Abstract
Background
Cochlear implantation (CI) is an electronic hearing device that is surgically implanted to bypass damaged portions of the ear and directly stimulate the auditory nerve. Nowadays, CI prospects for children with profound hearing loss (HL) have been significantly improved. Now, most implanted children can expect similar audiological outcomes to those with moderate to severe HL with aids depending on the time of loss and cognitive function.
Aim
This study aimed at assessing the progress in all aspects of language acquisition and the effect of various factors on the outcome of cochlear implantation in children undergoing auditory training for at least 2 years after surgery.
Results
The results showed the effectiveness of early implantation in terms of improvement in linguistic skills, indicated by significant change of language age scores when compared before and after surgery (median age 1.167 years to 4.75 years with p value < 0.0001). Significant improvement in degree of hearing level (HL median from 100 dB to 25 with p value < 0.0001), in addition to its effect on improving the general IQ (mean from 82.42 ± 9.46 to 88.61 ± 8.13 with p value = 0.006) and abstract IQ scores (mean from 83.48 ± 9.81 to 94.45 ± 10.41 with p value = 0.0001).
Conclusion
CI children showed significant improvement in speech perception, auditory skills, and IQ scores as well as receptive and expressive language after CI denoted by the improvement of language age. Significant improvement was found in early implantation age (under 2 years) in the postoperative degree of hearing level and in language test scores in comparison to older aged children.
Similar content being viewed by others
Background
Hearing loss (HL) is the most common sensory deficit in children particularly in developing countries; one to three of every 1000 live births per year have sensorineural hearing loss (SNHL), with a profound > 90 dB HL (decibels Hearing Level) deficit. Depending on their age at the onset of HL, it can be roughly divided into pre-lingual HL (more common) and post-lingual HL (less common). The lack of auditory input from surroundings and speech during early childhood disturbs the normal development of the auditory system and prohibits the development of speech and language aptitudes [1, 2].
Profound bilateral HL is an uncommon but significant cause of morbidity in the pediatric community. The prevalence rate of hearing loss was estimated from 6 randomly selected governorates, and it was found to be 16% with no significant sex difference. Marsa Matrouh had the highest prevalence in Egypt 25.7%, and North Sinai was the lowest with 13.5%. Children aged from 0 to 4 years had the highest prevalence 22.4%. The commonest cause was found to be otitis media with effusion 30.8% [3]. Without adequate treatment, children fail to develop linguistic abilities and communicative skills, with a significant impact on education, socio-emotional development, and future professional prospects [4].
Several studies have reported positive benefits of pediatric CI on language perception skills, speech intelligibility, and voice monitoring [5, 6]. However, several factors account for the heterogeneity of outcomes. Intrinsic factors such as gender, IQ, socioeconomic status, age of onset of HL, or associated disabilities may predispose children to better or poorer outcomes with the implant. Conversely, extrinsic factors such as age at implantation, educational, and re-educational strategies may play an important role in the variability of several outcomes [7].
In order to prevent these serious impacts of HL on children, they should receive appropriate and adequate auditory rehabilitation including counseling, fitting with proper amplification device either hearing aids or cochlear implant and comprehensive auditory training program imminently [8].
Upon reviewing the literature, some studies were conducted in Egypt in different governorates regarding epidemiology, etiology, and rehabilitation outcome [9,10,11]. Since there were no studies conducted in Alexandria concerned with the outcome of cochlear implanted children. This aroused the need to carry out this study to assess the progress after 2 years of cochlear implantation. The rationale of this study is to better understand the factors that promote spoken language development after CI.
This study aimed at assessing the progress in all aspects of language acquisition and the effect of various factors on the outcome of cochlear implantation in children undergoing auditory training for at least two years after surgery.
Methods
Patients
A retrospective longitudinal study of the pediatric patient database was conducted at the Unit of Phoniatrics, in the outpatient clinic of Alexandria Main University hospital. It was conducted within the period of 6 months starting January 7, 2019. The ethics committee of the Faculty of Medicine, Alexandria University (IRB NO: 00012098, FWA NO: 00018699) approved the study (0,105,978). The recorded data of 33 children were evaluated in this study. All patients suffered from prelingual deafness and had normal mental function with no other comorbidities. Inclusion criteria involved hearing-impaired children of both sexes, who underwent CI for at least 2 years, good audiological profile after CI (normal hearing level or mild hearing loss).
