Abstract
Recently, allergic rhinitis (AR) cases have been surging rapidly in many developing countries. However, the prevalence, risk factors and treatment modalities for AR within the Malaysian population have not been thoroughly evaluated. The present study aimed to provide a complete review of literature on allergic rhinitis in Malaysia. Available data indicated that the prevalence of AR varied across different age groups and regions in Malaysia, but there is an increasing trend among the younger population. The key contributing factor is exposure and sensitization towards several airborne allergens, mainly house dust mites, cat fur and fungi, with possible genetic predispositions. In addition, variations in the symptom severity may be associated with racial orientations. For management of the disease, standard prescriptions of conventional drugs (antihistamines, intranasal corticosteroids and nasal decongestants) remain as the treatment of choice. A small proportion of the native residents tend to resort to alternative approaches of self-healing through aromatherapy and natural food consumption such as tiger’s milk mushroom and Tualang honey. In conclusion, the increase in the cases of AR in Malaysia is due to environmental and genetic factors which requires proper medical intervention as treatment strategies. The utilization of holistic approaches requires further studies and clear understanding prior to their integration into the standard of care. There are still many gaps in the knowledge and management of allergic rhinitis which demands further attention from the research community.
Similar content being viewed by others
Background
Allergic rhinitis (AR), a type 1 hypersensitivity disorder, causes inflammation of the upper nasal cavity due to inappropriate immunologic reactions against harmless agents [1]. The cardinal symptoms of AR are sneezing, rhinorrhoea, nasal itchiness and congestion [2], sometimes accompanied with itchy and watery eyes [3,4,5]. Apart from the clinical burden, other implications of AR include sleep deprivation, absenteeism from school/work and lack of productivity [6, 7]. In 2018 alone, about US $30.7 to 105.4 billion were spent on treating AR within Asia-Pacific [6]. These reports insinuated that allergic rhinitis is a vexing form of allergy with multiple adverse repercussions. The global prevalence of AR stands at 15–25%, with children and adolescents more prone to this condition than adults [8]. Lately, significant rises in the disease epidemiology rates were noted in many countries [9,10,11]. In Malaysia, several studies were performed to assess the disease burden [4, 5, 12], but changes in the incidence rates of allergic rhinitis through the years within this population have not been clearly elucidated.
The Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines have highlighted indoor (house dust mites, cockroaches, and animal dander) and outdoor (pollens and moulds) allergens as two of the most prominent causes of AR [13]. Nonetheless, other predisposing factors including family history of allergies and the presence of concurrent asthma and/or eczema may also be instrumental [14]. For the Malaysian scene, though there is a cornucopia of research carried out on the context of allergen sensitization for years, studies assessing the aetiologies of AR are still lacking. Usually, conventional medications are recommended as treatment option, but these are mainly for mitigation of symptom severities only. In this regard, the consumption of natural food sources such as honey, tiger’s milk mushroom and Kecubung fruit, as employed by the local Malay population to counteract the effects of allergic rhinitis, are exceedingly unique yet disputable [15,16,17]. In spite of that, the potential therapeutic benefits of such treatments cannot be cast aside entirely and warrants further investigation.
Allergies have significant socioeconomic impacts on the lives of the sufferers; therefore, a good knowledge, attitude and practice towards AR is needed for long-term disease prevention. Unfortunately, a lack of awareness and understanding of allergic diseases among Malaysians has led to poor choice of treatment strategies [18], which caused improper management of symptoms and brought unnecessary costs to the patients. In this case, a thorough assessment of the situation of AR in Malaysia based on existing knowledge and practices is highly essential for resolution of this disease. With that, the current study attempts to describe the trend in the prevalence of AR in Malaysia and to identify causative agents responsible for AR in this population. In addition, we have also reviewed different types of treatment options available for AR in Malaysia. The final objective of this study is to identify gaps in the literature on allergic rhinitis-related studies in Malaysia and make relevant suggestions for future research opportunities.
The data for this review was collected from previously published literatures in the PubMed and Scopus databases. The following keywords were used to filter and extract relevant research articles: allergic rhinitis, hay fever, prevalence, epidemiology, causes, aetiology, treatment, therapy, Malaysia. The resulting papers were classified into three major subcategories: prevalence, aetiology (environmental and genetic factors) and treatment options (standard and traditional medications). For each of those categories, any or all information pertaining to AR in Malaysia were summarized, compiled and presented in the form of either figures or tables. As a mean to provide additional perspective to the subject matter, this paper has also included reviews of related international studies conducted primarily in the Asia-Pacific region. Discussion based on studies of other respiratory disorders such as asthma and atopic dermatitis was kept to a bare minimum unless deemed necessary, depending on the context of the topic. This is an initial comprehensive study dedicated to compile, analyse and present information on the prevalence, causes and treatments of allergic rhinitis in Malaysia.
Prevalence of allergic rhinitis in Malaysia
According to a multi-national survey by Katelaris et al. (2011), approximately 8.7% of the population across the Asia-Pacific region suffered from allergic rhinitis [19]. In that same survey, the prevalence rate of AR for Malaysia was estimated to be 7.1%, which was higher than other Southeast Asian countries such as Hong Kong, the Philippines and Singapore [19, 20].
Prevalence of allergic rhinitis in children
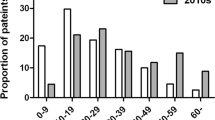
To date, many studies have reported on the prevalence of respiratory-related diseases in various regions (Fig. 1) throughout Malaysia. An earlier Southeast Asian population-based study evaluating the status of respiratory diseases among secondary school students in East Malaysia had established the prevalence of AR of 11.2% [3]. Another questionnaire-based survey administered to secondary school children from the East Coast showed the prevalence of AR at 11.0% and 14.8% in 1995 and 2001, respectively [4]. In 2016, the prevalence of AR was at 18.8% as presented by a survey involving 462 students from 8 secondary schools within the southern region of Peninsular Malaysia [5]. As of 2020, approximately 31.7% and 55.5% of junior high school students from the East Coast and central regions of Malaysia, respectively, had symptoms of AR [12, 21]. Direct comparison of epidemiologic rates from these studies indicates that the prevalence of AR has increased markedly over the years among secondary school children in Malaysia (Fig. 2). In one primary school in the central area, about 11.2% of the students aged between 7 and 12 years old were reported to have current rhinitis [22], whereas in the East Coast, a slight increase (+0.4%) in the occurrence of AR among primary school children was seen between 1995 and 2001 [4]. The International Study of Asthma and Allergies in Childhood (ISAAC) observed small increases in the incidence of AR among children (6 to 7 years old) and young teenagers (13 to 14 years old) in all of these regions (northern, central, East Coast and southern) between 1994 and 2002 (Table 1). During this same timeframe, a decrease in the prevalence rate of allergic rhinitis was only seen among teenagers from the northern region of Peninsular Malaysia (Table 1).
Prevalence of allergic rhinitis in young adults
In a cross-sectional study by Kumar et al. (2020), the prevalence of AR among 1000 higher education students (18 to 26 years old) was at 79.5%. Of this group, only 12.5% exhibited symptoms of AR since childhood [24]. There are, however, no other prevalence studies available for this age group in Malaysia.
Prevalence of allergic rhinitis in adults
For the Malaysian adult population, Lim et al. (2015) estimated the prevalence of AR to be about 53.0% [25]. The findings of this study were limited to office workers from a random tertiary education centre in the central region of Peninsular Malaysia only and were not indicative of the population at large due to differences in occupational backgrounds, age groups, racial profiles and gender. Under these circumstances, it would be of great benefit to have more AR epidemiological studies performed systematically at nationwide scales to obtain a better representation of the general Malaysian population.
Environmental agents associated with allergic rhinitis in Malaysia
House dust mites
Studies from the Middle East, Europe and Southeast Asia emphasized that allergic sensitization to house dust mites contributes tremendously towards allergic rhinitis development [26,27,28], and Malaysia is of no exception [25]. Previously, Mariana et al. (2000) showed that Malaysian households were heavily infested with house dust mites [29] These mites survive and reproduce more readily in tropical weather countries, owing to the favourable environmental temperatures and humidity levels that facilitate their growth and developmental cycles [30]. This explains their relative abundance within the local communities, particularly in the urban and suburban areas [29]. Three of the most common species of dust mites that can trigger significant reactivities among Malaysians are Dermatophagoides pteronyssinus (European house dust mite), Dermatophagoides farinae (American house dust mite) and Blomia tropicalis (Table 2). Yadav et al. (2015) made an interesting observation in their cross-sectional study of AR, whereby children aged between 2 and 10 years old had significantly higher sensitization rates towards D. pteronyssinus and B. tropicalis than infants younger than 2 years old [39] (Table 2). This implies that exposure to risk factors begins during early childhood stages, and this sensitization process persists and develops rapidly into the later years. As such, longitudinal studies are necessary to investigate the impacts of childhood allergen introduction on the occurrence of allergic rhinitis.
