Abstract
Background
Universal newborn hearing screening (UNHS) has been widely adopted worldwide as a standard of care because it enables the detection of congenital hearing loss early in life. Therefore, the concepts of regular measurement of performance using pre-determined quality measures are recommended for continuous improvement of the program. This study aimed to evaluate and update the performance of a UNHS program by measuring the recommended quality measures between 2010 and 2019. A retrospective study analyzing data of 50569 babies screened between January 2010 and December 2019 was performed. The pre-determined quality measures of coverage rate, initial referral rate, return to follow-up rate, diagnosis rate, and age at diagnosis were measured.
Results
The average coverage rate was 95.5%, with all years achieving the recommended benchmark of ≥ 95% except 2014 (91.8%) and 2019 (89.5%). Generally, the initial referral rate (10%) exceeded the benchmark of ≤ 4%. The program only managed to reach the benchmark for initial referral rate in 2013, 2014, and 2015. Both quality indicators for return to follow-up and diagnosis rates also did not meet the ≥ 95% and ≥ 90% standards, respectively. The return to follow-up ranged from 62 to 72.7%, while the average diagnosis rate was 73.4% (60–100%). One hundred thirty-seven infants were diagnosed with hearing loss at a median age of 3.8 months (± 0.4 months), resulting in a prevalence of 0.27%.
Conclusion
The findings demonstrated an excellent coverage rate but unsatisfactory performance for other quality indicators. Hence, the current program needs to be revisited to remain relevant and effective.
Similar content being viewed by others
Background
Congenital hearing loss is one of the most common disabilities, with a prevalence estimate at 1 to 3 healthy newborns per 1000 lives and 2 to 4 per 100 in high-risk infants [1]. The rapid improvement in technologies has allowed congenital hearing loss to be detected early in life through universal newborn hearing screening (UNHS). In addition, UNHS has been demonstrated to be effective in minimizing the deleterious impact on language, cognitive, and psychosocial development of children diagnosed with congenital hearing loss [2]. Moreover, the age of diagnosis has been lowered tremendously with the introduction of this program. For example, the age at diagnosis in Holte et al. [3] study ranged from 0.5 to 70 months. These positive outcomes have made UNHS a standard practice of care all over the world.
To date, UNHS has been carried out in many countries across the globe. For instance, 98.3% of 4 million infants born in the United States of America received screening through this program [4]. There have been no national UNHS yet in Malaysia, but this program has been carried out through public and private hospital initiatives. For public hospitals, 15 UNHS programs were offered in 2015 [5]. Hospital Canselori Tuanku Mukhriz (HCTM) is among the few hospitals implementing UNHS since the early 2000s [6, 7]. The program follows the Joint Committee on Infant Hearing (JCIH) guidelines to identify newborns with congenital hearing loss by the age of 3 months and to initiate appropriate intervention by 6 months [8]. The guidelines also promote continuous quality measurement to track the program’s performance. A few quality indicators have been outlined in the guidelines, including the coverage rate, initial referral rate, return to follow-up rate, and age at diagnosis. In countries where UNHS has been implemented, the coverage rate varied between 90.9% in China [9] and 99.8% in Singapore [10], while the proportion of newborns referred for re-screening varied between 0.6% and 37.9% [11]. Accordingly, two previous studies have been conducted to measure the performance of the UNHS program at HCTM in the early years of its implementation. Mukari et al. [6] measured the program's performance from April 2003 to February 2004 and found that all the measured quality indicators did not meet the recommended benchmarks. For example, the coverage was only 84.6%, and the average referral rate was 12%. Abdullah et al. [12] revisited the program’s performance from April 2003 to December 2005. Significant improvements were observed in the program’s coverage rate, initial referral rate and age of diagnosis. However, their findings were still unsatisfactory when compared to the JCIH guidelines.
In conclusion, these studies’ results are more than a decade old and using data gathered within a short-term period that did not allow for the assessments of trends or changes over time. Moreover, a change in the screening protocol, from three-step to two-step, has been implemented following the finding from the 2008 study [12]. To date, there have been no studies conducted after the change in protocol. Given that the protocol has been using for several years, there is a need to update the quality indicators and monitor the progress of the program with a more extended study period. This comprehensive evaluation will help HCTM identify the program's strengths and weaknesses to achieve the set benchmarks. Therefore, this study aimed to assess the performance of the HCTM program over 10 years and determine whether it meets the recommended international benchmarks.