Methods
All study participants were assessed by phoniatricians of at least 3 years’ experience in phoniatrics practice, and the IQ was assessed by expert psychometrists of more than 20 years’ experience at the Unit of Phoniatrics, in the outpatient clinic of Alexandria Main University hospital. All data was obtained from the database of the children records.
Pre-operative
All study participants underwent the following protocol of assessment including the following:
-
A.
Elementary diagnostic procedures
-
History taking including the following:
-
➢ Personal data, parents’ consanguinity, and socio-economic status
-
➢ Age of hearing loss discovery and causative factor (if known)
-
➢ Pre-implant residual hearing
-
➢ Hearing aids (age when it was fitted, laterality, and regularity of hearing aid use)
-
➢ Medical history and relevant pre-natal, peri-natal, and post-natal events
-
-
Audiological evaluation (pure tone audiometry)
-
Lip reading, sound detection, and auditory perceptual assessment (APA) to obtain:
-
➢ Levels of receptive language skills (RLS GM) after Geers and Moog [12, 13]
-
▪ I: Demonstrates awareness that the mouth and/or voice convey information
-
▪ II: Demonstrates comprehension of a few words or expressions
-
▪ III: Demonstrates the ability to learn new words
-
▪ IV: Demonstrates the ability to acquire new comprehension vocabulary in phrases and sentence
-
▪ V: Demonstrates comprehension of successive phrases and sentences
-
-
➢ Levels of expressive language skills (ELS GM) after Geers and Moog [12, 13].
-
▪ I: Demonstrates awareness that vocalizations are used to communicate
-
▪ II: Demonstrates the ability to use a few syllables, words or expressions
-
▪ III: Demonstrates the ability to learn new expressive vocabulary
-
▪ IV: Demonstrates the ability to acquire new expressive vocabulary fairly readily
-
▪ V: Demonstrates the ability to join 2 or 3 words together
-
▪ VI: Demonstrates the ability to combine verbs and nouns in phrases or sentences
-
▪ VII: Demonstrates the ability to use sentences containing a modifying word or phrase
-
▪ VIII: Demonstrates the ability to use sentences containing more than one type of modifying word or phrase
-
▪ IX: Demonstrates the ability to use sentences containing more than one verb form
-
-
➢ Categories of auditory performance (CAP) [14]
-
▪ 0: No awareness of environmental sounds
-
▪ 1: Awareness of environmental sounds
-
▪ 2: Response to speech sounds (e.g., ‘‘go’’)
-
▪ 3: Identification of environmental sounds
-
▪ 4: Discrimination of some speech sounds without lip-reading
-
▪ 5: Understanding of common phrases without lip-reading
-
▪ 6: Understanding of conversation without lip-reading
-
▪ 7: Use of telephone with known listener
-
-
➢ Speech intelligibility rating criteria (SIR) [15]
-
Category 1: Connected speech is unintelligible. Pre-recognizable words in spoken language, primary mode of communication may be manual.
-
Category 2: Connected speech is unintelligible. Intelligible speech is developing in single words when context and lip-reading cues are available.
-
Category 3: Connected speech is intelligible to a listener who concentrates and lip-reads.
-
Category 4: Connected speech is intelligible to a listener who has a little experience of a deaf person’s speech.
-
Category 5: Connected speech is intelligible to all listeners. Child is understood easily in everyday contexts.
-
-
-
Speech and language rehabilitation prior to implantation: (duration and regularity were recorded)
-
-
B.
Clinical diagnostic procedures
-
Formal language testing using the following:
-
❖Test of acquired communication skills (TACS) for children younger than 2 years [16].
-
❖Arabic Language Test (ALT) for children older than 2 years. Assessing receptive language, expressive language, semantics, pragmatics, prosody, and articulation. The child’s score is then compared to the mean of his age group to determine the child’s language age and language defects [17].
-
-
Articulation testing using Arabic articulation test (if it was available in the child’s records) [18]
-
Psychometric evaluation
-
❖Vineland social maturity scale (VSMS) to assess Social quotient [19]
-
❖Stanford Binet Scale 4th edition to assess mental age, verbal intelligence quotient, abstract intelligence quotient, and general intelligence quotient [20]
-
❖Denver Developmental Screening Test (DDST), DENVER II for children less than 2 years [21]
-
-
Operative history
-
➢ Age at the time of implantation
-
➢ Unilateral/bilateral cochlear implant
-
➢ Brand: (Advance Bionics (AB), Cochlear, MED-EL, Oticon)
-
➢ Implant type
-
➢ Site of insertion: (round window, extended round window, Boney cochleostomy)
Postoperative
Post-CI: Children were reassessed using same protocol same as pre-cochlear implantation in addition to the following:
-
Speech and language rehabilitation after implantation: place, duration, regularity, number of sessions, and type of parents’ involvement; active/passive involvement; and their commitment to required tasks.