Cat fur
Certain types of mammalian-derived allergens including fur, dander (skin flakes), feather and saliva from domesticated pets and farm animals might trigger allergic rhinitis [41]. According to Pang et al. (2017), most Asian AR patients were sensitized towards airborne allergens from cats (19.0%) and dogs (32.0%) [42]. This agrees with the findings of Yadav and Naidu (2013) that children with AR were more likely to own pets at their homes [43]. Data from several studies assert that cat allergy is the second most important AR inducing factor after common dust mites in Malaysia [31, 34, 35], with an estimated prevalence of 25.4% among urban office workers [25]. Cats secrete an allergenic glycoprotein, Fel d 1, from sebaceous gland under their skin and fur which can stimulate Th2-driven hypersensitivities in humans upon inhalation/ingestion [44]. This allergen usually resides on upholstered furniture in homes with cat ownership; nonetheless, it can also be found in considerable amounts on car seats and school floors [45]. Norbäck et al. (2016) showed that the Fel d 1 allergen was consistently present in settled dust samples collected from classrooms of selected schools in the southern region of Malaysia [5]. Further studies relating varying concentrations of Fel d 1 at different sampling sites are needed as they may shed some light on deciphering the threshold level required for initiation of allergen-specific sensitization.
Fungi
Fungi are another typically implicated airborne immunogen after dust mites and animal dander [8]. Recent research had established significant positive association between levels of total fungal DNA in settled dust and rhinitis symptoms among Malaysian students [5]. Furthermore, Fu et al. (2020) demonstrated that fungal richness in school classrooms was positively correlated with allergic rhinitis [21]. Early childhood exposure to high concentrations of fungal allergens may lead to sensitization, and this depends heavily on the age of first contact as well as the strain involved [46]. In Thailand, the three main species of fungi that caused positive reactions among rhinitis patients were Cladosporium sp., Penicillium sp. and Aspergillus sp [47]. Interestingly, a different pattern of sensitization was seen among Malaysian subjects, with the prevalence of 23.5%, 21.2% and 18.8% for Fusarium sp., Aspergillus flavum and Dreselera orysae, respectively [48]. In addition, Kttafah et al. (2020) observed the greatest number of positive responses towards Aspergillus fumigatus in their study of fungal sensitization among Malaysian atopic populations [40]. This disparity in sensitization between Thailand and Malaysia might be due to variations in the fungal spore distribution in both countries, which in turn are strongly affected by climatic parameters such as rainfall and humidity levels [47]. In this case, multicentre birth cohort studies might be useful in understanding the correlation that exist between fungi strain, meteorological conditions and allergic rhinitis predisposition.
Bacteria and associated biomarkers
Indoor microbiome exposure may exert some influence on the occurrence of allergic rhinitis in Malaysia. According to Fu et al. (2020), Gammaproteobacteria, Cyanobacteria and Deinococci, among a few others, were some of the most abundant classes of bacteria found within school classrooms in the East Coast of Malaysia [21]. The richness in the class, Gammaproteobacteria, was significantly, protectively associated with AR, while Aeromonas enteropelogenes, Escherichia fergusonii and Brasilonema bromeliae were negatively associated with AR. On the contrary, Deinococcus grandis was positively correlated with AR [21]. This could mean that exposure to certain types of bacteria may lead to either predisposition or protection against AR. However, due to limitation of studies in this area, the exact role of microorganisms in the pathogenesis of AR remains to be seen.
In some cases, chemical microbial markers may also contribute towards development of rhinitis symptoms. Norbäck et al. (2016) showcased that exposure to endotoxins with C14 3-hydroxy fatty acid (3-OH FA) group was positively correlated with the incidence of AR among Malaysian high school students [49]. Endotoxins or lipopolysaccharides (LPS) are biochemical structures that form part of the outer surface of the cell membrane of a gram-negative bacterium, which upon its lysis can trigger potent activation of the immune system [50]. Braga et al. (2004) demonstrated that simultaneous inhalation of lipopolysaccharides and D. pteronyssinus allergen extract can greatly intensify the nasal allergic reactions as opposed to that of single antigenic challenges alone [51]. Moreover, elevated levels of lipopolysaccharides in the environment were linked with higher occurrence of AR [52]. These findings support the idea that bacterial-derived biomarkers can act as mediators in the pathomechanism of allergic disorders. Future assessment should focus more on investigating the interrelationship between endotoxin polymorphisms and their associated effects on allergic rhinitis manifestation.
Genetic predisposition of allergic rhinitis in Malaysia
Over the past three decades, various studies have suggested noteworthy correlations between specific determinants such as stress levels, family income and daily computer usage time with the epidemiology of AR throughout Asia [20]. One of the most important risk factor that is strongly linked with AR predisposition is an individual’s genetic makeup. Genome-wide association studies (GWAS) and next-generation sequencing techniques have allowed for precise locating of genes susceptible for allergic disorders [53]. A recently conducted meta-analysis in a European population had pinpointed several major histocompatibility complex (MHC) genes that can confer high susceptibility to allergic rhinitis which include HLA-B, HLA-DQA1, HLA-DQA2 and HLA-DRB1 [54]. In a review by Spinola (2017), the linkage between human leukocyte antigen (HLA) genes and AR seemed to vary depending on the effect of the gene (protective or predisposing), population under study and type of allergen sensitization [55]. For instance, HLA-DQB1*06:01:01 and HLA-DRB1*08:03:02 were considered as risk alleles for HDM-sensitized AR, whereas HLA-DQB1*05 conferred protection in a Chinese Han ethnic group [56]. Likewise, alleles HLA-DPB1*05:01 and HLA-DPB1*02 conveyed susceptible and protective roles, respectively, among Japanese rhinitis subjects with cedar pollinosis and sensitization [57].
The distribution of HLA class I and II allelomorphs in Malaysia varies considerably across different racial groups and aboriginal tribes. Malaysia is comprised of three major ethnic groups, namely Malays, Chinese and Indians. The Malays shared many HLA alleles, especially A*24, B*15, Cw*04, Cw*07, DQB1*03, DQB1*05, DRB1*12 and DRB1*15, with other Malay sub-ethnic groups such as Banjar, Bugis, Jawa, Kelantan and Rawa (Table 3). Several of those variants were also prevalent among indigenous groups from East Malaysia; however, alleles A*11, B*18, DRB1*09 and DRB1*16 were more common within this population than in the Malays (Table 4). The Malaysian Chinese differed from the Malays in terms of alleles B*40:01, C*01:02, DQB1*03:03 and DRB1*09 (Table 4). Due to a lack of studies, comparison of HLA alleles for the Malaysian Indian population was not conducted in this review. Some of these HLA class I and II polymorphs were significantly linked with autoimmune and malignant disorders in Malaysia including systemic lupus erythematosus [68,69,70], rheumatoid arthritis [71], aplastic anaemia [72], and leukaemia [73]. Apart from that, two local studies had independently demonstrated a strong association between HLA-B*15:02 allele and drug-induced (carbamazepine) hypersensitive reactions in patients and healthy controls, irrespective of their ancestries [74, 75]. However, studies on the interrelation between HLA markers and allergic predisposition in Malaysia are still lacking.
Besides the HLA genes, studies by Ramasamy et al. (2011) and Bønnelykke et al. (2013) indicated that certain loci harbouring genes such as C11ORF30/EMSY, IL2, STAT6 and TMEM232 contained different forms of intergenic single-nucleotide polymorphisms (SNPs) that significantly increased the risk of developing AR through allergen-specific sensitizations [76, 77]. Andiappan et al. (2011) had reported two novel SNPs in MRPL4 and BCAP gene loci, respectively, which might act as risk candidates for rhinitis among Singaporean Chinese population [78]. Within Chinese Han community, AR risk variants were seen near EMSY-LRRC32 locus, whereas a protective genotype was found at IL4 region [79]. In Japan, two variants in IL-1B genomic stretch were determined to be associated with cedar and cypress allergy [80]. Similarly, a Malaysian pilot study by Yadav et al. (2013) established a significant relationship between a variant of IL-13 gene (IL-13 R130Q) and allergic rhinitis development [81], thereby affirming that SNPs play a huge role in the pathomechanism of allergic diseases. The potential role of these genes should be further confirmed via mechanistic studies and validated on a larger population size.
