is an incomplete development of the ear canal resulting in hearing deficits. It occurs as a result of failure in the embryological development of the first branchial arch whereby the first branchial groove epithelial plate does not canalize (atresia) or has incomplete canalization (stenosis) [1]. The majority of patients with CAA have a malformed (microtia) or absent (anotia) external ear. This malformation is unilateral in most patients and has a tendency to be right-sided [1, 2]. It may occur as an isolated entity or associated with a variety of chromosomal abnormalities such as Trisomy 13, 18, and 22 [3]. This malformation is also seen as part of some syndromes such as Treacher-Collins and Goldenhar [4].
Prompt diagnosis and intervention is essential in accordance with the 2019 position statement by the Joint Committee of Infant Hearing which outlines that hearing screening should be completed by one month of age, audiological assessment by 3 months of age, and early intervention by 6 months of age [5, 6]. Delay in diagnosis and intervention will lead to significant negative implications to the child’s speech and language development [7]. This is due to the narrowed or absent external ear canal which causes substantial conductive hearing loss of up to 60dBHL on the affected side [7].
Hearing rehabilitation for patients with CAA is the mainstay of management. There are several options available that cater to different patient populations. After birth, hearing amplification should be offered without delay once the child has undergone the necessary medical and audiological assessments. The most common and practical option is a bone conduction hearing aid (BCHA) in the form of a headband or softband. As the child grows older, other treatment options can be considered, such as reconstructive surgery and implantable hearing devices. Implantable hearing devices aim to amplify sound via bone conduction which directly stimulates the cochlear. With the latest advances, implantable hearing aids have shown promising results in terms of audiological benefits. Whereas atresia reconstructive surgery aims to create a clean, dry external ear canal to improve hearing. A helpful guide in determining if a patient would benefit from atresia surgery is the Jahrsdoerfer classification [4]. Quality of life (QOL) scores following hearing intervention have also shown significant benefits [8, 9].
Traditionally, hearing rehabilitation has been emphasized in cases of bilateral CAA while patients with unilateral CAA were thought to be able to compensate with the normal ear. However, this perception is no longer valid as recent studies have shown evidence that children with unilateral CAA have significant delays in speech/language development and suffer from poorer school performance [10].
The Joint Committee of Infant Hearing has recommended early hearing detection and intervention to optimize auditory perception, speech and language development [6]. In our local setting, newborn hearing screening has been implemented in stages in government hospitals, initially focusing on high-risk infants and later expanding to include all infants [11]. This study aimed to evaluate the timing of hearing loss diagnosis and intervention in this group of patients. This study also identified the types of hearing rehabilitation available in our center for this group of patients and compared the hearing gain between the type of hearing aids.
Methods
This was a descriptive observational study with a convenience sampling method. Ethics approval was obtained from Medical Research and Ethics Committee, National University of Malaysia (FF-2020–043). Patients under follow-up at the Otorhinolaryngology and Audiology Clinic of a tertiary academic institution diagnosed with congenital aural atresia/stenosis were identified from the existing clinic census and case mix database as well as during clinic appointments. These patients were invited to participate in the study during their scheduled appointments or via a telephone call. Patients with missing file records or incomplete data, or with less than 6 months of follow-up duration were excluded.
The written informed consent was obtained from all recruited patients who were of the age to give consent. However, for patients who were below 18 years of age, consent was obtained from their parents. Data was collected from the patients using a data collection sheet during the scheduled appointments or via a telephone call. High-resolution computed tomography (HRCT) scan of the temporal bone was reviewed and Jahrsdoerfer scoring done accordingly. Patients were categorized according to the timing of hearing loss diagnosis and intervention based on the recommendations by the Joint Committee of Infant Hearing [6].
Hearing assessments with pure tone audiometry (PTA) or auditory brainstem response performed before and after hearing intervention were reviewed and analyzed. The results of hearing thresholds at frequencies of 0.5, 1, 2, and 4 kHz pre- and post-intervention were used to calculate hearing gain [12, 13]. The hearing gain was calculated as the difference between pre-intervention and post-intervention air conduction hearing thresholds. Patient satisfaction towards their hearing aid was assessed using a 10-point Likert scale in which 0 is least satisfied and 10 indicates most satisfied.
Statistical analysis
Data analysis was performed using the IBM Statistical Package for Social Sciences (SPSS) version 26.0. All p values < 0.05 are considered as statistically significant. Descriptive statistics were calculated, where frequency and percentage were calculated for categorical data, and mean, median, standard deviation, and ranges for continuous data. Comparison between the usage of hearing aids with unilateral versus bilateral affected ears and the hearing thresholds was done using Fisher’s exact test. Independent t-test was used to compare the hearing gain between the different types of hearing rehabilitation options.
