Abstract
Background
COVID-19-related olfactory dysfunction is an emerging problem with a significant impact on the quality of life of affected individuals. Different lines of treatment have been used with varying results. This study aimed to assess the potential therapeutic effect of PRP in the treatment of post-COVID olfactory dysfunction. This work aimed to assess the potential therapeutic effect of platelet-rich plasma (PRP) in treating post-COVID-19 parosmia. A pilot study was conducted on 60 patients with post-COVID parosmia without responding to a 3-month course of olfactory training, topical corticosteroids, omega-three, vitamin B12, and zinc supplementation. The patients were distributed randomly and equally among 2 groups. The case group was subjected to three PRP injections in the olfactory cleft at 3 weeks intervals. The control group continued the pre-study treatment protocol for 6 weeks. The degree of parosmia was assessed before and after treatment subjectively using a visual analog scale (VAS) from 0 to 10. Reaching 0–1 on the visual analog scale was a complete improvement. The primary outcome was assessing the post-treatment score for parosmia 1 month after the third injection in the case group. The second outcome was the comparison between both groups regarding the degree of improvement 1 month after cessation of treatment.
Results
There was a highly significant improvement in VAS for parosmia (p < 0.00001) in the case group and a significant improvement in VAS for parosmia in the control group (p = P = 0.00148). There was a significant difference between both groups regarding the degree of improvement favoring the case group (p = 0.002).
Conclusion
Platelet-rich plasma injection in the olfactory cleft offers a therapeutic option for treating patients with post-COVID-19 olfactory parosmia who failed to respond to traditional conservative treatment.
Similar content being viewed by others
Background
Olfactory dysfunction caused by COVID-19 is characterized by a fast onset of impairment, which may come with or without other symptoms. Italian COVID-19 hospitalized patients of young age and female gender were more likely to have a compromised sense of taste or smell [1]. Unpublished studies and personal accounts suggest that olfactory issues can be resolved in 2 weeks or less. However, it is unknown how many people would experience chronic postinfectious olfactory impairment due to a lack of long-term follow-up [2].
Angiotensin-converting enzyme 2 receptor, a necessary component for SARS-CoV-2 entry, is abundant in nasal epithelial cells, making coronaviruses one of several pathogenic organisms that can cause postinfectious olfactory dysfunction [3]. If cells in the olfactory neuroepithelium are disrupted, inflammatory changes in the olfactory neuroepithelium may impact olfactory receptor neuron function, encourage more olfactory receptor neuron damage, and restrict subsequent neurogenesis. Olfactory impairment from such changes may be temporary or persistent [4].
In patients with olfactory dysfunction, the olfactory neuroepithelium and olfactory filae, peripheral nerve fibers that cross the cribriform plate and enter the nasal cavity, may be exploited as therapeutic targets since they can regenerate. An autologous biologic product called platelet-rich plasma (PRP) is created from freshly drawn whole blood with a high platelet content. One of PRP’s anti-inflammatory and pro-regenerative properties is the upregulation of growth factors such as transforming growth factor, vascular endothelial growth factor, epidermal growth factor, and insulin-like growth factor. It has been used as a safe and efficient treatment for inflammation, wound healing, and peripheral neuropathies in various therapeutic settings [5]. PRP has been demonstrated to help with neurodegeneration and axon regeneration. GFs and stem cells have been used in animal experiments to treat anosmia and regenerate olfactory neurons when neurodegenerative processes are present [6, 7]. Due to the high concentration of GFs and neurotrophic factors in PRP, several authors have examined PRP’s effectiveness in treating anosmia through its role in accelerating the healing process in animal models [8]. This study aimed to assess the potential therapeutic effect of PRP in the treatment of post-COVID parosmia.
Patients and methods
The current study was a pilot study conducted on 60 patients with post-COVID parosmia recruited from the outpatient clinic of the Otorhinolaryngology Department, [Removed for blinding] during the period from December 2020 to December 2021. Approval from the institutional review board was obtained, and informed written consent was taken from every patient before participation in the study.