Ethnicity and allergic rhinitis
The latest version of the ARIA guidelines has classified AR based on duration (intermittent or persistent) and symptom severity (mild or moderate-severe) [13]. The degrees of AR symptoms intensity are predominantly controlled by circulating allergen-specific IgE levels [82], polysensitization status [83, 84], duration of allergy and the presence of comorbidities [85]. In some inflammatory disorders (SLE and ankylosing spondylitis), significant differences in the disease chronicity were noticed within the population when racial and ethnic backgrounds were factored in [86, 87]. This leads to the hypothesis that ethnicity can trigger variations in the symptom severities. Although the prevalence of allergic rhinitis among the Malays was lower than the non-Malays [43], Amini et al. (2016) inferred that the Malays were more likely to suffer from the most severe symptoms of AR [88]. On the contrary, the Chinese and Indians mainly experienced mild to moderate effects. The same study also supported the notion that elevation in disease severity among the Chinese and Indians depended more on the periods of concomitant allergic diseases, such as atopic dermatitis and asthma, rather than the duration of AR alone. The Indians, in particular, exhibited a positive association between polysensitivities and AR severity [88]. These results imply that ethnicity contributes towards exacerbation of nasal symptoms in relation to rhinitis. Future directions would be to study the involvement of other relevant variables such as genetic background and socioeconomic status, on the symptom severity between different races.
Management and treatment of allergic rhinitis in Malaysia
Two distinct modalities that are currently in practice are prevention of allergen contact and treatment with medical therapies [89].
Preventive self-care practices
In a review of house dust mites (HDM) in Malaysia by Nadchatram (2005), carpets and mattresses were listed as the primary habitats of B. tropicalis and D. pteronyssinus. Routine washing and high-temperature drying of clothes, bed sheets, pillowcases and carpets were essential in maintaining low levels of HDM and its associated allergens at homes [30]. For animal-based allergies, avoiding exposure to furry pets and its surroundings was highly advised [89]. In addition, the Malaysian Allergy Prevention (MAP) guidelines suggested that patients with allergic disorders may benefit from elimination/removal of HDM and pets; however, persons subjected to pets during early infancy may not be at risk for developing allergy [90].
Conventional treatment
Some of the most typically administered conventional drugs for treatment of allergic rhinitis in Malaysia are anti-histamines (e.g. cetirizine, chlorpheniramine, desloratadine and loratadine), intranasal corticosteroids (e.g. budesonide, fluticasone furoate and mometasone) and nasal decongestants (e.g. oxymetazoline) [91]. Loratadine and cetirizine were two of the most preferred choice of anti-histamines for AR management in several Southeast Asian countries [92]. Azelastine nasal spray is another typically prescribed anti-histamine with demonstrated excellence in its safety and efficacy profiles [93]. On the other hand, mometasone furoate and fluticasone furoate nasal sprays displayed equal efficacies as monotherapy for allergic rhinoconjunctivitis, as demonstrated by Aneeza et al. (2013) in a Malaysian population [94]. Additionally, Goh et al. (2014) showed that montelukast in combination with fluticasone propionate (nasal spray) helped to mitigate nasal-ocular symptoms and significantly improve the quality of life in a cohort of Malaysian patients with moderate to severe allergic rhinitis [95].
The ARIA guidelines suggested that the choice of treatment (monotherapy and/or combinatorial) for any group of patients must take into account several factors such as their ages, comorbidities, type of rhinitis (perennial or seasonal) and severity of symptoms [13]. These approaches, however, were mostly based on low certainties of experimental/clinical evidence and should be viewed as conditional recommendations only [13]. Even though the ARIA guidelines have been continuously revised and updated over the years, there exist a wide disparity in its perception and implementation at the primary care level. A recent survey of Malaysian physicians found that only 66.0% of general practitioners and medical officers were aware of the ARIA guidelines [96]. This is considerably lower than that seen in a previous cross-sectional study, which reported that 80.8% of general practitioners from four ASEAN countries (Thailand, Indonesia, Philippines and Malaysia) were well-informed of the ARIA guidelines [92]. In fact, only 58.0% of pharmacists and 66.0% of ENT specialists from Malaysia were satisfied with the suggestions outlined by ARIA, as reported by Prepageran et al. (2014) [97].
The diagnosis of allergic rhinitis in Malaysia is predominantly based on assessments of clinical history, followed by anterior rhinoscopy. Other practices such as allergy testing, imaging paranasal sinuses and nasal endoscopy are less commonly used [96]. Some of the preferred methods of allergy testing include skin prick test, skin patch test and blood serum analysis for total/specific IgE and eosinophil count [96]. Most Malaysian primary care physicians prioritized prescription of first- and second-generation oral anti-histamines and combination of oral anti-histamines with nasal decongestants for treatment of AR [96]. Similar choices were also favoured by most general practitioners and pharmacists from Indonesia, Philippines and Thailand [92]. For the treatment of mild AR, most Malaysian medical professionals preferred prescriptions of anti-histamines for a duration of less than 2 weeks, whereas a combination therapy of anti-histamines with intranasal steroids for more than 3 months was highly favoured by most local ENT specialists for moderate-severe cases of AR [97]. They also believed that efficacy is the most important criterion for selection of anti-histamine drugs. However, most general practitioners and ENT specialists were against increasing the doses of anti-histamines in the event of poor patient prognosis [97]. The ARIA guidelines, though greatly beneficial, lack some pertinent information on the use of anti-histamines, such as its maximum duration of treatment and acceptable levels of dosage increments for patients who are not responding favourably. As such, Abdullah et al. (2019) recommended patient profiling, on the basis of their age, gender and occupation, as a formal guide for prescription of anti-histamines in Malaysia, with follow-up actions taken to closely monitor patient responses thereafter [98].
Allergen immunotherapy
Immune-based therapies for specific allergens have shown promising results in averting the symptoms of allergic rhinitis [99]. In a single blind, randomized placebo-controlled trial, HDM-sensitized Chinese AR patients showed significant reductions in their mite sensitivities after oral consumption of encapsulated D. farinae allergen extract [100]. Fujisawa et al. (2018) also emphasized that subcutaneous injection of allergen mixture solution at appropriate doses provided long-term safety and efficacy among Japanese patients with HDM-induced AR [101]. Additionally, a research from Singapore found that sublingual intake of mite extract medication ‘Staloral’ can greatly improve the quality of AR patients’ life by relieving nasal-associated symptoms [102]. As of yet, there has been no studies conducted on the effects of immunotherapies on allergic patients in Malaysia. Despite that, ‘ACARIZAX’, a form of sublingual immunotherapy (SLIT) tablet containing extracts of D. pteronyssinus and D. farinae allergens, was approved for marketing and distribution in several Southeast Asian countries, including Malaysia [103]. This tablet was shown to reduce the clinical symptoms of AR among European HDM-sensitized individuals with a lower expected risk of allergic reactions compared to subcutaneous immunotherapies (SCIT) [104]. Some of the most common adverse events related to oral-based immunotherapies were mild, inflammatory reactions around the mouth cavity and exacerbation of pre-existing rhinorrhoea; however, gastrointestinal effects were extremely rare in most cases [105].
Natural and alternative approaches
The Ministry of Health Malaysia has introduced policy statements to incorporate complementary and alternative medicine (CAM) therapies into its national healthcare system [106]. One baseline study by Siti et al. (2009) showed that herbs and herbal-based products were among some of the most extensively used medications by Malaysians for disease management [107].
Lignosus rhinocerotis, known locally as tiger’s milk mushroom (cendawan susu harimau), is a naturally occurring medicinal fungus used frequently by the native populations for mitigation of respiratory symptoms due to its potent anti-inflammatory activities [16]. The therapeutic use of L. rhinocerotis extract (LRE) in the management of airway inflammation was investigated by Muhammad et al. (2019) using ovalbumin (OVA)-induced mouse model [108]. They observed significant reductions of eosinophils, lymphocytes, neutrophils and cytokines (IL-4 and IL-5) in the bronchoalveolar lavage fluid (BALF) as well as declination in total serum IgE levels upon intranasal administration of LRE with specific dosages for 7 consecutive days. Moreover, the authors also reported a decrease in the percentage of CD4+ helper T cells in the lung-draining lymph nodes, including suppression of mucus secretion and leukocyte invasion in the lungs [108]. Johnathan et al. (2021) in their study of oral consumption of LRE on airway inflammation using OVA-induced rat models observed significant elevation of CD4+CD25+Foxp3+ regulatory T cells in the BALF after treatment with LRE [109]. They also demonstrated down regulation of allergic/asthmatic-associated genes (IL-17A and ADAM33) following 7 days of L. rhinocerotis extract gavaging [109]. The preceding studies provided ample evidence on the in vivo effects of L. rhinocerotis in regulating the inflammatory mediators of allergy and asthma. Despite that, the murine models utilized in these studies were representative of allergic asthma only; hence, their findings might not be entirely conclusive for allergic rhinitis. Due to the small sample sizes in both studies, the generalization of outcomes cannot be made as well.