Results
There was a total of 55 patients recruited in this study. The mean age of the patients was 14.37 years (± 11.18). The oldest patient was 58 years old and the youngest was 3.6 months old. There were 36 (65.5%) male and 19 (34.5%) female patients. The majority of the patients were of Malay ethnicity (54.4%), followed by Chinese (36.4%) and Indian (9.1%). Seventeen (30.9%) patients had other associated syndromic features (refer to Table 1). Four patients were diagnosed in our center, while fifty-one patients were diagnosed in other hospitals before being referred to our center for further management.
Thirty-five (63.6%) patients had congenital aural atresia/stenosis affecting one ear with 20 patients having bilateral ear affected. Out of the 55 patients, six (10.9%) patients had canal cholesteatoma. These patients’ hearing levels ranged from normal hearing to profound hearing loss bilaterally. Specifically, 1.8% of patients had normal hearing, 9.1% had mild hearing loss, 63.6% had moderate hearing loss, 18.2% had severe hearing loss, and 7.3% had profound hearing loss (refer to Table 2).
HRCT of the temporal bone was done in 46 patients during the study period. Of these patients, 24 had favorable Jahrsdoerfer scores of seven or more while 22 patients had unfavorable Jahrsdoerfer scores. Canalplasty was performed for eight patients, of which six had favorable anatomy based on the Jahrsdoerfer grading scale. Canalplasty was done in six patients in view of the presence of canal cholesteatoma. Only two patients underwent canalplasty primarily for hearing rehabilitation (refer to Table 3).
The timing of diagnosis of hearing loss in most patients (67.3%) was after 3 months of age. 20% of patients were diagnosed between 3 months to 1 year old, while 47.3% were diagnosed after 1 year old (refer to Table 4). Only 37 (67.3%) patients subsequently underwent hearing rehabilitation. Most patients (78.4%) had late intervention (refer to Table 5).
In terms of types of hearing rehabilitation, seven (9.1%) patients were fitted with a bone-anchored hearing implant (BAHI), which was either BAHA Connect or BAHA Attract. Eight (14.5%) patients underwent canalplasty, eight (14.5%) patients opted for air conduction hearing aid (ACHA) while 14 (25.5%) patients were fitted with bone conduction hearing aid (refer to Table 6 and Fig. 1). Of the 37 patients who received hearing rehabilitation, 13 subsequently changed to a different type of hearing aid. Twelve patients transitioned to BAHI while one patient who was fitted with air conduction hearing aid later underwent canalplasty for canal cholesteatoma.
A significant association was found between the usage of hearing aids with the number of affected ears, in which bilateral affected ear is significantly associated with the use of hearing aid (p = 0.001). Moderate to severe hearing loss was also significantly associated with hearing aid usage. However, the number of affected ears and degree of hearing loss were not significantly associated with earlier diagnosis (p = 0.533, p = 0.140).
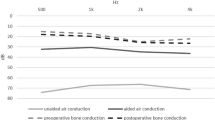
The highest mean hearing gain after hearing rehabilitation was 35.23 dB (SD ± 9.75) for BAHA Connect/Attract, followed by 30.23 (SD ± 12.15) for air conduction hearing aid, 29.54 dB (SD ± 5.70) for bone conduction hearing aid and least was 9.06 dB (SD ± 7.61) for canalplasty. A comparison of hearing gain was done between BAHA Connect/Attract, ACHA, BCHA, and canalplasty using an independent T-test. A significant difference in hearing gain was seen between canalplasty and BAHA Connect/Attract (p < 0.001) only. There was no significant difference in hearing gain between BAHA Connect/Attract with bone conduction hearing aid or air conduction hearing aid. All patients who received BAHA Connect/Attract reported the highest average satisfaction score of 7.74 out of 10 (refer to Table 7 and Fig. 2).
Discussion
Congenital aural atresia (CAA) and stenosis is a rare external auditory canal defect resulting from aberrant development of the first branchial arch and its derivatives [3, 12]. The term CAA encompasses varying degrees of deformity from stenosis to complete absence of the external auditory canal.
The demographic results in this study are similar to those in existing literature in which the condition is commonly unilateral and tends to affect the right side [1, 2]. Among our study population, a proportion of our patients were syndromic, most of which had Goldenhar syndrome.