Data management and statistical analysis
Data were collected, coded, revised, and entered the Statistical Package for Social Science (Rstudio) version 2.3.2. The data were presented as numbers and percentages for the qualitative data, mean, standard deviations, and ranges for the quantitative data with parametric distribution and median with interquartile range (IQR) for the quantitative data with non-parametric distribution. Chi-square test and Fisher’s exact test were used in the comparison between two groups with qualitative data. Paired t test was used in the comparison between paired two groups (before and after) with quantitative data and parametric distribution and Wilcoxon paired test was used in the comparison between two groups with quantitative data and non-parametric distribution. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p value was considered significant if < 0.05.
Results
Descriptive results
The study included 19 (57.6%) males and 14 (42.4%) females. The age of all cases ranged from 3.11 to 13.1 years with a median (IQR) of 8.9 (6.8–10.4) years. The age of hearing loss ranged from 0.0 to 48.0 months with a median (IQR) of 15 (8.0–20.0) months. The etiologies of hearing loss were unknown in 30 patients (90.9%), meningitis in two patients (6.06%), and otitis media in one patient (3.03%). The age of hearing aids fitting ranged from 1.0 to 21.0 months with a median (IQR) of 9.0 (5.0–13.50) months. Twenty patients (60.6%) used binaural hearing aids, 11 patients (33.3%) used a monoaural right hearing aid, and two patients (6.1%) used no hearing aids. The majority of our patients (75.7%) used their hearing aids regularly while 18.2% used them irregularly. Positive parent involvement was reported in 75.8% (25 patients) of all cases.
At the time of the CI operation, the age of the patients ranged between (0.58–7.0) years with a median of 4 (2.5 to 5.0) years. All patients (33) received unilateral implants (right side). The implants brands were MED-EL, cochlear, and Oticon implants which were used in 22 (66.67%) patients, 7 (21.21%) patients, and 4 patients (12.12%), respectively. Boney cochleostomy insertion was performed in 14 patients (42.2%), and round window insertion was conducted in 10 patients (30.3%) while extended round window insertion was carried out in 9 patients (27.3%) as shown in Tables 1 and 2.
Comparative results
-
a.
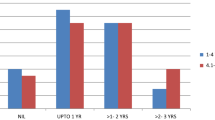
Comparison of Levels of Receptive Language Skills (RLS GM) before and after operation was demonstrated in Fig. 1. The levels of RLS GM before and after the operation were distributed as the following: 15 patients (45.5%) before the operation and one patient (3.03%) after the operation demonstrated comprehension of a few words or expressions, 12 patients (36.4%) before the operation and no patient after the operation demonstrated awareness that the mouth and/or voice convey, 3 patients (9.09%) before the operation and 7 patients (21.2) after the operation demonstrated the ability to learn new words, two patients (6.06%) before the operation and 8 patients (24.2%) after operation demonstrated the ability to acquire new comprehensive vocabulary in phrases and sentences, and one patient (3.03%) before operation and 17 patients (51.5%) after the operation demonstrated comprehension of successive phrases and sentences. There was no statistically significant difference between RLS GM before and after the operation (p = 0.854).
-
b.
Comparison between Levels of Expressive Language Skills (ELS GM) before and after operation illustrated in Fig. 2. The preoperative levels of ELS GM were distributed as the following: 15 (45.5%) patients demonstrated the ability to use a few syllables, words, or expressions; 12 (36.4%) patients demonstrated awareness about the used vocalization to communicate; 3 (9.09%) patients demonstrated the ability to learn new expression; and 33 patients (9.09%) demonstrated the ability to acquire new expressive vocabulary readily.
The postoperative levels of ELS GM were distributed as the following: 8 patients (24.2%) demonstrated the ability to join 2 or 3 words together, 6 patients (18.2%) demonstrated the ability to learn new expressions, 6 patients (18.2%) demonstrated the ability to combine verbs and nouns in phrases or sentence, three patients (9.09%) demonstrated the ability to acquire new expressive vocabulary fairly readily, and two patients (6.06%) demonstrated the ability to use a few syllables, words, or expressions.