Methods
A retrospective study design was employed to review the screening results from infants born in HCTM between January 2010 and December 2019. This study was approved by Research Ethics Committee of Universiti Kebangsaan Malaysia (UKM PPI/111/8/JEP-2021-041). The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki. Written informed consent was obtained from each participant/patient for study participation and data publication.
Hearing screening procedure
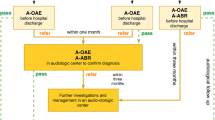
The program used a two-stage screening protocol to screen babies born at the facility using Transient Evoked Otoacoustic Emissions (TEOAE) and Automated Auditory Brainstem Response (AABR). Trained nurses and medical technologists conducted inpatient TEOAE screening on healthy newborns in the post-natal ward and neonatal intensive care unit (NICU). The screening was performed either in a room within the maternity ward or at the mother’s bedside. All healthy neonates were screened within 24 h after birth, while NICU babies received screening depending on their health status. Newborns were screened only once in the first stage with two attempts per ear. Those who failed the initial TEOAE screening were given an appointment within 2 weeks for an outpatient AABR re-screening at the Ear, Nose, and Throat (ENT) Clinic before discharge. Babies who passed the AABR re-screening were discharged, while those with failed results were scheduled to undergo a diagnostic ABR at the Audiology Unit. Figure 1 show the hearing screening protocol at HCTM.
Data management
The program collected hearing screening data (e.g., demographic information, number of babies born, date of initial screening and rescreening, initial and re-screening results, and date of diagnosis) every month and stored in the Microsoft Excel file by year of the birth cohort. The screening personnel filled out the hearing screening data, and the audiologists monitored the database. The audiologists emailed the database with a secure password to the research team. The database uses registration numbers to protect patient information, privacy, and confidentiality.
Statistical analysis
Generally, the analysis involved calculating percentages for all the quality indicators and compared these with JCIH guidelines. The median and standard deviation were also computed. Microsoft Excel was used to organize and perform the data analysis. Each month’s hearing screening data were extracted from the database and critically analysed to compute quality indicators of coverage rate, initial referral rate, return for follow-up rate, diagnosis rate, and age at diagnosis. The prevalence of hearing loss over the 10 years was also established. Table 1 shows the formulae used in computing each quality indicator together with its recommended benchmarks.
Results
Overall results of the screening process
Results of the hearing screening tests from 2010 to 2019 are summarised in Table 2. During the study period, a total of 52798 babies were born alive at HCTM, and 50633 (95.9%) received hearing screening within 1 month of age. Specifically, 46056 (91%) and 4577 (9%) healthy newborns and NICU babies received the initial screening. Of the 50633 newborns, 90.3% (45734) passed the screening, and 10% (4897) failed the initial TEOAE screening. Throughout the 10 years, only 3223 (65.8%) returned for the outpatient re-screening with AABR and 432 (13.4%) failed in the second stage screening using AABR. Only 163 completed the comprehensive assessments, and 137 (0.27%) of the 50633 were diagnosed within 3 months of age.
Quality indicators across the years
Table 3 presents the quality indicators measured for each year from 2010 to 2019.
Coverage rate
The coverage rate refers to the percentage of newborns who completed the initial screening within 1 month of age. As shown in Table 3, the coverage rate ranged from 89.5 to 97.8%. Generally, the coverage rate during the study period achieved the minimum benchmark of 95% for all years except in 2014 (91.8%) and 2019 (89.5%).
Initial referral rate
The initial referral rate is defined as the percentage of newborns who failed the initial test in either one or both ears. Table 2 shows that the initial referral rate showed a declining trend from 2010 to 2012 and met the JCIH benchmark of less than 4% in 2013 (2.3%), 2014 (2.9%), and 2015 (2.9%). However, the proportion exceeded the benchmark and showed an increasing pattern for the last three assessment years.