Our study showed most patients were diagnosed and intervened late after 3 months and 6 months of age respectively. Most of our patients (94.6%) were referred from other centers, in which the timing of hearing assessments may vary. Our findings are similar to a recent local analysis which reported 81% of infants did not complete diagnostic audiological assessments within 3 months. Likewise, global surveys reported an average age of diagnosis of 4.6 months and 34.9 months for screened and unscreened infants respectively [14]. Hamzah and colleagues [15] identified late referrals and long waiting time for appointments as factors leading to delayed diagnosis. This is exacerbated by a lack of awareness among healthcare professionals, where a local study revealed only 20% had good knowledge on newborn hearing screening and 22% were not aware of the program [16]. This is compounded by poor knowledge among mothers regarding childhood hearing loss and its impact [17]. Other factors contributing to delayed diagnosis are parental denial or confusion, late recognition by parents and lack of explanation by professionals [15].
Our study also found that patients with moderate to severe hearing loss were more likely to receive hearing aids, indicating that the degree of hearing deficit affected patients’ choice to seek hearing rehabilitation. Chien and Lin [18] found that the take-up rate for hearing aids was highly related to the severity of hearing loss. This could be due to the hearing loss having a greater impact on their ability to hear and carry out their daily routines [19]. Unfortunately, our study did not find a significant correlation between the severity of hearing loss and earlier diagnosis. This may indicate the hearing loss was undetected due to a lack of access to hearing screening facilities in some centers. 63.6% of our patients had unilateral CAA and half did not adopt any form of hearing rehabilitation. A possible explanation is that the hearing deficit may not have caused an obvious impairment. Thus, the parents or patients themselves probably did not find it crucial to seek treatment. Similarly, Golub et al. [20] reported individuals with unilateral hearing loss to have low hearing aid usage.
Other than that, a significant proportion of patients (32.7%) did not proceed with hearing rehabilitation. Most of these patients who did not receive hearing rehabilitation had unilateral CAA with mild to moderate hearing loss. Again, unilateral hearing loss had previously been thought to be of little consequence, and hearing rehabilitation was not emphasized in this group of patients [7]. However, over the last decade, numerous studies show significant speech, educational and behavioral deficits in these patients [21]. Therefore, these patients and their parents/carers should have adequate counseling to dispel any misconceptions towards hearing devices.
Based on the results of this study, hearing loss detection and intervention among our patients are not within the recommended timeframe by the Joint Committee of Infant Hearing [6]. Late diagnosis could be attributed to poor understanding of the condition among patients and carers, leading to delayed intervention. Difficult access to information may also play a role. Thus, more initiatives to raise public awareness are needed to educate on the importance of early hearing rehabilitation in these patients.
In our study, a large proportion of patients opted for non-surgical bone-conduction hearing aids such as the softband BAHA, ADHEAR, and conventional bone-conduction hearing aid. Early hearing amplification with these devices can be instituted in infants as young as 3 months old [22]. The major advantage of the bone-conduction hearing aid is its ease of application and non-invasive nature, making it recommended for children awaiting other forms of hearing aids. Fourteen patients in our study who had opted for bone-conduction hearing aids later proceeded with bone-anchored hearing implant (BAHI). Studies by Goh et al. [23] and Mazita et al. [24] demonstrate that BAHI has reliable hearing outcomes in addition to being easy to handle, comfortable, and cosmetically acceptable [8].
The option of atresia reconstructive surgery or canalplasty in CAA requires assessment with high-resolution computed tomography (HRCT) temporal to help decide if the patient will benefit from surgery. It aims to create a clean, dry external auditory canal to facilitate amplification-free hearing. The CT gives valuable information on the status of the middle and inner ear as well as the presence of cholesteatoma. Based on CT, the Jahrsdoerfer classification is a useful guide to determine if a patient would benefit from atresia surgery [4]. For most centers, a Jahrsdoerfer score of 7 and above is considered favorable for canalplasty. Complications of this surgery include restenosis, facial nerve palsy, and recurrent canal infections [12, 22]. Bouhabel et al. [12] reported that 26% of patients will need a repeat surgery and 30% will still require a conventional hearing aid post-surgery. In addition, post-canalplasty care involves toileting and dressing which needs the patient’s cooperation, hence young children may not be ideal candidates. In this study, canalplasty was performed for eight patients, of which six patients had favorable Jahrsdoerfer scores while 2 patients had unfavorable Jahrsdoerfer scores. The indication for canalplasty in most patients in our study was canal cholesteatoma. This is because canalplasty has poorer hearing outcomes compared to BAHI and is a technically challenging surgery with relatively higher rates of complications [25].