There was no statistically significant difference between ELS GM levels before and after the operation (p=0.208).
-
iii.
Comparison of Categories of Auditory Performance (CAP) before and after Operation simplified in Fig. 3. Regarding preoperative CAP, 12 patients (36.4%) responded to speech sound, 6 patients (18.2%) had no awareness to the environmental sounds, 6 patients (18.2%) discriminated some speech sounds without lip-reading, 4 patients (12.1%) were aware of environmental sounds, and 3 patients (9.09%) identified the environmental sounds. Regarding postoperative CAP, 14 patients (42.3%) understood the common phrases without lip-reading, 11 patients (33.3%) understood the conversation without lip-reading, and 7 patients (21.1%) had no awareness of environmental sounds. There was no statistically significant difference between CAP before and after the operation (p = 0.737).
-
iv.
Fig. 4 illustrated the comparison of Speech Intelligibility Rating (SIR) Criteria before and after the operation. Comparison of SIR before and after the operation showed the following, among 27 patients (81.8%) before the operation and no patient after the operation, unintelligible pre-recognizable words in spoken language primary mode of communication was manual, among two patients (6.06%) before the operation and three patients (9.09%) after the operation, unintelligible intelligible speech is developing in single words with context and lip-reading, two patients (6.06%) before operation, and 10 patients (30.3%) after operation were intelligible to the listener who concentrates and lip-reading, two patients (6.06%) patients before operation and 16 patients (48.5%) after the operation were intelligible to a listener who has a little experience of a real person’s speech; finally, no patient before the operation and 4 patients (12.1%) after the operation were intelligible to all listeners and child understood easily in everyday contexts. There was no statistically significant difference between SIR before and after the operation (p = 0.813).
-
v.
The Comparison of Stanford Binet IQ improvement before and after the operation was shown in Table 3. There was a statistically significant difference before and after the operation, as regards language age (years), abstract IQ score, general IQ score, general IQ categories, and audiological profile (p < 0.0001, P = 0.0001, p = 0.006, p = 0.052, and p < 0.0001, respectively).
Analysis of variable results
-
a.
Univariate and multivariate linear regression showed no statistically significant difference as a separate variable or in the presence of all variables of general IQ score (postoperative) and age of hearing loss (months), cause of hearing loss, age of hearing aids (months), duration of hearing deprivation till hearing aids (months), duration of hearing deprivation from hearing loss till CI (years), duration of rehabilitation in years (preoperative), age at time of CI surgery (years), implant brand, site insertion, and parent involvement as shown in Table 4.
-
b.
Univariate and multivariate linear regression showed that there was a statistically significant difference between language age scores and age at the time of CI surgery as a separate variable (p = 0.006) and in the presence of other variables (adjusted p = 0.016). While no statistically significant difference was found between Arabic language test (years) (postoperative) and age of hearing loss (months), cause of hearing loss, age of hearing aids (months), duration of hearing deprivation till hearing aids (months), duration of hearing depravation from hearing loss till CI (years), duration of rehabilitation in years (preoperative), age at time of CI surgery (years), implant brand, site insertion, and parents involvement as shown in Table 5.
-
c.
Univariate and multivariate linear regression showed that there was a statistically significant difference between audiological profile score and age of hearing loss (months), age at time of CI surgery, and site of insertion (round window) as a separate variable (p = 0.017, p = 0.001, p = 0.019, respectively). No statistically significant difference was found between audiological profile score (postoperative) and age of hearing loss (months), cause of hearing loss, age of hearing aids (months), duration of hearing deprivation till hearing aids (months), duration of hearing depravation from hearing loss till CI (years), duration of rehabilitation in years (preoperative), age at time of CI surgery (years), implant brand, site insertion, and parents’ involvement as shown in Table 6.
Discussion
Cochlear implantation (CI) has become the most successful neural prosthesis, for auditory rehabilitation of children with severe to profound SNHL who fail to benefit from conventional amplification. Technological developments in CI systems on which a sequence of speech coding strategies have been implemented seem to have resulted in improved speech perception. Nevertheless, changing selection criteria for implantation have coincided with growing technology and post-CI speech perception advancement. The main goal of a CI is to use electric stimulation to restore functional hearing [22, 23].
This study investigated factors contributing to the comprehension and production of language by children with prelingual SNHL after at least 2 years of CI use. Studying the effect of different factors so that maximum implant benefit could be achieved [24].