Recently, a clinical prospective study by Tan et al. (2021) evaluated the efficacy of L. rhinocerotis intake on the improvement of health among a group of Malaysian volunteers [110]. The study participants orally consumed encapsulated, powdered form of L. rhinocerotis, twice daily, for 3 months, and follow-up visits after each month were conducted for examination of health status [110]. Increased levels of pulmonary functions and anti-oxidant capacities were observed with a huge reduction in respiratory symptoms as measured using validated nasal symptom questionnaire (NSQ) and visual analogue scale (VAS). Not only that, they also reported reduction in the levels of interleukins, IL-1β and IL-8 and elevation of salivary IgA levels [110]. Although seemingly promising, the lack of a placebo control group here made it difficult to assess the true efficacy of the supplement. Extended periods of treatment are also necessary to truly gauge the long-term effects of this extract. In addition, the specific contents of the supplement were not clearly mentioned, and only one type of dosage was used. There is also a strong potential for biasness due to the involvement of the supplier of L. rhinocerotis extract in this study.
Honey is another organic supplement taken regularly for its immunomodulatory effects. Tualang honey, produced by Apis dorsata (rock bee), is the most typically consumed honey in the practice of CAM within the central region of Malaysia [111]. The effect of Tualang honey on alleviation of airway-related symptoms was studied by Kamaruzaman et al. (2014) using ovalbumin (OVA)-induced asthmatic rabbit models. Upon treatment with aerosolized honey sprays for 5 days, marked attenuations in the levels of active eosinophils, macrophages and neutrophils were seen in the bronchoalveolar lavage fluid (BALF), alongside inhibitions of goblet cell hyperplasia in the lung airway lumens [112]. These findings provide sufficient initial evidence on the influence of Tualang honey in the management of asthma. The authors, however, did not disclose full information regarding the source and method of preparation of the aerosolized honey used in this study. No justifications were given on the use of only two concentrations of honey either. Future in vivo studies investigating the rescue and preventative effects of honey using murine models of AR will be useful in order to replicate the outcomes of the study by Kamaruzaman et al. (2014) in the nasal mucosa.
In a double-blinded, randomized-placebo controlled trial, Asha’ari et al. (2013) showed that oral ingestion of raw, unprocessed Tualang honey, in complementary with anti-histamine, could provide nasal symptom relief among Malaysian allergic rhinitis patients [15]. The placebo and treatment groups took 10 mg of loratadine for the first 4 weeks of the study, alongside honey-flavoured corn syrup (for placebo group only) and pure Tualang honey (for treatment group only). From weeks 5 until 8, the uptake of anti-histamine and the respective treatments were discontinued. At the end of the study, subjects from the treated group reported significant improvement in their nasal symptoms compared to the placebo group [15]. It should be taken into consideration that no laboratory assessment of serum total and specific IgE levels was performed during this study. Besides, clinical evaluation of nasal symptoms was not conducted during each follow-up as well. The short period of study and small sample size made it difficult to conclusively attribute the observed improvements to the intervention given.
Another randomized-controlled study by Abd Manab et al. (2018) investigated the potential role of Tualang honey as an adjunct therapy in the treatment of moderate to severe persistent allergic rhinitis [113]. The control and trial groups took intranasal corticosteroids and oral anti-histamines for a duration of 6 weeks, but only the trial group received an additional treatment of intranasal Tualang honey spray, taken daily at night throughout the same period. As a result, significant improvements in the symptom scores for nasal blockage, discharging and sneezing as well as reductions in total IgE levels were observed for both groups between weeks 0 and 6 of this study [113]. There was no significant difference between the control and trial groups for all of the parameters measured. Of note, the formulations used for preparation of the intranasal honey spray were well-described in this study. Unfortunately, this is non-blinded research wherein the trial group was pre-informed regarding the contents of the intranasal honey spray earlier on in the study. This might have created performance bias which could greatly affect interpretation of the data obtained. The lack of a proper placebo control group has also limited the confidence in the findings of this study.
Virgin coconut oil (VCO) is popularly used in the management of atopic dermatitis (AD) due to its anti-oxidant, anti-inflammatory and antibacterial properties [114]. The impact of virgin coconut oil intake on attenuation of airway/nasal inflammation has not been widely studied. One study by Kamalaldin et al. (2017) determined that the intrusion of inflammatory cells as well as the number of goblet and proliferative cells in the airway lumenwas significantly lower in VCO-treated allergic asthma models [115]. The authors also inferred that VCO performed better as a rescue agent rather than a preventive one in the case of asthma. These findings, however, may not be entirely relevant for AR due to their assessment of airway inflammation only. Zainuddin et al. (2016), in their randomized-control trial, concluded that ingestion of virgin coconut oil did not improve the symptoms of Malaysian AR patients when taken in complementary to anti-histamine (loratadine) [116]. A huge proportion of the study subjects (58.0%) reported gastrointestinal side effects throughout the 28-day period of study. This might be related to the consumption of high volume of VCO per day (30 mL) without cooking. Additionally, the exact source and composition of the VCO used in this study was not disclosed, thereby making it difficult to elucidate the findings obtained. Further studies are necessary to fully understand the effects of virgin coconut oil in the amelioration of AR symptoms.
Although not traditionally used in the management of allergic rhinitis, the efficacy of snakehead fish (Channa striatus) or Haruan supplementation as a therapeutic adjuvant for AR was researched recently. Susibalan et al. (2018) demonstrated significant improvement in nasal blockage and itchiness, alongside reduction in ocular pruritus among Malaysian allergic rhinitis patients after supplementation with oral Channa striatus (CS) extract [117]. This treatment was taken in complementary with anti-histamine (levocetirizine) and topical intranasal corticosteroid (fluticasone furoate) for 6 weeks. The serum IgE levels of the CS-treated group were also found to be significantly lower than that of the placebo groups’ at the end of the study. This is a well-constructed randomized, double-blinded, placebo-controlled trial which could have benefitted further with a larger population size and longer study period. There were no internal side effects in the consumption of this extract as evidenced by laboratory assessments of full blood count (FBC), renal profile (RP) and liver function test (LFT). Bakar et al. (2019) further investigated changes in inflammatory markers upon oral consumption of CS extract alongside daily application of corticosteroid nasal spray (mometasone furoate) for 6 weeks [118]. They observed no significant difference in the serum eosinophil counts and IL-4 levels between treated and placebo control groups. However, within the CS-treated group itself, there were substantial improvements in the nasal symptom scores and reductions in eosinophil counts and IL-4 levels between weeks 1 and 6 of this study. This study could have included an additional control group with corticosteroid treatment alone to further validate the findings gathered. Albeit with inconclusive efficacy, the low-risk safety profiles associated with consumption of Channa striatus (CS) extract might be beneficial for AR patients seeking for an alternative treatment option.
Nonetheless, ingestion of any kind of natural/tropical remedies requires safe and proper dosing techniques in order to hinder harmful toxicological consequences; as depicted in one local case of accidental self-poisoning with Datura stramonium (Kecubung fruit), a highly toxic plant used traditionally for treatment of allergic rhinitis in the East Coast of Malaysia [17]. Similar cases of poisoning with seeds of this fruit had also been reported in Canada [119] and Greece [120]. The toxicity of D. stramonium can be attributed to the presence of tropane alkaloids and several other active bio-compounds in various concentrations throughout all parts of this plant [121]. It is therefore highly imperative that the consumption of this plant or any of its parts is discontinued until sufficient evidence is available regarding its usage in treating AR or any other disorders in general.
Besides organic medications, facial candling or lilin resdung is another therapeutic approach practiced primarily by the Malays for alleviation of various nasal-related conditions including flu, rhinitis and sinusitis [122]. This method involves passing of lighted herbalised candle over the patient’s face for an extended period of time, as it is believed that the aroma from the herbal blend helps to promote relaxation to the patient by mainly relieving nasal pressures. Despite its claimed benefits, only mixed responses were obtained regarding the effectiveness of facial candling in countering the symptomatic effects of allergic rhinitis [123, 124].
Conclusion
The current study has comprehensively assessed and evaluated published literatures on the epidemiology, aetiology and therapy of allergic rhinitis in Malaysia. Due to limitation of data availability, the nationwide prevalence of AR in Malaysia cannot be established. Nevertheless, existing information on the percentages of recorded cases of AR among children and teenagers alone indicated distinct increments over the last few years. The reason for this might be attributed to the fact that Malaysia has been experiencing massive growths in the rates of urbanization and industrialization recently. Therefore, a modernized way of living and climatic changes owing to air pollution greatly exposes the public to putative risk factors linked with AR manifestation. Sensitization towards a myriad of biological and chemical derivatives is also of substantial importance, most of which can further aggravate the underlying allergic disorder.