The audiological benefits of hearing rehabilitation in patients with CAA are undeniable. There have been numerous studies comparing between the different options of hearing rehabilitation. In our study, BAHA Connect/Attract achieved the highest functional gain (35.23 dB; SD ± 9.75) compared to other types of rehabilitation. Bone-anchored hearing implants have been established as being superior to external auditory canal reconstruction (EACR) [12, 26]. Even in patients with favorable Jardoerfer scoring, canalplasty does not achieve comparable hearing gain as BAHA Connect /Attract. Thus, canalplasty as an option of hearing rehabilitation is not the best choice but is done primarily for canal cholesteatoma while BAHA Connect/Attract should be considered as one of the main solutions for individuals with CAA. In our study, 14 patients transitioned to BAHA Connect/Attract. Previous studies have shown that BAHA Connect/Attract has improved patient’s quality of life and well-being as well as giving immense satisfaction with regard to comfort, speech perception, and ease of use [8, 9]. This was consistent with our finding that individuals who received BAHA Connect/Attract had the highest satisfaction scores (mean 7.74).
Conclusion
A significant proportion of patients have delayed diagnosis and intervention emphasizing the need for improved access and more initiatives to ensure timely identification of hearing loss and intervention. Bone-anchored hearing implants provide excellent hearing improvements in patients with CAA with good patient satisfaction. Non-surgical options include air conduction hearing aids and bone conduction hearing aids which provide modest audiological benefits. Canalplasty still has a role in cases of canal cholesteatoma and in reconstruction of the atretic canal despite poor hearing gain.
Limitations
In this study, most of our patients were referred from multiple centers thus results may not accurately reflect data specific to our center. Late referrals and delays in obtaining an appointment may contribute to the delay in hearing diagnosis and intervention. Additionally, these patients may be referred from hospitals far from our center and have logistic problems causing the late consultation. In some patients referred from other hospitals, the referring hospital did not provide initial diagnostic hearing assessment results. Thus, the timing of hearing loss diagnosis was obtained from the parents or caretakers which may result in recall bias. Other than that, this study did not assess the speech outcome of patients as our sample population included patients of all ages with different speech skills which could not be standardized.
Recommendation
Further prospective and long-term studies to evaluate the outcome of hearing rehabilitation in these patients. We also recommend that programs to improve access to hearing screening facilities and more initiatives are needed to ensure timely identification of hearing loss and intervention in these patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nicholas BD, Kesser BW (2013) Unilateral aural atresia: current management issues and results. Curr Otorhinolaryngol Rep 1:92–98. https://doi.org/10.1007/s40136-013-0014-9
Frenzel H (2018) Hearing rehabilitation in congenital middle ear malformation. Adv Otorhinolaryngol 81:32–42. https://doi.org/10.1159/000485525
Cabrejo R, Persing J, Alperovich M (2019) Epidemiologic assessment of microtia in over 23 million consecutive United States Births. J Craniofac Surg 30:342–346. https://doi.org/10.1097/SCS.0000000000004885
Tsang WSS, Tong MCF, Ku PKM et al (2016) Contemporary solutions for patients with microtia and congenital aural atresia – Hong Kong experience. J Otol 11:157–164. https://doi.org/10.1016/j.joto.2016.11.001
Joint Committee on Infant Hearing (2007) Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. Pediatrics 120:898–921. https://doi.org/10.1542/peds.2007-2333
Joint Committee on Infant Hearing (2019) Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J Early Hear Detect Interv 4:1–44. https://doi.org/10.15142/fptk-b748
Declau F, Cremers C, Van De Heyning P et al (1999) Diagnosis and management strategies in congenital atresia of the external auditory canal. Br J Audiol 33:313–327. https://doi.org/10.3109/03005369909090115
Rahim SA, Goh BS, Zainor S et al (2018) Outcomes of bone anchored hearing aid implant at Universiti Kebangsaan Malaysia Medical Centre (UKMMC). Indian J Otolaryngol Head Neck Surg 70:28–32. https://doi.org/10.1007/s12070-017-1193-3
McDermott AL, Williams J, Kuo M et al (2009) Quality of life in children fitted with a bone-anchored hearing aid. Otol Neurotol 30:344–349. https://doi.org/10.1097/MAO.0b013e31818b6491