The outcome varies in the studied children and depends among others on the age of implantation, residual hearing, mode of communication, and support of family, as well as the quality, regularity, and length of rehabilitation. These factors contribute to speech perception abilities and were found to explain some of the variances in results [25, 26].
The present study of 33 cases consisted of 19 males (57.6%) and 14 (42.4%) females. This is consistent with the findings of Abdel Hamid et al. who reported approximately equal male to female distribution in children with SNHL. However, this is contradictory to earlier studies that showed male predominance in children with sensorineural hearing loss [27].
All cases were deafened under 3 years of age. The age of hearing loss ranged from 0.0 to 48.0 months and were implanted within the range between (0.58–7.0) years at the time with a median of 4 (2.5 to 5.0) years (most under age 5). Although most of the children were reportedly deaf from birth, 30 patients (90.9%). However, 9.09% of them had some known etiology of deafness after birth, meningitis in two patients (6.06%), and otitis media in one patient (3.03%). For the 33 children, the mean age at first hearing aid fit ranged from 1 to 21 months with a median of 9 (5.0–13.50) months [24].
The most common etiology of bilateral SNHL is unknown in agreement with the finding of Sanjay Morzaria et al. who discussed two studies that assessed patients with unknown SNHL prospectively to identify unrecognized causes. Although their methodology was unclear, the authors stated a diagnosis in 44% of unknown cases with prospective evaluation [28].
The timing of HL in all the subjects was pre-lingual; the age of hearing loss ranged from birth to 48 months, and the degree of hearing loss was bilateral severe to profound SNHL ranges from 90 to 110 dB HL in all 33 cases. The pure-tone audiogram results showed significant improvement in hearing at all frequencies after cochlear implantation. The subjects ranged from having normal hearing to having mild hearing loss (20–35 dB HL). This is to be expected because the direct stimulation of the auditory nerve endings at the different sites in the cochlea leads to increased sound perception at all frequencies. This effect is seen in all subjects, unrelated to the brand or model of multichannel CI and site of insertion [29].
The collected data also showed a significant difference between age of hearing loss discovery and degree of hearing level improvement after CI which stresses the importance of early hearing screening.
Children with HL which was diagnosed by 6 months of age with early intervention demonstrated significantly better language and IQ scores than those in whom a hearing loss was identified after 6 months of age. Thus, the current candidacy criteria have been expanded to allow deaf children to access the benefits of CI as early as possible [30].
Regarding their hearing technology, 31 (93.99%) patients used HA, the age of HA fitting ranged from 1 to 21 months while 20 patients (60.6%) used binaural HA, 11 patients (33.3%) used a monoaural right HA, while two patients (6.1%) wore no HA because they underwent CI surgery when they were under 12 months old. Most of our patients (75.7%) used their hearing aids regularly while 18.2% used them irregularly. Positive parent involvement in terms of understanding and commitment to rehabilitation was reported in 75.8% (25 patients) of all cases prior to surgery.
All 33 cases got unilateral right CI afterward, this is consistent with the increased use of CI for hearing restoration for children with severe to profound HL due to earlier diagnosis and preference for earlier implantation these days [31].
Although improved, no statistically significant difference was found in levels of receptive language skills, levels of expressive language skills, CAP or SIR scores of the studied cases when compared before and after CI. This is contradictory to the findings of Bernhard Richter et al. [13]. It might be attributed to the small number of cases included in this study.
When comparing between pre- and post-CI a statistically significant increase in the abstract IQ and General IQ scores of the cases was found. Moreover, a statistically significant increase in the scores of the total language age in all cases was found when the mean difference of the scores of the TACS and Arabic language test was compared before and after the operation.
The presented data are consistent with the pediatric literature, demonstrating that children gain significant improvement in speech perception, auditory skills as well as receptive and expressive language following implantation [11, 32].
The improvement in the scores was enough to detect an overall significant improvement in the total language age. With different magnitude of progress, while this might be attributed to the scoring system of the Arabic language test, in which each subtest score is converted into an equivalent language age with a 6-month interval between the equivalent ages. It is mainly due to the multivariate dependent variable nature of this study that makes each case has its own distinctive outcome.
Additionally, these results confirm the role of CI in the progress of language acquisition leading to an increase in the verbal intelligence scores with no statistically significant difference found. This was confirmed by the improvement detected in the language skills of the cases.