Disparities in the disease distribution within different subpopulations raises the pertinent question of whether genetics, an often-overlooked player, lay the basis for allergic rhinitis susceptibility. Needless to say, scientists worldwide have managed to somewhat describe and understand noteworthy correlations between genetics and AR to a certain extent, but there is still a long way to go. Scarcity of research in this field of allergy immunogenetics in Malaysia has opened up endless possibilities for future scientific endeavours. Treatment wise, both conventional and alternative medications are meant to provide temporary relief only, although allergen-specific immunotherapies may hold some promise in ensuring complete resolution of the allergic condition. With that being said, healthcare providers especially pharmaceutical researchers are urged to review and discover new treatment options that are personalized based on the patients’ individual demographics and medical histories.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- AR:
-
Allergic rhinitis
- HLA:
-
Human leukocyte antigen
References
Wheatley LM, Togias A (2015) Allergic rhinitis. N Engl J Med. 372(5):456–463. https://doi.org/10.1056/NEJMcp1412282
Bjermer L, Westman M, Holmström M, Wickman MC (2019) The complex pathophysiology of allergic rhinitis: scientific rationale for the development of an alternative treatment option. Allergy Asthma Clin Immunol. 15(1):1–15. https://doi.org/10.1186/s13223-018-0314-1
Leung R, Ho P (1994) Asthma, allergy, and atopy in three south-east Asian populations. Thorax. 49(9):3–4 http://thorax.bmj.com/
Quah BS, Pauzi IW, Ariffin N, Mazidah AR (2005) Prevalence of asthma, eczema and allergic rhinitis: two surveys, 6 years apart, in Kota Bharu, Malaysia. Respirology 10(2):244–249. https://doi.org/10.1111/j.1440-1843.2005.00645.x
Norbäck D, Hashim JH, Cai GH et al (2016) Rhinitis, ocular, throat and dermal symptoms, headache and tiredness among students in schools from Johor Bahru, Malaysia: associations with fungal DNA and mycotoxins in classroom dust. PLoS One. 11(2):e0147996. https://doi.org/10.1371/journal.pone.0147996
Kulthanan K, Chusakul S, Recto MT et al (2018) Economic burden of the inadequate management of allergic rhinitis and urticaria in Asian countries based on the GA2LEN model. Allergy Asthma Immunol Res. 10(4):370–378. https://doi.org/10.4168/aair.2018.10.4.370
Mir E, Panjabi C, Shah A (2012) Impact of allergic rhinitis in school going children. Asia Pac Allergy. 2(2):93. https://doi.org/10.5415/apallergy.2012.2.2.93
Passali D, Cingi C, Staffa P, Passali F, Muluk NB, Bellussi ML (2018) The International study of the allergic rhinitis survey: outcomes from 4 geographical regions. Asia Pac Allergy. 8(1):e7. https://doi.org/10.5415/apallergy.2018.8.e7
Brozek G, Lawson J, Szumilas D, Zejda J (2015) Increasing prevalence of asthma, respiratory symptoms, and allergic diseases: four repeated surveys from 1993-2014. Respir Med. 109(8):982–990. https://doi.org/10.1016/j.rmed.2015.05.010
Zar HJ, Ehrlich RI, Workman L, Weinberg EG (2007) The changing prevalence of asthma, allergic rhinitis and atopic eczema in African adolescents from 1995 to 2002. Pediatr Allergy Immunol. 18(7):560–565. https://doi.org/10.1111/j.1399-3038.2007.00554.x
Zhang L, Zhang Y (2019) Increasing prevalence of allergic rhinitis in China. Allergy Asthma Immunol Res. 11(2):156–169. https://doi.org/10.4168/aair.2019.11.2.156
Mohd Isa KN, Hashim Z, Jalaludin J, Norbäck D, Jabbar MA, Hashim JH (2020) The impact of exposure to indoor pollutants on allergy and lung inflammation among school children in Selangor, Malaysia: an evaluation using factor analysis. Aerosol Air Qual Res. 20(11):2371–2383. https://doi.org/10.4209/AAQR.2020.03.0128
Brożek JL, Bousquet J, Agache I et al (2017) Allergic rhinitis and its impact on asthma (ARIA) guidelines—2016 revision. J Allergy Clin Immunol. 140(4):950–958. https://doi.org/10.1016/j.jaci.2017.03.050
An SY, Choi HG, Kim SW et al (2015) Analysis of various risk factors predisposing subjects to allergic rhinitis. Asian Pacific J Allergy Immunol 33(2):143–151. https://doi.org/10.12932/ap0554.33.2.2015
Asha’ari ZA, Ahmad MZ, WSJ WD, Che Hussin CM, Leman I (2013) Ingestion of honey improves the symptoms of allergic rhinitis: evidence from a randomized placebo-controlled trial in the East Coast of Peninsular Malaysia. Ann Saudi Med. 33(5):469–475. https://doi.org/10.5144/0256-4947.2013.469
Nallathamby N, Phan CW, Seow SLS et al (2018) A status review of the bioactive activities of tiger milk mushroom Lignosus rhinocerotis (Cooke) Ryvarden. Front Pharmacol. 8:998. https://doi.org/10.3389/fphar.2017.00998
Mohamad N, Baharuddin KA, Ahmad R (2009) A traditional Malay myth leading to unintentional self intoxication with kecubung fruit. Southeast Asian J Trop Med Public Health. 40(6):1331–1334 Accessed 28 Feb 2020. http://www.ncbi.nlm.nih.gov/pubmed/20578469
Tengku Azhar TN, Che Hassan MR, Zazi NM et al (2020) Parental knowledge and awareness and towards allergy prevalence in Selangor. Int J Adv Sci Technol 29(9s):1628–1637 Accessed 22 June 2021. http://sersc.org/journals/index.php/IJAST/article/view/13802
Katelaris CH, Lai CKW, Rhee CS et al (2011) Nasal allergies in the Asian - Pacific population: results from the allergies in Asia-Pacific survey. Am J Rhinol Allergy. 25(Suppl. 1):S3-15. https://doi.org/10.2500/ajra.2011.25.3674
Chong SN, Chew FT (2018) Epidemiology of allergic rhinitis and associated risk factors in Asia. World Allergy Organ J. 11:17. https://doi.org/10.1186/s40413-018-0198-z
Fu X, Norbäck D, Li Y et al Associations between indoor microbiome exposure and allergic and non-allergic rhinitis for junior high school students in Terengganu, Malaysia. Authorea Prepr. Published online October 15, 2020. https://doi.org/10.22541/AU.160279753.37398847/V1
Norzila MZ, Haifa AL, Deng CT, Azizi BH (2000) Prevalence of childhood asthma and allergy in an inner city Malaysian community: intra-observer reliability of two translated international questionnaires. Med J Malaysia. 55(1):33–39 Accessed 6 Mar 2020. http://www.ncbi.nlm.nih.gov/pubmed/11072488
Ellwood P, Asher MI, Beasley R, Clayton TO, Stewart AW (2005) The International Study of Asthma and Allergies in Childhood (ISAAC): phase three rationale and methods. Int J Tuberc Lung Dis. 9(1):10–16
Kumar KA, Sarun DD, Jeppu AK (2020) Social and psychological impact of allergic rhinitis among university students in Malaysia. Indian J Public Heal Res Dev. 11(6):1336–1340. https://doi.org/10.37506/IJPHRD.V11I6.9989
Lim FL, Hashim Z, Than LTL, Said SM, Hashim JH, Norbäck D (2015) Asthma, airway symptoms and rhinitis in office workers in Malaysia: associations with house dust mite (HDM) allergy, cat allergy and levels of house dust mite allergens in office dust. PLoS One. 10(4):e0124905. https://doi.org/10.1371/journal.pone.0124905
Coskun ZO, Erdivanlı OC, Kazıkdas KÇ et al (2016) High sensitization to house-dust mites in patients with allergic rhinitis in the Eastern Black Sea region of Turkey: a retrospective study. Am J Rhinol Allergy 30(5):351–355. https://doi.org/10.2500/ajra.2016.30.4353
Lipiec A, Sybilski A, Komorowski J et al (2020) Sensitisation to airborne allergens as a risk factor for allergic rhinitis and asthma in the Polish population. Postep Dermatol Alergol. 37(5):751–759. https://doi.org/10.5114/ada.2019.84231