Jensen DR, Grames LM, Lieu JEC (2013) Effects of aural atresia on speech development and learning: Retrospective analysis from a multidisciplinary craniofacial clinic. JAMA Otolaryngol - Head Neck Surg 139:797–802. https://doi.org/10.1001/jamaoto.2013.3859
Abdullah A, Hazim MYS, Almyzan A et al (2006) Newborn hearing screening: Experience in a Malaysian hospital. Singapore Med J 47:60–64
Bouhabel S, Arcand P, Saliba I (2012) Congenital aural atresia: Bone-anchored hearing aid vs. external auditory canal reconstruction. Int J Pediatr Otorhinolaryngol 76:272–277. https://doi.org/10.1016/j.ijporl.2011.11.020
Fuchsmann C, Tringali S, Disant F et al (2010) Hearing rehabilitation in congenital aural atresia using the bone-anchored hearing aid: Audiological and satisfaction results. Acta Otolaryngol 130:1343–1351. https://doi.org/10.3109/00016489.2010.499879
Neumann K, Euler H, Chadha S, White K (2020) A Survey on the Global Status of Newborn and Infant Hearing Screening. J Early Hear Detect Interv 5(2):63–84
Hamzah NFA, Umat C, Harithasan D, Goh BS (2021) Challenges faced by parents when seeking diagnosis for children with sensorineural hearing loss. Int J Pediatr Otorhinolaryngol 143:110656. https://doi.org/10.1016/j.ijporl.2021.110656
Mazlan R, Min WS (2018) Knowledge and attitude of Malaysian healthcare professionals towards newborn hearing screening program. Malaysian J Public Heal Med 20:30–39
Wong YA, Mukari SZMS, Harithasan D, Mazlan R (2019) Knowledge and attitude on childhood hearing loss among mothers and mothers-to-be in urban and rural areas in Malaysia. Int J Pediatr Otorhinolaryngol 124:79–84. https://doi.org/10.1016/j.ijporl.2019.05.040
Chien W, Lin FR (2012) Prevalence of hearing aid use among older adults in the United States. Arch Intern Med 172:292–293. https://doi.org/10.1001/archinternmed.2011.1408
Popelka MM, Cruickshanks KJ, Wiley TL et al (1998) Low prevalence of hearing aid use among older adults with hearing loss: The epidemiology of hearing loss study. J Am Geriatr Soc 46:1075–1078. https://doi.org/10.1111/j.1532-5415.1998.tb06643.x
Golub JS, Lin FR, Lustig LR, Lalwani AK (2018) Prevalence of adult unilateral hearing loss and hearing aid use in the United States. Laryngoscope 128:1681–1686. https://doi.org/10.1002/lary.27017
Priwin C, Jönsson R, Magnusson L et al (2007) Audiological evaluation and self-assessed hearing problems in subjects with single-sided congenital external ear malformations and associated conductive hearing loss. Int J Audiol 46:162–171. https://doi.org/10.1080/14992020601077984
Lo JFW, Tsang WSS, Yu JYK, et al (2014) Contemporary hearing rehabilitation options in patients with aural atresia. Biomed Res Int 2014:. https://doi.org/10.1155/2014/761579
Farnoosh S, Mitsinikos FT, Maceri D, Don DM (2014) Bone-anchored hearing aid vs. reconstruction of the external auditory canal in children and adolescents with congenital aural atresia: a comparison study of outcomes. Front Pediatr 2:498–500. https://doi.org/10.3389/fped.2014.00005
Mazita A, Wan Fazlina WH, Abdullah A et al (2009) Hearing rehabilitation in congenital canal atresia. Singapore Med J 50:1072–1076
Nadaraja GS, Gurgel RK, Kim J, Chang KW (2013) Hearing outcomes of atresia surgery versus osseointegrated bone conduction device in patients with congenital aural atresia: A systematic review. Otol Neurotol 34:1394–1399. https://doi.org/10.1097/MAO.0b013e3182a36065
Farnoosh S, Tania Mitsinikos F, Maceri D, Don DM (2014) Bone-anchored hearing aid vs. reconstruction of the external auditory canal in children and adolescents with congenital aural atresia: A comparison study of outcomes. Front Pediatr 2:1–7. https://doi.org/10.3389/fped.2014.00005
Acknowledgements
Not applicable
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
BSG, AA, and WFWH contributed to the study design and facilitated the patient recruitment in clinic. RL did the data collection and analysis and wrote the manuscript. BSG made substantial contributions to the study conception and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of National University of Malaysia. Ethics code: FF-2020-043. The written informed consent was obtained from all recruited patients who were of the age to give consent. However, for patients who were below 18 years of age, consent was obtained from their parents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lim, R., Abdullah, A., Wan Hashim, W.F. et al. Hearing rehabilitation in patients with congenital aural atresia: an observational study in a tertiary center. Egypt J Otolaryngol 39, 90 (2023). https://doi.org/10.1186/s43163-023-00436-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00436-w