The collected data show that language development and verbal intelligence develop faster in the younger age, and this might be due to an increase in the level of neural auditory plasticity in the first 6 years of life with maximum plasticity up to the first 4 years of life resulting in faster linguistic acquisition [33].
There was a statistically significant difference between language age scores and age at the time of CI. Results from this study suggest that early implantation is associated with rate increases in the acquisition of language. These findings emphasize the need to develop objective tools to monitor the benefit of amplification in developing language acquisition and guide timely intervention with CI [32].
So, the sooner children with hearing loss received their cochlear implant, the better their language outcome. this statement is in agreement with other recent studies which reported that the age of implantation ranged from 6 to 48 months due to the concept of a sensitive period [34].
It is contributed to the neural maturation processes of the auditory pathway, the active part of which starts in the first few months of life (after around 6.5 months) with what is termed canonical babbling. Clinical studies showed that artificial electrical stimulation results in inadequate maturation of the auditory pathway. Investigations into the cortical maturation of congenitally deaf children who underwent prelingual cochlear implantation revealed both physiologically normal maturation characteristics and characteristics that differed from the physiology of normal-hearing people [35, 36].
This is contrary to what was reported by Geers et al. who stated that receiving an implant at 2 years of age was not of any significance in regard to linguistic gain over receiving it at 5 years of age [24]. While it is in agreement with the findings of Kirk et al. [37] and Lee-Suk Kim et al. [38] who reported a significant advantage for children getting implanted under 2 years compared with 3 to 4 years of age.
This study included a follow-up of a few early implanted children suggests that age at implantation determines expressive language development, auditory skills, speech understanding, and oral linguistic development. Therefore, young age at implantation is an important determining factor of outcome as demonstrated in Tables 3 and 4 [39].
It also stated that early implantation age (under 2 years) makes a significant improvement in the degree of hearing level postoperative in comparison to older aged children furthermore in regard of surgical data we found that the round window technique for cochlear implant electrode insertion gives better results as well, in agreement of the finding of Leong et al. who concluded that the round window approach is a practical choice in CI surgery since it permits an angle of insertion that minimizes intracochlear trauma so insertion of the electrode array through the round window allows for most anatomical variations in cochlear size and orientation to maximize full and accurate electrode array placement in the scala tympani, a feature generally considered to be associated with improved auditory outcomes [40].
Limitations of the study
It had to be mentioned that unfortunately, the number of subjects was relatively small as collecting data was confined to a short period of time; and thus, statistical evaluation was difficult. Consequently, this study only sheds light on the performance of a relatively small number of cochlear implanted children at a given time. Longer longitudinal prospective larger-scale multi-centric studies are needed to adequately assess their progress and the outcomes during the first few years post-implantation.
Conclusion
CI children showed significant improvement in speech perception, auditory skills, and IQ scores as well as receptive and expressive language after CI denoted by the improvement of language age. Significant improvement was found in early implantation age (under 2 years) in the postoperative degree of hearing level and in language test scores in comparison to older aged children.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Thabet MT, Said NM (2012) Cortical auditory evoked potential (P1): a potential objective indicator for auditory rehabilitation outcome. Int J Pediatr Otorhinolaryngol 76(12):1712–1718. https://doi.org/10.1016/j.ijporl.2012.08.007
Gordon KA, Papsin BC, Harrison RV (2006) An evoked potential study of the developmental time course of the auditory nerve and brainstem in children using cochlear implants. Audiol Neurootol 11(1):7–23. https://doi.org/10.1159/000088851