Locsin CGN, Jurado ML (2018) Aeroallergen sensitization and associated comorbid diseases of an adult Filipino population with allergic rhinitis. Asia Pac Allergy 8(3):e25. https://doi.org/10.5415/apallergy.2018.8.e25
Mariana A, Ho TM, Azirun MS, Wong AL (2000) House dust mite fauna in the Klang Valley, Malaysia. Southeast Asian J Trop Med Public Health. 31(4):712–721 Accessed 13 Jan 2020. http://www.ncbi.nlm.nih.gov/pubmed/11414418
Nadchatram M (2005) House dust mites, our intimate associates. Trop Biomed. 22(1):23–37
Ho TM, Murad S, Kesavapillai R, Singaram SP (1995) Prevalence of allergy to some inhalants among rhinitis patients in Malaysia. Asian Pacific J Allergy Immunol. 13(1):11–16
Kook SC, Soong SLT (1995) Specific IgE in the identification of allergens in allergic rhinitis Malaysian patients. Asian Pacific J Allergy Immunol. 13(1):23–27 Accessed 17 Feb 2020. http://www.ncbi.nlm.nih.gov/pubmed/7488340
Gendeh BS, Murad S, Razi AM, Abdullah N, Mohamed AS, Kadir KA (2000) Skin Prick test reactivity to foods in adult Malaysians with rhinitis. Otolaryngol Neck Surg. 122(5):758–762. https://doi.org/10.1016/S0194-5998(00)70211-7
Gendeh BS, Mujahid SH, Murad S, Rizal M (2004) Atopic sensitization of children with rhinitis in Malaysia. Med J Malaysia. 59(4):522–529
Asha’ari ZA, Yusof S, Ismail R, CMC H (2010) Clinical features of allergic rhinitis and skin prick test analysis based on the ARIA classification: a preliminary study in Malaysia. Ann Acad Med Singapore. 39(8):619–624 Accessed 7 Dec 2018. http://www.ncbi.nlm.nih.gov/pubmed/20838703
Zahedi FD, Gendeh BS, Husain S (2011) Sensitisation to common allergens in children with allergic rhinitis. Brunei Int Med J. 7(4):200–206 Accessed 15 Jan 2020. https://apamedcentral.org/search.php?where=aview&id=10.0000/bimj.2011.7.4.200&code=0033BIMJ&vmode=PUBREADER
Chong KT, Wong SF, Mak JW, Loh LC, Ho TM (2015) Sero-prevalence study of IgE responses to allergens from Malaysian house dust (HDM) and storage mites (SM). Trop Biomed. 32(3):524–539 Accessed 7 Mar 2020. http://www.ncbi.nlm.nih.gov/pubmed/26695214
Nadzrah SY, Zulkiflee AB, Prepageran N (2015) Common aeroallergens by skin prick test among the population in two different regions. Prim Heal Care Open Access. 5(3):1–6. https://doi.org/10.4172/2167-1079.1000206
Yadav A, Naidu R (2015) Clinical manifestation and sensitization of allergic children from Malaysia. Asia Pac Allergy. 5(2):78. https://doi.org/10.5415/apallergy.2015.5.2.78
Kttafah GH, Abdullah MS, Nasuruddin MH, Alsailawi HA (2020) Aeroallergen sensitizations with special reference to fungi sensitization among the community of Sultan Idris Education University, Malaysia. Indian J Ecol 47(4):1099–1106 Accessed 26 Aug 2021. https://www.indianjournals.com/ijor.aspx?target=ijor:ije1&volume=47&issue=4&article=038
Zahradnik E, Raulf M (2014) Animal allergens and their presence in the environment. Front Immunol. 5:76. https://doi.org/10.3389/fimmu.2014.00076
Pang KA, Pang KP, Pang EB, Cherilynn TYN, Chan YH, Siow JK (2017) Food allergy and allergic rhinitis in 435 asian patients - a descriptive review. Med J Malaysia. 72(4):215–220
Yadav A, Naidu R (2013) Indoor environmental and demographic factors of Malaysian allergic children. J Allergy Clin Immunol. 131(2):AB163. https://doi.org/10.1016/J.JACI.2012.12.1245
Bonnet B, Messaoudi K, Jacomet F et al (2018) An update on molecular cat allergens: Fel d 1 and what else? Chapter 1: Fel d 1, the major cat allergen. Allergy Asthma Clin Immunol 14:14. https://doi.org/10.1186/s13223-018-0239-8
Niesler A, Ścigała G, Izbińska BL (2016) Cat (Fel d 1) and dog (Can f 1) allergen levels in cars, dwellings and schools. Aerobiologia (Bologna). 32(3):571–580. https://doi.org/10.1007/s10453-016-9433-7
Stark PC, Celedón JC, Chew GL et al (2005) Fungal levels in the home and allergic rhinitis by 5 years of age. Environ Health Perspect. 113(10):1405–1409. https://doi.org/10.1289/ehp.7844
Songnuan W, Bunnag C, Soontrapa K et al (2018) Airborne fungal spore distribution in Bangkok, Thailand: correlation with meteorological variables and sensitization in allergic rhinitis patients. Aerobiologia (Bologna). 34(4):513–524. https://doi.org/10.1007/s10453-018-9527-5
Ishlah LW, Gendeh BS (2005) Skin prick test reactivity to common airborne pollens and molds in allergic rhinitis patients. Med J Malaysia. 60(2):194–200
Norbäck D, Hashim JH, Markowicz P et al (2016) Endotoxin, ergosterol, muramic acid and fungal DNA in dust from schools in Johor Bahru, Malaysia - associations with rhinitis and sick building syndrome (SBS) in junior high school students. Sci Total Environ. 545-546:95–103. https://doi.org/10.1016/j.scitotenv.2015.12.072
Ding X, Su W, Ding X (2015) Methods of endotoxin detection. J Lab Autom. 20(4):354–364. https://doi.org/10.1177/2211068215572136
Braga CR, Rizzo MCV, Naspitz CK, Solé D (2004) Nasal provocation test (NPT) with isolated and associated dermatophagoides pteronyssinus (Dp) and endotoxin lipopolysaccharide (LPS) in children with allergic rhinitis (AR) and nonallergic controls. J Investig Allergol Clin Immunol. 14(2):142–148 Accessed 8 March 2020. http://www.ncbi.nlm.nih.gov/pubmed/15301304
Rufo JC, Madureira J, Paciência I et al (2017) Indoor fungal diversity in primary schools may differently influence allergic sensitization and asthma in children. Pediatr Allergy Immunol. 28(4):332–339. https://doi.org/10.1111/pai.12704
Ortiz RA, Barnes KC (2015) Genetics of allergic diseases. Immunol Allergy Clin North Am. 35(1):19–44. https://doi.org/10.1016/j.iac.2014.09.014
Waage J, Standl M, Curtin JA et al (2018) Genome-wide association and HLA fine-mapping studies identify risk loci and genetic pathways underlying allergic rhinitis. Nat Genet. 50(8):1072–1080. https://doi.org/10.1038/s41588-018-0157-1
Spinola H (2017) HLA loci and respiratory allergic diseases. J Respir Res. 3(4):112–121. https://doi.org/10.17554/j.issn.2412-2424.2017.03.32
Zhao YY, Zhao YY, Li J, Zhang Y, Zhang L (2016) HLA-DRB1*08:03:02 and HLA-DQB1*06:01:01 are associated with house dust mite-sensitive allergic rhinitis in Chinese subjects. Int Forum Allergy Rhinol. 6(8):854–861. https://doi.org/10.1002/alr.21747
Morii W, Sakai A, Ninomiya T et al (2018) Association of Japanese cedar pollinosis and sensitization with HLA-DPB1 in the Japanese adolescent. Allergol Int. 67(1):61–66. https://doi.org/10.1016/j.alit.2017.04.004
Dhaliwal JS, Shahnaz M, Too CL et al (2007) HLA-A, -B and -DR allele and haplotype frequencies in Malays. Asian Pacific J allergy Immunol. 25(1):47–51 Accessed 11 Dec 2018. http://www.ncbi.nlm.nih.gov/pubmed/17891921
Azira NMS, Zeehaida M, Nurul KY (2013) HLA DR/DQ type in a Malay population in Kelantan, Malaysia. Malays J Pathol. 35(1):65–69 Accessed 11 Dec 2018. http://www.ncbi.nlm.nih.gov/pubmed/23817396
Edinur HA, Zafarina Z, Spínola H, Nurhaslindawaty AR, Panneerchelvam S, Norazmi MNN (2009) HLA polymorphism in six Malay subethnic groups in Malaysia. Hum Immunol. 70(7):518–526. https://doi.org/10.1016/J.HUMIMM.2009.04.003
Tan LK, Farid BM, Salsabil S et al (2016) HLA-A, -B, -C, -DRB1 and -DQB1 alleles and haplotypes in 951 Southeast Asia Malays from Peninsular Malaysia. Hum Immunol. 77(10):818–819. https://doi.org/10.1016/j.humimm.2016.06.022
Koh CL, Benjamin DG (1994) HLA DQα genotype and allele frequencies in Malays, Chinese, and Indians in the Malaysian population. Hum Hered. 44(3):150–155. https://doi.org/10.1159/000154207