The inclusion criteria of this study included an age of more than 18 years with a history of COVID-19 infection as confirmed by a polymerase chain reaction (PCR) test more than 3 months before. Patients in the study should have olfactory dysfunction in the form of parosmia without a response to a 3-month course of olfactory training, topical corticosteroids, omega-three, vitamin B12, and zinc supplementation. Patients with active COVID-19 infection, patients with previous nasal surgery, and patients with bleeding tendencies were excluded from the study.
The study patients were randomly distributed among two groups using the block randomization method. The case group included 30 patients subjected to three PRP injections in the olfactory cleft at 3 weeks intervals. The control group included 30 patients who continued the pre-study treatment protocol, including olfactory training, topical corticosteroids, omega-three, vitamin B12, and zinc supplementation for 6 weeks.
The study patients were subjected to an assessment protocol, including history taking to assess the inclusion and exclusion criteria. Complete otorhinolaryngology examination, including endoscopic examination of the nose and computed tomography of the nose and paranasal sinuses, were performed to exclude other intranasal pathologies. The degree of parosmia was assessed subjectively using a visual analog scale from 0 to 10. Reaching 0–1 on the visual analog scale was a complete improvement. The assessment of the degree of parosmia using VAS will be repeated 1 month after cessation of the treatment in each group.
Platelet-rich plasma preparation
The procedures outlined by Perez et al. [9] were performed on each patient. [1] After sterilization, 8.5 ml of whole blood was aspirated by venipuncture from the cubital vein using a wide-pore canula, and 1.5 ml of acid citrate dextrose was added (ACD). [2] Neither before nor during platelet separation was the blood cooled. [3] To provide a “soft” spin, the collected tubes on the ACD were centrifuged at 800 rpm for 10 min. [4] Sterile syringes were used to transfer platelet-containing supernatant plasma into another clean, sterile tube (without anticoagulant). [5] To obtain a platelet concentrate, the tubes holding the separated plasma were centrifuged at a higher speed of 2000 rpm (a hard spin). The lower 1/3 of the tubes contained PRP, whereas the top 2/3 contained platelet-poor plasma (PPP). Platelet pellets develop at the tube’s bottom. [6] Platelet pellets were suspended in a minimum amount of plasma (1–2 ml) by gently shaking the tube after PPP was extracted using sterile syringes. [7] To ensure adequate platelet yielding, the platelet count was assessed following PRP preparation.
PRP Administration
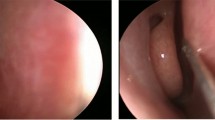
The PRP administration started with applying a local anesthetic solution prepared by mixing decongestant nasal drops with Emla® 5% and 10% Xylocaine spray and inserted in the nose on cotton pieces for 30 min. With the aid of a nasal endoscope, PRP is injected into the olfactory region approximately every 1 cm2 using a 1-ml syringe and 30-G needle.
Outcomes
The study’s primary outcome was assessing the post-treatment score for parosmia 1 month after the third injection in the case group. The second outcome was the comparison between both groups regarding the degree of improvement 1 month after cessation of treatment.
Statistical analysis
Data were collected, tabulated, and statistically analyzed using an IBM personal computer with Statistical Package of Social Science (SPSS) version 22, IBM Corp, Armonk, NY, USA. Descriptive statistics for quantitative data were presented as mean (¯X) and standard deviation (SD). Qualitative data were presented as numbers and percentages (%). Data turned up to be non-normally distributed according to the Kolmogorov–Smirnov test. Mann–Whitney U test was used to compare the quantitative data of both groups. The chi-square test (χ2) was used to study the association between two qualitative variables. Wilcoxon sign rank test was used to compare both groups' pretreatment and post-treatment scores. A two-sided p-value of (≤ 0.05) was considered statistically significant.