Abdel-Hamid O, Khatib OM, Aly A, Morad M, Kamel S (2007) Prevalence and patterns of hearing impairment in Egypt: a national household survey. East Mediterr Health J 13:1170–1180
Owens D, Espeso A, Hayes J, Williams R (2006) Cochlear implants: referral, selection and rehabilitation. Curr Paediatr 16(5):360–365
Bruijnzeel H, Ziylan F, Stegeman I, Topsakal V, Grolman W (2016) A systematic review to define the speech and language benefit of early (<12 months) pediatric cochlear implantation. Audiol Neurootol 21(2):113–126. https://doi.org/10.1159/000443363
Cejas I, Hoffman MF, Quittner AL (2015) Outcomes and benefits of pediatric cochlear implantation in children with additional disabilities: a review and report of family influences on outcomes. Pediatric Health Med Ther 6:45–63. https://doi.org/10.2147/phmt.S65797
Roman S, Rochette F, Triglia JM, Schön D, Bigand E (2016) Auditory training improves auditory performance in cochlear implanted children. Hear Res 337:89–95. https://doi.org/10.1016/j.heares.2016.05.003
Apuzzo ML, Yoshinaga-Itano C (1995) Early Identification of Infants with Significant Hearing Loss and the Minnesota Child Development Inventory. Seminars in Hearing 16:124–135
Taha AA, Pratt SR, Farahat TM, Abdel-Rasoul GM, Albtanony MA, Elrashiedy A-LE et al (2010) Primary-school children in Shebin El-Kom District. Egypt Am J Audiol 19:46–60
Elbeltagy R, Bakry HM, Waly EH (2019) Hearing loss-related knowledge and attitude toward neonatal hearing screening among Egyptian parents. Egypt J Otolaryngol 35(2):207–212
Hamid AA, Elshazly M, Eldessouky T et al (2015) Predictors of language and auditory skills in Egyptian children with a cochlear implant. Egypt J Otolaryngol 31:170–175. https://doi.org/10.4103/1012-5574.161605
Moog JS, Popelka GR, Geers AE, Russo MH (1990) Early speech perception test for profoundly hearing-impaired children. Central Institute for the Deaf, St. Louis, Mo
Richter B, Eissele S, Laszig R, Löhle E (2002) Receptive and expressive language skills of 106 children with a minimum of 2 years’ experience in hearing with a cochlear implant. Int J Pediatr Otorhinolaryngol 64(2):111–125. https://doi.org/10.1016/s0165-5876(02)00037-x
Archbold S, Lutman ME, Marshall DH (1995) Categories of auditory performance. Ann Otol Rhinol Laryngol Suppl 166:312–314
Cox RM, McDaniel DM (1989) Development of the Speech Intelligibility Rating (SIR) test for hearing aid comparisons. J Speech Hear Res 32(2):347–352. https://doi.org/10.1044/jshr.3202.347
Elhakeem ES (2013) Formulation of an Arabic test for evaluating acquired skills in communication. 29th world congress of IALP proceeding. Torino, Italy; 28–29 August 2013
Rifaie N, Hamza TM, Elfiky YH (2021) Validity and reliability of the revised Arabic language test for 2–4-year-old children: cross-sectional study. Egypt J Otolaryngol 37:26. https://doi.org/10.1186/s43163-021-00088-8
Kotby MN, Bassiouny S, EL-Zomor M, Mohsen E (1986) Standard isolation of an 295 articulation test. Proceedings of the 9th annual Ain Shams medical congress 915. 296 11
Sparrow SS, Balla DA, Cicchetti DV (1984) Vineland adaptive behavior scales: Interview edition, survey form manual. Circle Pines: American Guidance Service
(1988) Stanford-Binet scale fourth image. Quoted and prepared by Dr. Louis Kamel Malika, second edition. Victor Kyrollos Press
Frankenburg WK, Dodds JB (1967) The Denver developmental screening test. J Pediatr 71(2):181–191. https://doi.org/10.1016/s0022-3476(67)80070-2
Carlson ML, Sladen DP, Haynes DS, Driscoll CL, DeJong MD, Erickson HC et al (2015) Evidence for the expansion of pediatric cochlear implant candidacy. Otol Neurotol 36(1):43–50. https://doi.org/10.1097/mao.0000000000000607
David EE, Ostroff JM, Shipp D, Nedzelski JM, Chen JM, Parnes LS et al (2003) Speech coding strategies and revised cochlear implant candidacy: an analysis of post-implant performance. Otol Neurotol 24(2):228–233. https://doi.org/10.1097/00129492-200303000-00017
Geers AE, Nicholas JG, Sedey AL (2003) Language skills of children with early cochlear implantation. Ear Hear 24(1 Suppl):46S-58S. https://doi.org/10.1097/01.AUD.0000051689.57380.1B
Janeschik S, Teschendorf M, Bagus H, Arweiler-Harbeck D (2013) Influence of etiologic factors on speech perception of cochlear-implanted children. Cochlear Implants Int 14(4):190–199. https://doi.org/10.1179/1754762812y.0000000017