Allia S, Norazmi MN, Panneerchelvam S, Zafarina Z (2019) The pattern of HLA-A, -B and -DRB1 alleles and haplotypes of four Malay sub-ethnic groups namely Kelantan, Champa, Patani and Mandailing Malays of Peninsular Malaysia. Hum Immunol. 80(7):423–424. https://doi.org/10.1016/j.humimm.2019.02.015
Too CL, Tan LK, Heselynn H et al (2019) HLA-A, -B, -C, -DRB1 and -DQB1 alleles and haplotypes in 194 Southeast Asia Chinese from Peninsular Malaysia. Hum Immunol. 80(11):906–907. https://doi.org/10.1016/j.humimm.2019.09.005
Dhaliwal JS, Shahnaz M, Azrena A et al (2010) HLA polymorphism in three indigenous populations of Sabah and Sarawak. Tissue Antigens. 75(2):166–169. https://doi.org/10.1111/j.1399-0039.2009.01410.x
Jinam TA, Saitou N, Edo J, Mahmood A, Phipps ME (2010) Molecular analysis of HLA class I and class II genes in four indigenous Malaysian populations. Tissue Antigens. 75(2):151–158. https://doi.org/10.1111/j.1399-0039.2009.01417.x
Tasnim AR, Allia S, Edinur HA, Panneerchelvam S, Zafarina Z, Norazmi MN (2016) Distribution of HLA-A, -B and -DRB1 alleles in the Kensiu and Semai Orang Asli sub-groups in Peninsular Malaysia. Hum Immunol. 77(8):618–619. https://doi.org/10.1016/j.humimm.2016.06.009
Azizah MR, Ainol SS, Kong NC, Normaznah Y, Rahim MN (2001) HLA antigens in Malay patients with systemic lupus erythematosus: association with clinical and autoantibody expression. Korean J Intern Med. 16(2):123–131. https://doi.org/10.3904/kjim.2001.16.2.123
Azizah MR, Ainoi SS, Kuak SH, Kong NC, Normaznah Y, Rahim MN (2001) The association of the HLA class II antigens with clinical and autoantibody expression in Malaysian Chinese patients with systemic lupus erythematosus. Asian Pacific J Allergy Immunol. 19(2):93–100 Accessed 13 Feb 2020. http://www.ncbi.nlm.nih.gov/pubmed/11699726
Yusuf YM, Phipps ME, Chow SK, Yeap SS (2011) HLA-A*11 and novel associations in Malays and Chinese with systemic lupus erythematosus. Immunol Lett. 139(1-2):68–72. https://doi.org/10.1016/j.imlet.2011.05.001
Kong KF, Yeap SS, Chow SK, Phipps ME (2002) HLA-DRB1 genes and susceptibility to rheumatoid arthritis in three ethnic groups from Malaysia. Autoimmunity. 35(4):235–239. https://doi.org/10.1080/08916930290024179
Dhaliwal JS, Wong L, Kamaluddin MA, Yin LY, Murad S (2011) Susceptibility to aplastic anemia is associated with HLA-DRB1*1501 in an aboriginal population in Sabah, Malaysia. Hum Immunol 72(10):889–892. https://doi.org/10.1016/j.humimm.2011.06.013
Hassan N, Dhaliwal JS, Ibrahim HM et al (2015) Increased soluble HLA-DRB1 in B-cell acute lymphoblastic leukaemia. Malays J Pathol. 37(2):83–90 Accessed 13 Feb 2020. http://www.ncbi.nlm.nih.gov/pubmed/26277663
Chang CC, Too CL, Murad S, Hussein SH (2011) Association of HLA-B1502 allele with carbamazepine-induced toxic epidermal necrolysis and Stevens-Johnson syndrome in the multi-ethnic Malaysian population. Int J Dermatol. 50(2):221–224. https://doi.org/10.1111/j.1365-4632.2010.04745.x
Then SM, Rani ZZM, Raymond AA, Ratnaningrum S, Jamal R (2011) Frequency of the HLA-B*1502 allele contributing to carbamazepine-induced hypersensitivity reactions in a cohort of Malaysian epilepsy patients. Asian Pacific J Allergy Immunol. 29(3):290–293
Ramasamy A, Curjuric I, Coin LJ et al (2011) A genome-wide meta-analysis of genetic variants associated with allergic rhinitis and grass sensitization and their interaction with birth order. J Allergy Clin Immunol. 128(5):996–1005. https://doi.org/10.1016/j.jaci.2011.08.030
Bønnelykke K, Matheson MC, Pers TH et al (2013) Meta-analysis of genome-wide association studies identifies ten loci influencing allergic sensitization. Nat Genet. 45(8):902–906. https://doi.org/10.1038/ng.2694
Andiappan AK, Wang DY, Anantharaman R et al (2011) Genome-wide association study for atopy and allergic rhinitis in a Singapore Chinese population. PLoS One. 6(5):e19719. https://doi.org/10.1371/journal.pone.0019719
Li YJ, Chen J, Rui XQ, Li N, Jiang F, Shen J (2018) The association between sixteen genome-wide association studies-related allergic diseases loci and childhood allergic rhinitis in a Chinese Han population. Cytokine. 111:162–170. https://doi.org/10.1016/j.cyto.2018.08.022
Fujii R, Hishida A, Wu MC et al (2018) Genome-wide association study for pollinosis identified two novel loci in interleukin (IL)-1B in a Japanese population. Nagoya J Med Sci. 80(1):109–120. https://doi.org/10.18999/nagjms.80.1.109
Yadav A, Govindasamy GK, Naidu R (2013) Polymorphic variants of interleukin-13 R130Q, interleukin-4 T589C, interleukin-4RA I50V, and interleukin-4RA Q576R in allergic rhinitis: a pilot study. Allergy Rhinol. 3(1):35–40. https://doi.org/10.2500/ar.2012.3.0022
Corsico AG, Amici MD, Ronzoni V et al (2017) Allergen-specific immunoglobulin E and allergic rhinitis severity. Allergy Rhinol. 8(1):1–4. https://doi.org/10.2500/ar.2017.8.0187
Ciprandi G, Cirillo I (2011) Monosensitization and polysensitization in allergic rhinitis. Eur J Intern Med. 22(6):e75–e79. https://doi.org/10.1016/j.ejim.2011.05.009
Ha EK, Baek JH, Lee SY et al (2016) Association of polysensitization, allergic multimorbidity, and allergy severity: a cross-sectional study of school children. Int Arch Allergy Immunol. 171(3-4):251–260. https://doi.org/10.1159/000453034
Cuvillo AD (2010) Validation of ARIA duration and severity classifications in Spanish allergic rhinitis patients - the ADRIAL cohort study. Rhinol J. 48(2):201–205. https://doi.org/10.4193/Rhin09.099
Jamalyaria F, Ward MM, Assassi S et al (2017) Ethnicity and disease severity in ankylosing spondylitis a cross-sectional analysis of three ethnic groups. Clin Rheumatol. 36(10):2359–2364. https://doi.org/10.1007/s10067-017-3767-6
Crosslin KL, Wiginton KL (2009) The impact of race and ethnicity on disease severity in systemic lupus erythematosus. Ethn Dis. 19(3):301–307
Amini P, Abdullah M, Seng LS et al (2016) Ethnicity influences disease characteristics and symptom severity in allergic rhinitis patients in Malaysia. Int Forum Allergy Rhinol. 6(6):624–630. https://doi.org/10.1002/alr.21442
Elango S (2005) Recent trends in the diagnosis and management of allergic rhinitis. Med J Malaysia. 60(5):672–677 Accessed13 Nov 2018. http://www.ncbi.nlm.nih.gov/pubmed/16515128
Malaysian Allergy Prevention (MAP) Guidelines for healthcare professionals. Published 2014. Accessed 10 Jan 2020. https://www.allergymsai.org/guideline-map.html
Saraiza AB, Khizuan AK, Leow WL, Yanti BA, Putra SHAP (2017) Use of antihistamines and nasal decongestants. Pharmaceutical Services Division, Ministry of Health Malaysia
Abdullah B, Snidvongs K, Recto M, Poerbonegoro NL, Wang DY (2020) Primary care management of allergic rhinitis: a cross-sectional study in four ASEAN countries. Multidiscip Respir Med. 15(1):726. https://doi.org/10.4081/MRM.2020.726
Horak F, Zieglmayer UP (2009) Azelastine nasal spray for the treatment of allergic and nonallergic rhinitis. Expert Rev Clin Immunol. 5(6):659–669. https://doi.org/10.1586/eci.09.38
Aneeza WH, Husain S, Rahman RA, Van DD, Abdullah A, Gendeh BS (2013) Efficacy of mometasone furoate and fluticasone furoate on persistent allergic rhinoconjunctivitis. Allergy Rhinol. 4(3):e126. https://doi.org/10.2500/AR.2013.4.0065
Goh B, Ismail MI, Husain S (2014) Quality of life assessment in patients with moderate to severe allergic rhinitis treated with montelukast and/or intranasal steroids: a randomised, double-blind, placebo-controlled study. J Laryngol Otol. 128(3):242–248. https://doi.org/10.1017/S002221511400036X