Return for follow-up rate
The return for follow-up rate is the proportion of newborns attending the out-patient re-screening using AABR within 4 weeks of the referral or by 44 weeks gestational age for premature babies. The return to follow-up rate fluctuated throughout the study period, ranging from 61.3 to 76.7% and never surpassing the benchmark of 95%. Within the study period, 1674 newborns did not attend the scheduled re-screening resulting in an overall loss to follow-up rate of 34.2%.
Diagnosis rate
Diagnosis rate refers to the percentage of newborns who completed the confirmation of hearing status by 3 months of age. Of 163 infants who participated in the diagnostic assessments, only 31 (19%) received evaluation within 3 months of age. The diagnosis rate for these 31 infants ranged from 5 to 36.4%. The diagnosis rate showed a decreasing pattern over the study period, with none achieving the recommended standard. Two hundred and eighty-six infants did not attend the diagnostic assessment, resulting in a 66.2% loss to diagnostic follow-up.
Age at diagnosis
Age at diagnosis is defined as the infant’s corrected age when completing the diagnostic audiology assessment. One hundred and thirty-seven infants were diagnosed with hearing loss. The overall median age was 3.9 months (± 0.4), ranging from 3.7 to 4.9 months and exceeding the recommended 3-month benchmark. However, the age at diagnosis showed a decreasing trend over the 10 years. Of 137 infants, 45 and 92 were confirmed to have unilateral and bilateral hearing loss, respectively.
Discussion
This study analyses the performance of the UNHS program conducted by a university hospital over the 10 years. The performance was measured using quality indicators which include the (1) coverage rate, (2) initial referral rate, (3) return to follow-up rate, (4) diagnosis rate, and (5) age at diagnosis.
Coverage rate
In general, the screening coverage was consistently high. The coverage rate averaging 95.5% for 2010–2019 met the recommended benchmark and aligned with other published studies [13, 14]. The high coverage rate indicates that the parents and the screeners accept the program. This high coverage rate is attributed to two main factors. First, the cost of the hearing screening is part of the maternity package and is covered by general health insurance. The screening fee covered by the third parties also plays a crucial role in increasing the coverage rate of the program in Taipei City, Taiwan [15] and Italy [16]. The second factor is associated with having dedicated personnel to conduct the screening. Within 10 years, 15 personnel were assigned by the hospital to conduct the testing and document the screening results, where each personnel carried out the duty for 2 years. These personnel attended the training courses and were supervised by the audiologists before allowing them to screen independently. The audiologists also gave refresher training to ensure the retention of knowledge and skill of the personnel. The approach of having dedicated personnel have also been found to contribute to a high coverage rate in community clinics in South Africa [15]. Frederichs et al. [17] demonstrated a lower coverage rate (22.5%) in clinics with non-permanent screening staff than facilities with dedicated personnel (74.6–84.7%). Although the coverage rate of the program was consistently high over 10 years, the program failed to reach the benchmark in 2014 and 2019. The main reason for the drop could be the change of dedicated screening personnel from March onwards for 2019. It could be possible that the new personnel required extra time to learn and adapt to the new responsibility. For 2014, the TEOAE screening tool used to screen healthy newborns broke down intermittently from January to June. When these unexpected events happened, the personnel had to discontinue the screen and most likely missed testing the babies because they had been discharged from the hospital.
Initial referral rate
Generally, referral rates of 4% or higher were recorded throughout the study period. The overall referral rate of 10% in this study vary considerably from other countries such as South Africa (37.9%) [11], Uganda (43.3%) [18], and Brazil (30%) [19]. The most likely reason for the high referral rates in the present study comes from healthy babies. The TEOAE screening for this population was usually completed within 12–24 h after birth due to early hospital discharge [12]. Detailed analysis showed that 85.6% of 4897 newborns who failed the initial screening test were from the healthy infant group. Van Dyak et al. [11] also faced a similar problem where healthy newborns in South Africa are typically discharged from the hospitals between 6 and 24 h after birth. In their study, the TEOAE refer rate for ears screened within 24 h after birth was 55%. It is known that the high initial referral rate among newborns who were screened with TEOAE before 48 h after birth is attributed to the presence of vernix in the newborn’s external ear canal. Findings by Kumari and Rangasayee [20] further supported this claim, who reported that the vernix is still present in 35.4% of healthy newborns aged less than 24 h. The vernix causes transient conductive auditory dysfunction and interferes with TEOAE screening yielding false positive results.