Results
The study included 60 patients with post-COVID-19 parosmia distributed as two similar case and control groups. There was no statically significant difference between the two groups regarding age, gender, and VAS for parosmia (p = 0.303, 0.584, and 0.484, respectively) (Table 1).
There was a highly significant improvement in VAS for parosmia (p < 0.00001) in the case group and a significant improvement in VAS for parosmia in the control group (p = P = 0.00148) (Table 2). There was a significant difference between both groups regarding the degree of improvement favoring the case group (p = 0.002) (Table 3).
Discussion
The pathophysiology of COVID-19-induced olfactory impairment has been explained by three theories, including the following: [1] mechanical obstruction brought on by inflammation around the olfactory cleft, which prevents odorants from binding to olfactory receptors [10]; [2] infection of ACE-2 expressing supporting cells, particularly the sustentacular cells of the olfactory epithelium [11]; and [3] direct invasion of olfactory neurons by SARS-COV-2 which prevents the olfactory nerve transmission [12]. Based on the second and third hypotheses, platelet-rich plasma might be a viable approach for treating refractory olfactory impairment.
The basal cells that make up the olfactory epithelium’s basal layer are capable of regeneration [13]. Progenitor cells come in two varieties: globose basal cells (GBC) and horizontal basal cells (HBC) (GBC). GBCs are constantly active and aid in the regeneration of olfactory epithelium cells, whereas HBCs are typically inactive and multiply after lesions. Therefore, activating HBC should aid in improving the performance of the olfactory system [14,15,16,17,18]. In recent years, several studies have been conducted to assess the use of growth factors for activating HBCs in the olfactory epithelium. By triggering olfactory nerve regeneration, statins, for instance, improved degenerative anosmia. Reduced inflammation and the activation of genes linked to cell growth and neurogenesis, which led to cell proliferation and neuroregeneration, were the two ways the olfactory epithelium improved. Basic fibroblast growth factor (bFGF) intranasal treatment has been advantageous. bFGF is a multifunctional growth factor that prevents the death of nerve cells and encourages neuronal sprouting, which might lead to the regeneration of the olfactory epithelium. PRP contains large amounts of platelet-derived growth factor (PDGF), insulin-like growth factor (IGF), neurotrophin-3, angiopoietin-1, and other GFs and neurotropic factors. Its administration is therefore anticipated to have a therapeutic and neuro-regenerative effect, and it may be used as a stimulant of basal cell regeneration in treating anosmia [19,20,21,22,23]. Earlier studies have shown that PRP may activate and create new olfactory system receptors [8].
Platelet-rich plasma has been shown to have neuro-regenerative properties in both peripheral and central nervous system injuries. PRP promotes axon regeneration and recovery of neurological functions after injury of the peripheral nerves through three mechanisms: [1] transform the fibrin within the nerve gap from a passive supporter to an active promoter of nerve axon regeneration [24, 25], [2] direct promotion of nerve axon regeneration [26], [3] promote raging the Schwann cells of the central and distal segments of the nerve to proliferate and upregulate their synthesis and release of neurotrophic and other growth factors that act synchronously with platelet-released factors to promote axon regeneration [27,28,29], and [4] enhance mesenchymal stem cells differentiation into Schwann cells and release of axon regeneration-promoting factors [30,31,32,33].
PRP enhances the central nervous system’s axons regeneration. In organ culture, peripheral axons transform into spinal cord tissue, which would not occur naturally [34]. IGF-1 and VEGF activities play a part in this effect [34]. Thus, PRP can potentially promote axon regeneration and neurological recovery following spinal cord injury. It may also be a therapeutic approach for CNS diseases like traumatic brain injury, autoimmune diseases, and neurodegenerative disorders like Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis [35].