Francis HW, Pulsifer MB, Chinnici J, Nutt R, Venick HS, Yeagle JD et al (2004) Effects of central nervous system residua on cochlear implant results in children deafened by meningitis. Arch Otolaryngol Head Neck Surg 130(5):604–611. https://doi.org/10.1001/archotol.130.5.604
Abdel-Hamid O, Khatib OM, Aly A, Morad M, Kamel S (2007) Prevalence and patterns of hearing impairment in Egypt: a national household survey. East Mediterr Health J 13(5):1170–1180. https://doi.org/10.26719/2007.13.5.1170
Morzaria S, Westerberg BD, Kozak FK (2004) Systematic review of the etiology of bilateral sensorineural hearing loss in children. Int J Pediatr Otorhinolaryngol 68(9):1193–1198. https://doi.org/10.1016/j.ijporl.2004.04.013
Wei WI, Wong R, Hui Y, Au DK, Wong BY, Ho WK et al (2000) Chinese tonal language rehabilitation following cochlear implantation in children. Acta Otolaryngol 120(2):218–221. https://doi.org/10.1080/000164800750000955
Kwak MY, Lee JY, Kim Y, Seo JW, Lee JY, Kang WS et al (2020) Long-term change in the speech perception ability in pediatric cochlear implants and the effect of the age at implantation. Otol Neurotol 41(6):758–766. https://doi.org/10.1097/mao.0000000000002640
Van Wieringen A, Wouters J (2015) What can we expect of normally-developing children implanted at a young age with respect to their auditory, linguistic and cognitive skills? Hear Res 322:171–179. https://doi.org/10.1016/j.heares.2014.09.002
Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL et al (2010) Spoken language development in children following cochlear implantation. JAMA 303(15):1498–1506. https://doi.org/10.1001/jama.2010.451
Lee KY, Van Hasselt CA, Tong MC (2010) Age sensitivity in the acquisition of lexical tone production: evidence from children with profound congenital hearing impairment after cochlear implantation. Ann Otol Rhinol Laryngol 119(4):258–265. https://doi.org/10.1177/000348941011900409
Shahin E, El Shennawy A, Sheikhany A, El Tahawy A (2019) The influence of early versus late cochlear implantation on the language outcomes of egyptian arabic speaking children with congenital bilateral severe-profound sensory-neural hearing loss. EJENTAS 20(1):16–22
Lesinski-Schiedat A, Illg A, Heermann R, Bertram B, Lenarz T (2004) Paediatric cochlear implantation in the first and in the second year of life: a comparative study. Cochlear Implants Int 5(4):146–159. https://doi.org/10.1179/cim.2004.5.4.146
Moore JA, Bass-Ringdahl S (2002) Role of infant vocal development in candidacy for and efficacy of cochlear implantation. Ann Otol Rhinol Laryngol Suppl 189:52–55. https://doi.org/10.1177/00034894021110s511
Kirk KI, Miyamoto RT, Lento CL, Ying E, O’Neill T, Fears B (2002) Effects of age at implantation in young children. Ann Otol Rhinol Laryngol Suppl 189:69–73. https://doi.org/10.1177/00034894021110s515
Kim LS, Jeong SW, Lee YM, Kim JS (2010) Cochlear implantation in children. Auris Nasus Larynx 37(1):6–17. https://doi.org/10.1016/j.anl.2009.09.011
May-Mederake B (2012) Early intervention and assessment of speech and language development in young children with cochlear implants. Int J Pediatr Otorhinolaryngol 76(7):939–946. https://doi.org/10.1016/j.ijporl.2012.02.051
Leong AC, Jiang D, Agger A, Fitzgerald-O’Connor A (2013) Evaluation of round window accessibility to cochlear implant insertion. Eur Arch Otorhinolaryngol 270(4):1237–1242. https://doi.org/10.1007/s00405-012-2106-4
Acknowledgements
The research team would like to thank the other colleagues in the department. Also deep thank to the participants in the research and our colleagues.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EE: supervision, established the concept of the research, designed the work, validation, and visualization of the results. RM: role in supervision, role in revising the results, writing the original draft, reviewing, and editing. HE: role in collecting data, analyzing the data. FA: role in the concept of research, methodology design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of the Faculty of Medicine, Alexandria University (IRB NO: 00012098, FWA NO: 00018699), approved the study (no 0105978). Informed written consent to participate in the study was provided by parents or legal guardians of all participating children.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elhakeem, E.S., Elmaghraby, R.M., Elroumy, H.M.G.E. et al. Evaluation of outcome of cochlear implanted children after 2 years of rehabilitation in Alexandria: a retrospective study. Egypt J Otolaryngol 39, 42 (2023). https://doi.org/10.1186/s43163-023-00403-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00403-5