One of the suggestions to resolve the high referral rate issue is probably considering using AABR for in-patient screening. A few studies demonstrated that AABR screening effectively reduces the initial referral rate in programs where early discharge for healthy newborns is unavoidable. In their study, Clarke, Iqbal, and Mitchell [21] found that using AABR in the initial screening significantly reduced referral rate than TEOAE (3.7% vs 33.3%). Another suggestion is delaying the screening until near the time of discharge. Lupoli et al. [19] reported that delaying the screen by 1 h resulted in a decrease in the failure rate by 5%.
Return for follow up rate
The return for follow-up rates in the present study is far from achieving the recommended benchmark of 95% and more. The UNHS programs in Italy [16], China [22], and Turkey [23] also exhibited similar findings. The low return to follow-up would threaten the program’s effectiveness as it increases the number of missing babies with congenital hearing loss. A poor return for follow-up rate in the present study indicates that the direct booking of re-screening appointments by personnel at the point of screen completion and providing a brochure about communicative and educational risks of hearing impairment before babies are discharged were inadequate. One strategy that can be used to improve this quality indicator is to empower personnel to conduct parents counselling at the time of screening on the importance of the follow-up and the consequences of undetected or late detection of hearing loss in children. Another strategy is for the program to be proactive in contacting parents using phone calls, emails, or phone messages to remind parents about the re-screening appointment. Having efficient data management and tracking system capable of minimizing documentation loss has been proven to help improve the return for follow-up rate [24].
The high coverage rate due to early screening can also contribute to poor return for follow-up rate because vernix causes many babies to fail the initial screening tests. In all referral cases, the hearing screening personnel will inform about the vernix causing the failure and how this substance will naturally disappear from the babies’ ear canal after a few days or weeks. It is possible that the parents did not think that this condition was serious and therefore decided not to bring their babies back for rescreening. To overcome this problem, the program could perhaps consider making a second effort to re-screen babies who did not pass the initial screening close to discharge. Another suggestion is to align the re-screening with routine immunization visits, like the program in South Africa [25].
Diagnosis rate
The program did not achieve > 90% follow-up diagnostic testing by 3 months, as recommended by JCIH guidelines. The low overall rate of 3-month follow-up (19.3%) obtained in the present study is also shown in Bussé et al. [24], where only 33 of the 10.925 infants (0.3%) completed the full diagnostic assessment. The low referral rate to a full diagnostic assessment in the present study could be linked to the high number of infants lost to follow-up in the initial screening (34.2%). Additionally, 26 out of 163 infants (16%) were diagnosed with normal hearing. These false positive cases might interfere and delay the diagnosis of hearing loss of the present study. It is also possible that parents did not attend the diagnostic evaluation because they could not afford to pay the test fees and expenses to come for the diagnostic appointment. For instance, an ABR diagnostic test cost is Ringgit Malaysia (RM) 100 (approximately USD 24), which is much higher than the re-screening (roughly USD 8). This issue might add an economic burden to parents as general health insurance does not cover the test fees. Providing financial support to parents as practised in Taiwan [15] might help improve parental compliance to attend the diagnostic assessments.
Age at diagnosis
The median age at diagnosis (3.9 months) obtained in the present study was a month later than the recommended benchmark. It is important to note that the age at diagnosis in the present study was obtained from ABR threshold results without information on the type of loss. Therefore, the prevalence of 2.71 per 1000 newborns (137 of 50663) obtained in the present study includes all types of hearing loss, bilateral, or unilateral. These findings are consistent with studies in developed countries that report 1–3 cases of childhood hearing loss per 1000 live birth [1]. In other programs, such as in Bavaria, Germany, the prevalence of hearing loss only includes those with bilateral hearing loss [26]. Unilateral referrals were included in the present study because they can also negatively impact the children’s developmental and educational outcomes [27]. The present’s study actual prevalence of hearing loss in the present study could be much higher due to the low follow-up rate of the re-screening and diagnostic tests. The late diagnosis in the present could have been affected by a false positive case identified in 26 infants, which increased the waiting list for diagnostic assessments. Another source of delay in diagnosis was premature babies who only came to the diagnostic evaluation after being declared stable by the paediatricians. In the present study, the longest time taken to diagnose a premature baby was 32 months. The presence of middle ear effusion which requires several visits to doctors could also affect the age at diagnosis of the present study.