In the current study, there was a highly significant improvement of post-COVID olfactory parosmia following three three-weekly PRP injections in the olfactory cleft with a significant difference compared with the control group favoring the case group. Reviewing the literature, some authors have assessed the role of platelet-rich plasma in treating anosmia without specification of post-COVID olfactory dysfunction. Five patients with anosmia received platelet-rich plasma injections in a study by Mavrogeni et al. [36]. Four patients reported that “their smell came back” after the third and, ultimately, the fourth therapy. In contrast, the last patient claimed he could smell “a lot, but not everything.” The authors claimed that administering platelet-rich plasma to the olfactory area would be a promising, last-ditch treatment for total anosmia. In a pilot study, Yan et al. [37] examined the effectiveness of platelet-rich plasma in the treatment of olfactory dysfunction in seven patients who had an olfactory loss that had lasted longer than 6 months, showed no signs of sinonasal inflammatory disease, and did not improve with olfactory training or topical budesonide rinses. They discovered that all patients initially experienced a subjective improvement in smell following injection but that this improvement quickly stabilized. Two patients with functional anosmia did not significantly improve 3 months after treatment. At the 3-month follow-up, five patients with hyposmia exhibited improvement, with 60% achieving normosmia. Forty-eight anosmia patients with sinonasal polyposis participated in randomized controlled research by Goljanian Tabrizi et al. [38] to evaluate the effectiveness of platelet-rich plasma as an adjuvant therapy to endoscopic sinus surgery. Their research found that PRP injection had no immediate impact on patients with sinonasal polyposis’ ability to regain their olfactory function. Eighty patients with various anosmia causes participated in a prospective trial by Aboelmagd et al. [39] utilizing platelet-rich plasma. The authors found that whereas 34 out of 80 patients (42.5%) exhibited no improvement, 46 out of 80 patients (57.5%) said that “their smell came back.” All patients with idiopathic anosmia showed improvement, although there was no statistically significant difference between the patient and control groups.
The limitations of our study included the lack of objective assessment of olfactory functions using electroolfactogram due to its nonavailability. Although the validated tools for olfactory assessment like the University of Pennsylvania Identification test or Sniffin stick test have been widely used for olfactory assessment in various studies, they presented a challenge in assessing parosmia cases due to the variation of the distorted smells between different parosmia patients. So, the authors used a visual analog scale to assess the magnitude of the problem as described by the patients. The power of this study lies in its role in the primary evaluation of platelet-rich plasma as a treatment for a significant problem affecting the quality of life of a considerable number of patients reaching up to emaciation due to the perceived bad odors of many dietary products.
Conclusion
Platelet-rich plasma injection in the olfactory cleft offers a therapeutic option for treating patients with post-COVID-19 olfactory parosmias who failed to respond to traditional conservative treatment. Further larger studies are needed to confirm the findings of this study with emphasis on the long-term results of this treatment line.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACD:
-
Acid citrate dextrose
- CNS:
-
Central nervous system
- COVID-19:
-
Coronavirus disease of 2019
- GBC:
-
Globose basal cells
- HBC:
-
Horizontal basal cells
- IGF:
-
Insulin-like growth factor
- PCR:
-
Polymerase chain reaction
- PPP:
-