Abdullah B, Kandiah R, Hassan NFHN, Ismail AF, Mohammad ZW, Wang DY (2020) Assessment of perception, attitude, and practice of primary care practitioners towards allergic rhinitis practice guidelines: development and validation of a new questionnaire. World Allergy Organ J. 13(12):100482. https://doi.org/10.1016/J.WAOJOU.2020.100482
Prepageran N, Wang DY, Nair G, Maurer M (2014) The status quo and unmet needs in the management of allergic rhinitis and chronic rhinosinusitis: a Malaysian perspective. Asia Pac Allergy. 4(3):142. https://doi.org/10.5415/apallergy.2014.4.3.142
Abdullah B, Latiff AHA, Woo K et al (2019) Using patient profiles to guide the choice of antihistamines in the primary care setting in Malaysia: expert consensus and recommendations. Ther Clin Risk Manag. 15:1267–1275. https://doi.org/10.2147/TCRM.S221059
Kouzegaran S, Zamani MA, Faridhosseini R et al (2018) Immunotherapy in allergic rhinitis: it’s effect on the immune system and clinical symptoms. Open Access Maced J Med Sci. 6(7):1248–1252. https://doi.org/10.3889/oamjms.2018.264
Zhang HZ, Xie W, Wang Y, Chen J, Wen TH (2018) Dermatophagoides farinae allergen encapsule for oral immunotherapy with HDM allergic rhinitis. Syst Appl Acarol. 23(9):1782–1795. https://doi.org/10.11158/saa.23.9.5
Fujisawa T, Shimoda T, Masuyama K et al (2018) Long-term safety of subcutaneous immunotherapy with TO-204 in Japanese patients with house dust mite-induced allergic rhinitis and allergic bronchial asthma: multicenter, open label clinical trial. Allergol Int. 67(3):347–356. https://doi.org/10.1016/j.alit.2017.11.004
Soh JY, Thalayasingam M, Ong S, Loo EXL, Shek LP, Chao SS (2016) Sublingual immunotherapy in patients with house dust mite allergic rhinitis: prospective study of clinical outcomes over a two-year period. J Laryngol Otol. 130(3):272–277. https://doi.org/10.1017/S0022215116000025
ALK releases its annual report 2015 - EconoTimes. Accessed May 12, 2021. https://www.econotimes.com/ALK-releases-its-annual-report-2015-157723
Williamson KAL (2016) Standardized quality house dust mite sublingual tablets (Acarizax®): a guide to their use as sublingual allergy immunotherapy in Europe. Drugs Ther Perspect. 32(12):502–509. https://doi.org/10.1007/s40267-016-0349-7
Liu X, Ng CL, Wang DY (2018) The efficacy of sublingual immunotherapy for allergic diseases in Asia. Allergol Int. 67(3):309–319. https://doi.org/10.1016/j.alit.2018.02.007
The National Policy of Traditional and Complementary Medicine. 2nd ed.; 2007.
Siti ZM, Tahir A, Farah AI et al (2009) Use of traditional and complementary medicine in Malaysia: a baseline study. Complement Ther Med. 17(5-6):292–299. https://doi.org/10.1016/j.ctim.2009.04.002
Muhamad S, Muhammad N, Ismail N, Mohamud R, Safuan S, Nurul A (2019) Intranasal administration of Lignosus rhinocerotis (Cooke) Ryvarden (tiger milk mushroom) extract attenuates airway inflammation in murine model of allergic asthma. Exp Ther Med. 17(5):3867–3876. https://doi.org/10.3892/etm.2019.7416
Johnathan M, Muhamad SA, Gan SH et al (2021) Lignosus rhinocerotis Cooke Ryvarden ameliorates airway inflammation, mucus hypersecretion and airway hyperresponsiveness in a murine model of asthma. PLoS One. 16(3):e0249091. https://doi.org/10.1371/JOURNAL.PONE.0249091
Tan ESS, Leo TK, Tan CK (2021) Effect of tiger milk mushroom (Lignosus rhinocerus) supplementation on respiratory health, immunity and antioxidant status: an open-label prospective study. Sci Reports 11(1):1–10. https://doi.org/10.1038/s41598-021-91256-6
Wahab MSA, Othman N, Othman NHI, Jamari AA, Ali AA (2017) Exploring the use of and perceptions about honey as complementary and alternative medicine among the general public in the state of Selangor, Malaysia ARTICLE INFO ABSTRACT. J Appl Pharm Sci. 7(12):144–150. https://doi.org/10.7324/JAPS.2017.71220
Kamaruzaman NA, Sulaiman SA, Kaur G, Yahaya B (2014) Inhalation of honey reduces airway inflammation and histopathological changes in a rabbit model of ovalbumin-induced chronic asthma. BMC Complement Altern Med. 14:176. https://doi.org/10.1186/1472-6882-14-176
Abd Manab FW, Abdullah B, Shukri NM et al (2018) Efficacy of intranasal honey spray: as an adjunct treatment for allergic rhinitis. J Aust Tradit Soc. 24(1):20–25
Chew YL (2019) The beneficial properties of virgin coconut oil in management of atopic dermatitis. Pharmacogn Rev. 13:24–27. https://doi.org/10.4103/phrev.phrev_29_18
Kamalaldin NA, Sulaiman SA, Yusop MR, Yahaya B (2017) Does inhalation of virgin coconut oil accelerate reversal of airway remodelling in an allergic model of asthma? Int J Inflam. Published online. https://doi.org/10.1155/2017/8741851
Zainuddin N, Mohd Shah NA, Salim R (2016) Effects of virgin coconut oil as adjunct therapy in the treatment of allergic rhinitis. J Clin Heal Sci. 1(1):22–28 Accessed 22 Aug 2021. http://www.mmc.gov.my/v1/index.php/list-of-
Susibalan BD, Abdullah B, Lazim NM, Kadir AA (2018) Efficacy of snakehead fish (Channa striatus) in subjects with allergic rhinitis: a randomized controlled trial. Orient Pharm Exp Med. 18(3):209–215. https://doi.org/10.1007/s13596-018-0327-9
Abu Bakar MN, Abdullah B, Mohamad I, Lazim NM, Yahya NK, Kadir AA (2018) Efficacy of snakehead fish (Channa striatus) extract supplementation in allergic rhinitis patients: a randomized double blind placebo controlled trial. Int Med J. 26(4):297–300. https://doi.org/10.1007/s13596-018-0327-9
Spina SP, Taddei A (2007) Teenagers with Jimson weed (Datura stramonium) poisoning. Can J Emerg Med. 9(6):467–469. https://doi.org/10.1017/S1481803500015530
Boumba V, Mitselou A, Vougiouklakis T (2004) Fatal poisoning from ingestion of Datura stramonium seeds. Vet Hum Toxicol. 46(2):81–82 Accessed23 August 2021. https://europepmc.org/article/med/15080209
Gaire B, Subedi L (2013) A review on the pharmacological and toxicological aspects of Datura stramonium L. J Integr Med. 11(2):73–79. https://doi.org/10.3736/JINTEGRMED2013016
Fatikah Ismail NF, Neoh CF, Lim SM et al (2017) The immediate effect of facial candling on inflammatory mediators, substance P, symptoms severity, and quality of life in allergic rhinitis patients: study protocol for a randomized controlled trial. Med. 96(30):e7511. https://doi.org/10.1097/MD.0000000000007511
Fatikah Ismail N, Neoh C, Lean Q et al (2018) Facial candling for the treatment of allergic rhinitis in young adults: a qualitative study. J Pharm Bioallied Sci. 10(4):199. https://doi.org/10.4103/jpbs.jpbs_33_18
Athiraah Hamdan NK, Lean QY, Neoh CF et al (2020) Knowledge and perception of facial candling for allergic rhinitis among university staff and students. Evidence-based Complement Altern Med. Published online:5713134. https://doi.org/10.1155/2020/5713134
Acknowledgements
Not applicable
Funding
This study is funded by the Fundamental Research Grant Scheme (FRGS), Ministry of Higher Education (MOHE), Malaysia (04-01-17-1907FR).
Author information
Authors and Affiliations
Contributions
VP and MA conceived, designed and drafted the manuscript, while FN and STS provided critical revision of the article. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prasad, V., Abdullah, M., Nordin, F. et al. Prevalence, causes and treatments of allergic rhinitis in Malaysia: a literature review. Egypt J Otolaryngol 38, 170 (2022). https://doi.org/10.1186/s43163-022-00361-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00361-4