Limitations
The main limitation faced in this study was due to the insufficient documentation in the database. For example, we could not determine the prevalence of permanent childhood hearing loss because the type of hearing loss is not in the data management system. Similarly, the age of intervention and number of infants who elect amplification are also not available. This information was recorded in the babies' file and needed to be extracted manually. In addition, data in the present study originated from a single institution, limiting the result’s generalisability.
Conclusions
This study was successful in meeting the recommended benchmark of the coverage rate. However, the number of newborns who did not attend the follow-ups remains too high and jeopardizes the entire program’s effectiveness. Identifying the root cause and strategies to improve this particular quality indicator are urgently needed so that the program can meet the recommended benchmarks and the goals of early screening and intervention of childhood hearing loss.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- UNHS:
-
Universal newborn hearing screening
- HCTM:
-
Hospital Canselori Tuanku Mukhriz
- JCIH:
-
Joint Committee on Infant Hearing
- TEOAE:
-
Transient evoked otoacoustic emissions
- AABR:
-
Automated auditory brainstem response
- NICU:
-
Neonatal intensive care unit
- RM:
-
Ringgit Malaysia
References
Butcher E, Dezateux C, Cortina-Borja M, Knowles RL (2019) Prevalence of permanent childhood hearing loss detected at the universal newborn hearing screen: Systematic review and meta-analysis. PLoS One 14:e0219600. https://doi.org/10.1371/journal.pome.0219600
Ching TYC, Dillon H, Leigh G, Cupples L (2018) Learning from the longitudinal outcomes of children with hearing impairment (LOCHI) study: Summary of 5-year findings and implications. Int J Audiol 57:S105–S111
Holte L, Walker E, Oleson J, Spratford M, Moeller MP, Roush P et al (2012) Factors influencing follow-up to newborn hearing screening for infants who are hard of hearing. Am J Audiol 21:163–175
Neumann K, Euler HA, Chadha S, White KR, The International Newborn and Infant Hearing Screening (NIHS) Group (2020) A survey on the global status of newborn and infant hearing screening. J Early Hear Detect Interv 5:63–84
Bani NH, Samsudin MD, Bujnag R, Wan Husain WS, Md Yusoff Y, Che Abdullah MR et al (2019) Universal neonatal hearing screening in Malaysia: A report. Int J Allied Health Sci 3:543
Mukari SZ, Tan KY, Abdullah A (2006) A pilot project on hospital-based universal newborn hearing screening: lessons learned. Int J Pediatr Otorhinolaryngol 70:843–851
Abdullah A, Mohd Yusof Senusi MH, Awang MA, Abdul Ghani J, Michael Thomas A, Liyab B et al (2006) Newborn hearing screening: experience in a Malaysian hospital. Singap Med J 47:60–64
Joint Committee on Infant Hearing (JCIH) (2019) Year 2019 position statement: principles and guidelines for early hearing detection and intervention programs. J Early Detect Interv 4:1–44
Sun X, Shen X, Zakus D, Lv J, Xu Z, Wu H et al (2009) Development of an effective public health screening program to assess hearing disabilities among newborns in Shanghai: a prospective study. World Health Popul 11:14–23
Low WK, Pang KY, Ho LY, Lim SB, Joseph R (2005) Universal newborn hearing screening in Singapore: the need, implementation, and challenges. Ann Acad Med Singap 34:301–306
Van Dyak M, Swanepoel DW, Hall JW (2015) Outcomes with OAE and AABR screening in the first 48 hours – implications for newborn hearing screening in developing countries. Int J Pediatr Otorhinolaryngol 79:1034–1040
Abdullah A, Wan Hashim WF, Awang MA, Han YS, Abdul Ghani J, Said R et al (2008) Benefit and pitfalls of newborn hearing screening. Med J Malaysia 63:293–297