Platelet-poor plasma
- PRP:
-
Platelet-rich plasma
- SARS:
-
Severe acute respiratory distress syndrome
- VAS:
-
Visual analog scale
References
Giacomelli A, Pezzati L, Conti F et al (2020) Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis 53(9):1689–1699
Whitcroft KL, Hummel T (2020) Olfactory Dysfunction in COVID-19: Diagnosis and Management. JAMA 323(24):2512–2514
Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M et al (2020) SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med 26(5):681–687
Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S (2008) Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol 82(15):7264–7275
Yan CH, Mundy DC, Patel ZM (2020) The use of platelet-rich plasma in treatment of olfactory dysfunction: A pilot study. Laryngoscope Investig Otolaryngol 5(2):187–193
Lee CH, Jeon SW, Seo BS, Mo JH, Jeon EH, Choi AR et al (2010) Transplantation of neural stem cells in anosmic mice. Clin Exp Otorhinolaryngol 3(2):84
Nota J, Takahashi H, Hakuba N, Hato N, Gyo K (2013) Treatment of Neural Anosmia by Topical Application of Basic Fibroblast Growth Factor– Gelatin Hydrogel in the Nasal Cavity: An Experimental Study in Mice. JAMA Otolaryngol Head Neck Surg 139(4):396–400
Yasak AG, Yigit O, Araz Server E, DurnaDastan S, Gul M (2018) The effectiveness of platelet-rich plasma in an anosmia-induced mice model. Laryngoscope 128(5):E157–E162
Perez AG, Lana JF, Rodrigues AA, Luzo AC, Belangero WD, Santana MH (2014) Relevant aspects of centrifugation step in the preparation of platelet-rich plasma. ISRN Hematol 2014:176060
Stenner M, Vent J, Hüttenbrink KB, Hummel T, Damm M (2008) Topical therapy in anosmia: relevance of steroid-responsiveness. Laryngoscope 118(9):1681–1686
Butowt R, von Bartheld CS (2020) Anosmia in COVID-19: underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist 11:107385842095690
Gane SB, Kelly C, Hopkins C (2020) Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome Rhinology 58:289–294
Beites CL, Kawauchi S, Crocker CE, Calof AL (2005) Identification and molecular regulation of neural stem cells in the olfactory epithelium. Exp Cell Res 306(2):309–316
Leung CT, Coulombe PA, Reed RR (2007) Contribution of olfactory neural stem cells to tissue maintenance and regeneration. Nat Neurosci 10(6):720
Iwai N, Zhou Z, Roop DR, Behringer RR (2008) Horizontal basal cells are multipotent progenitors in normal and injured adult olfactory epithelium. Stem Cells 26(5):1298–1306
Duggan CD, Ngai J (2007) Scent of a stem cell. Nat Neurosci 10(6):673
Schwob JE, Jang W, Holbrook EH, Lin B, Herrick DB, Peterson JN et al (2017) Stem and progenitor cells of the mammalian olfactory epithelium: Taking poietic license. J Comp Neurol 525(4):1034–1054
Kim HY, Kim JH, Dhong HJ, Kim KR, Chung SK, Chung SC et al (2012) Effects of statins on the recovery of olfactory function in a 3- methylindole–induced anosmia mouse model. Am J Rhinol Allergy 26(2):e81–e84
Farrag TY, Lehar M, Verhaegen P, Carson KA, Byrne PJ (2007) Effect of platelet rich plasma and fibrin sealant on facial nerve regeneration in a rat model. Laryngoscope 117(1):157–165
Oppenheim RW, Qin-Wei Y, Prevette D, Yan Q (1992) Brain-derived neurotrophic factor rescues developing avian motoneurons from cell death. Nature 360(6406):755
Shirley DM, Williams SA, Santos PM (1996) Brain-derived neurotrophic factor and peripheral nerve regeneration: a functional evaluation. Laryngoscope 106(5):629–632
Elgazzar RF, Mutabagani MA, Abdelaal SE, Sadakah AA (2008) Platelet rich plasma may enhance peripheral nerve regeneration after cyanoacrylate reanastomosis: a controlled blind study on rats. Int J Oral Maxillofac Surg 37(8):748–755
Sariguney Y, Yavuzer R, Elmas C, Yenicesu I, Bolay H, Atabay K (2008) Effect of platelet-rich plasma on peripheral nerve regeneration. J Reconstr Microsurg 24(03):159–167
