Abstract
Background
Blood eosinophil count is significantly correlated with eosinophil infiltration in the nasal polyps; so, it could be a good marker for the nasal polyp eosinophilic inflammation.
Objective
Assessment of different peripheral eosinophil counts in different nasal polyps grading in allergic rhinitis patients.
Methods
A study was applied to 160 patients with allergic rhinitis (AR). Computed tomography (CT) was done preoperative then nasal polyps grading was assessed by nasal endoscopy. Peripheral eosinophil counts were checked in a blood sample for all patients. Then, a statistical analysis of the data was done.
Results
The study included 160 patients. Within 54 AR patients with no nasal polypi, eosinophil counts ranged between 0.001 × 103 μl and 0.907 × 103 μl with a mean of 0.2399 (SD = 0.2153). While within 106 patients with nasal polyps, eosinophil counts ranged between 0.05 × 103 μl and 14.7 × 103 μl with a mean of 1.6645 (SD = 3.06) with a significant difference (p = 0.0008, t = 3.418). The eosinophil counts were statistically significantly more in advanced grades of the nasal polyps (p < 0.0001, F = 9248).
Conclusion
Measuring peripheral eosinophil counts is simple, low cost, safe, and directly proportionate with different grades of nasal polyps. It can be used as a reliable marker to predict the severity of nasal polyps and consequently predict the prognosis of sinus disease and quality of life.
Similar content being viewed by others
Introduction
Chronic rhinosinusitis (CRS) is the most common chronic inflammatory disease of the upper airway [1].CRS is divided into two types according to the absence or presence of nasal polyps (NPs): CRS without NPs (CRSsNP) and CRS with NPs (CRSwNP) [2].
CRS is divided into two phenotypes according to CT and endoscopy findings: CRSsNP and CRSwNP [3] which are characterized by the presence of nasal polyps, signs and symptoms lasting more than 8–12 weeks [4, 5]. The EPOS2020 steering group classified CRS into primary and secondary and categorized each into diffuse and localized disease depending on the anatomical distribution. Then, primary CRS was classified into type 2 or non-type 2 while localized primary CRS was then subclassified clinically into two phenotypes: isolated sinusitis or allergic fungal rhinosinusitis. For diffuse CRS, the clinical phenotypes are predominantly eCRS and non-eCRS [6]. Immunologically, NPs are divided into three types: type 1, immune response which is common in Asia [7] and characterized by neutrophilic infiltration; type 2, which is characterized mainly by eosinophilic infiltration, and this type is more common in Caucasians [8]; and type 3 immune response is characterized by a high level of the IL-17 cytokine, mixed inflammatory cell pattern, and is associated with frequent asthma exacerbations [9].
CRSwNP affects about 1–4% of the general population and 25–30% of CRS patients [6]. The etiology of NPs is multifactorial: allergy and inflammatory mediators such as eosinophils which contain leukotrienes, eosinophilic cationic protein, major basic protein, platelet-activating factor, eosinophilic peroxidases, and other vasoactive substances that cause mucosal damage. These may play a critical role in the development of nasal polyps [10]. Also, there are non-allergic causes of NPs such as cystic fibrosis [1].
CRSwNP is often characterized by eosinophilic inflammation with increased levels of T helper 2 (Th2) cytokines [11, 12]. Marked eosinophilic tissue infiltration in CRSwNP is frequently associated with extensive sinus disease [11, 13], comorbid asthma, olfactory dysfunction, high recurrence rate after surgery, and less improvement in both disease-specific and general quality of life [14].
CRSwNP is frequently associated with asthma and allergic rhinitis, but the cellular and molecular mechanisms that contribute to the clinical symptoms are not fully understood.
It was found that blood eosinophil count is significantly correlated with eosinophil infiltration in the nasal polyps; the blood eosinophil count could be a good marker for the eosinophilic inflammation of NPs [15], especially when the histopathological assessment is not applicable due to it is not easy to obtain enough polyp tissue by biopsy before surgery [16].
In this study, we used peripheral eosinophilia as a marker for NPs with esinophilic infiltration, but we want to investigate the relation between peripheral eosinophil counts and severity of nasal polyps grades in AR patients and if this will predict the severity of the sinus disease.
Patient and methods
Study design
This study was conducted on 160 patients with allergic rhinitis (as proved by history and skin test) at the otorhinolaryngology department, university hospitals, over a period from January 2020 to January 2021. Informed consent was signed by all enrolled subjects or their relative after an explanation of the research purpose.
The exclusion criteria are patients under 18 years, patients who received steroids therapy or systemic antibiotics 1 month before enrollment in the study, patients with autoimmune disease, patients with recurrent nasal polypi after previous surgery, patients who has allergy elsewhere in the body or on medical treatment for allergy, and patients diagnosed with fungal rhinosinusitis, cystic fibrosis, primary ciliary dyskinesia, inverted papilloma, and any neoplastic lesions.
The following are the investigations:
-
Full ENT examination.
-
History taking.
-
All included patients complained of a symptom of AR: at the clinical visit, the patients gave symptoms of nasal blockage, nasal itching, sneezing, and rhinorrhea.