Caluraud S, Marcolla-Bouchtemble A, de Barros A, Moreau-Lenior F, de Sevin E, Rerolle S et al (2015) Newborn hearing screening: analysis and outcomes after 100,000 births in Upper-Normandy French region. Int J Pediatr Otorhinolaryngol 79:829–833
Pitathawatchai P, Khaimook W, Kirtsreesakul V (2019) Pilot implementation of newborn hearing screening program at four hospitals in southern Thailand. Bull World Health Organ 97:663–671
Huang H, Chiang S, Shiau Y, Yeh WY, Ho HC, Wang L et al (2013) The universal newborn hearing screening program of Taipei City. Int J Pediatr Otorhinolaryngol 77:1734–1737
Capua BD, Costantini D, Martufi C, Latini G, Centile M, Felice CD (2007) Universal newborn hearing screening: the Siena (Italy) experience on 19,7000 newborns. Early Hum Dev 83:601–606
Friderichs N, Swanepoel D, Hall JW (2012) Efficacy of a community-based infant hearing screening program utilizing existing clinic personnel in Western Cape, South Africa. Int J Pediatr Otorhinolaryngol 76:552–559
Walsh M, Redshaw E, Crossley E, Philips C (2015) Identifying the optimal age to perform newborn screening for hearing loss in Uganda. Ann Med Health Sci Res 5:403–408
Lupoli LDM, Garcia L, Anastasio ART, Fontana AC (2013) Time after birth in relation to failure rate in newborn hearing screening. Int J Pediatr Otorhinolaryngol 77:932–935
Kumari A, Rangasayee R (2016) Transient evoked otoacoustic emission in neonates with and without vernix. Int J Sci Res Publ 6:745–751
Clarke P, Iqbal M, Mitchell SA (2003) Comparison of transient-evoked otoacoustic emissions and automated auditory brainstem response for pre-discharge newborn hearing screening. Int J Audiol 42:443–447
Wenjin W, Xiangrong T, Yun L, Jingrong L, Jianyong C, Xueling W et al (2017) Neonatal hearing screening in remote areas of China: a comparison between rural and urban populations. J Int Med Res 46:637–651
Tatli MM, Serbetcioglu MB, Duman N, Kumral A, Kirkim G, Ogun B et al (2007) Feasibility of neonatal hearing screening program with two-stage transient otoacoustic emissions in Turkey. Pediatr Int 49:161–166
Bussé AML, Qirjazi B, Goedegebure A, Toll M, Hoeve HL, Toci E et al (2020) Implementation of a neonatal hearing screening program in three provinces in Albania. Int J Pediatr Otorhinolaryngol 132:110039
Swanepoel DW, Louw B, Hugo R (2007) A novel service delivery model for infant hearing screening in developing countries. Int J Audiol 46:321–327
Brockow I, Sohl K, Nennstiel U (2018) Newborn hearing screening in Bavaria – Is it possible to reach the quality parameters? Int J Neonatal Screen 4:26
Lieu JE (2004) Speech-language and educational consequences of unilateral hearing loss in children. Arch Otolaryngol Head Neck Surg 130:524–530
Acknowledgements
The authors thank the HCTM UNHS team for their assistance and support throughout this study
Funding
There are no financial conflicts of interest to disclose.
Author information
Authors and Affiliations
Contributions
RM contributed to the study design, supervision, analyses, and critical revision of the draft. KR participated in the data collection, analysis, and drafting the manuscript. AA contributed to supervision and critical revision of the draft. All authors have read and approve the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Research Ethics Committee of Universiti Kebangsaan Malaysia (UKM PPI/111/8/JEP-2021-041). The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki. Informed written consent was obtained from all participants in the study. For subjects who were under 16 years, informed written consent for participation in the study was obtained from their parents or legal guardians.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mazlan, R., Raman, K. & Abdullah, A. A 10-year retrospective analysis of newborn hearing screening in a tertiary hospital in Malaysia. Egypt J Otolaryngol 38, 135 (2022). https://doi.org/10.1186/s43163-022-00331-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00331-w