Lee AC, Yu VM, Lowe JB 3rd, Brenner MJ, Hunter DA, Mackinnon SE et al (2003) Controlled release of nerve growth factor enhances sciatic nerve regeneration. Exp Neurol 184:295
Mligiliche NL, Tabata Y, Ide C (1999) Nerve regeneration through biodegradable gelatin conduits in mice. East Afr Med J 76:400
Yu W, Wang J, Yin J (2011) Platelet-rich plasma: a promising product for treatment of peripheral nerve regeneration after nerve injury. Int J Neurosci 121(4):176–180
Ogata T, Yamamoto S, Nakamura K, Tanaka S (2006) Signaling axis in Schwann cell proliferation and differentiation. Mol Neurobiol 33:51
Monje PV, Rendon S, Athauda G, BatesM WPM, Bunge MB (2009) Non-antagonistic relationship between mitogenic factors and cAMP in adult Schwann cell re-differentiation. Glia 57:947
Oya T, Zhao YL, Takagawa K, Kawaguchi M, Shirakawa K, Yamauchi T et al (2002) Platelet-derived growth factor-b expression induced after rat peripheral nerve injuries. Glia 38:303
Tohill M, Mantovani C, Wiberg M, Terenghi G (2004) Rat bone marrow mesenchymal stem cells express glial markers and stimulate nerve regeneration. Neurosci Lett 362:200
Kalbermatten DF, Kingham PJ, Mahay D, Mantovani C, Pettersson J, Raffoul W et al (2008) Fibrin matrix for suspension of regenerative cells in an artificial nerve conduit. J Plast Reconstr Aesthet Surg 61:669
Mantovani C, Terenghi G, Shawcross SG (2012) Isolation of adult stem cells and their differentiation to Schwann cells. Methods Mol Biol 916:47
Tomita K, Madura T, Mantovani C, Terenghi G (2012) Differentiated adipose-derived stem cells promote myelination and enhance functional recovery in a rat model of chronic denervation. J Neurosci Res 90:1392
Takeuchi M, Kamei N, Shinomiya R, Sunagawa T, Suzuki O, Kamoda H et al (2012) Human platelet-rich plasma promotes axon growth in brain-spinal cord coculture. Neuroreport 23:712
Shen YX, Fan ZH, Zhao JG, Zhang P (2009) The application of platelet-rich plasma may be a novel treatment for central nervous system diseases. Med Hypotheses 73:1038
Mavrogeni P, Kanakopoulos A, Maihoub S, Krasznai M, Szirmai A (2017) Anosmia treatment by platelet rich plasma injection. Int Tinnitus J 20(2):102–105
Yan CH, Mundy DC, Patel ZM (2020) The use of platelet-rich plasma in treatment of olfactory dysfunction: A pilot study. Laryngoscope Investig Otolaryngol 5(2):187–193
GoljanianTabrizi A, Asadi M, Mohammadi M, AbediYekta A, Sohrabi M (2021) Efficacy of Platelet-Rich Plasma as an Adjuvant Therapy to Endoscopic Sinus Surgery in Anosmia Patients with Sinonasal Polyposis: A Randomized Controlled Clinical Trial. Med J Islam Repub Iran 35(1):1159–1165
Aboelmagd EA, Mohamed EF, Abdelmegeed EM, Eltahan AA (2021) Platelet-rich plasma in the management of anosmia. EJNSO 7(1):10–19
Acknowledgements
Not applicable
Funding
No funding for this research.
Author information
Authors and Affiliations
Contributions
HA provided the concept and design with the definition of the intellectual content and conducted clinical studies. RE conducted clinical studies, data collection, and manuscript editing. AH conducted clinical studies, data collection, data analysis, and manuscript writing. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the Institutional Review Boards (IRB) of the Menoufia Faculty of Medicine number (6/2022 ENT) and following the Declaration of Helsinki. After an explanation of all aspects of the study and being given the right to withdraw at any time, written consent was taken from all the patients.
Consent for publication
Not applicable.
Competing interests
No potential competing interests relevant to this article were reported for any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abo El Naga, H.A., El Zaiat, R.S. & Hamdan, A.M. The potential therapeutic effect of platelet-rich plasma in the treatment of post-COVID-19 parosmia. Egypt J Otolaryngol 38, 130 (2022). https://doi.org/10.1186/s43163-022-00320-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00320-z