-
Each patient underwent CT examination of the nasal cavity and sinuses to predict patients with eCRSwNP; according to Lund-Mackay scoring system, Meng et al. [17] found that an optimal cutoff value of > 2.59 for the ethmoid sinus/maxillary sinus (E/M) CT score ratio demonstrated a sensitivity of 94% and a specificity of 90% for eCRSwN.
-
Endoscopic examination to detect different grading of nasal polyps according to the Meltzer Clinical Scoring System [18] is a 0–4 nasal polyp grading system:
-
0 = no polyps
-
1 = polyps confined to the middle meatus
-
2 = multiple polyps occupying the middle meatus
-
3 = polyps extending beyond the middle meatus
-
4 = polyps completely obstructing the nasal cavity
-
Blood samples were taken from every patient who fulfilled the inclusion criteria to detect absolute eosinophil counts.
The patients were compared as regards the demographic features (age and sex), associated anatomical variations and pathology, complications, and recurrence rate.
Statistical methods
All analyses were performed using the Statistical Package for the Social Sciences (SPSS) for Windows, version 15 packed programs. A difference was considered significant at p < 0.05.
Results
One hundred sixty patients were included in the current study and divided into two groups: first group—54 patients without nasal polyps (35 males and 19 females) with age ranging from 18 to 55 years (mean = 39.7 ± 11). Within 54 patients with no nasal polyps, eosinophil count ranged between 0.001 × 103 μl and 0.907 × 103 μl with a mean of 0.2399 (SD = 0.2153).
The second group included 106 patients with nasal polyps (65 males and 41 females); their age ranged between 19 and 76 years (mean = 41.7 ± 14.9), and eosinophil count ranged between 0.05 × 103 μl and 14.7 × 103 μl with a mean of 1.6645 = 3.06 with significant difference between the two groups (p = 0.0008, t = 3.418) (Tables 1 and 2).
In grade 1 (36 patients), eosinophil count ranged between 0.05 × 103 μl and 7.68 × 103 μl with a mean of 0.7 + 1.7. In grade 2 (18 patients), eosinophil count ranged between 0.117 × 103 μl and 10.3 × 103 μl with a mean of 1.4588 + 3.1296. In grade 3 (14 patients), eosinophil count ranged between 0.114 × 103 μl and 0.986 × 103 μl with a mean of 0.553 + 0.3. In grade 4 (38 patients), eosinophil count ranged between 0.132 × 103 μl and 14.7 × 103 μl with a mean of 2.95595 + 3.856 (Table 2).
The difference between grades was found statistically highly significant (p < 0.0001, ANOVA, F= 9248).
Post hoc test: polyp grade1 1 vs grade 2—Diff = 0.7588, 95%CI = − 1.3777 to 2.8953, p = 0.7901; polyp grade 1 vs grade 3—Diff = − 0.1470, 95%CI = − 2.4781 to 2.1841, p = 0.9983; polyp grade 1 vs grade 4—Diff = 95,594.3000, 95%CI = 95,592.5787 to 95,596.0213, p = 0.0000; polyp grade 2 vs grade 3—Diff = − 0.9058, 95%CI = − 3.5431 to 1.7315, p = 0.8064; polyp grade 2 vs grade 4—Diff = 95,593.5412, 95%CI = 95,591.4236 to 95,595.6588, p = 0.0000; and polyp grade 3 vs grade 4—Diff = 95,594.4470, 95%CI = 95,592.1332 to 95,596.7608, p = 0.0000.
Discussion
Fokkens et al. [6] in the European Position Paper (EPOS) published in 2020 described an association between asthma and CRS; eosinophilia and asthma are risk factors for CRSwNP and disease recurrence. Eosinophilia affects the respiratory function and is associated with greater disease severity and recurrence rates [19] and hence severe sinus disease.
About 24 years ago, Hellquist [20] reported that eosinophilic polyps accounted for 86% of all polyps in Sweden. Ishitoya et al. [21] divide CRSwNP into two types, eosinophilic chronic rhinosinusitis (ECRS) and non-ECRS. Ferguson [22] and Orlandi [23] subclassified ECRS into 4 groups: superantigen-induced ECRS, classic allergic fungal rhinosinusitis (AFRS), non-allergic fungal ECRS, and aspirin-exacerbated ECRS. Know the term “eosinophilic CRSwNP” is used rather than ECRS which indicates more tissue eosinophilic infiltration.
Therefore, eosinophils are the most common and important inflammatory cells in the pathogenesis of polyps [24, 25]. To diagnose this type of NPs, tissue biopsy is the gold standard. However, to assess the severity of the sinus disease, diagnosis must occur preoperatively. It is not always easy to take enough biopsies from the nose preoperatively due to poor patient compliance [16], besides taking serial biopsies to diagnose, follow-up, and predict the recurrence is coasty.
In addition, a biopsy cannot be taken after FESS and clearance of sinuses from polyp; so to follow up and to pick up recurrence, more time must pass until polyps appear again to be detected by CT or tissue histopathology.
Several studies proved that peripheral eosinophilia is strongly correlated to tissue infiltration with eosinophils in CRSwNP [21, 26,27,28]. Our results support these studies as we found a positive correlation between peripheral eosinophil counts and the presence of nasal polyps; the eosinophil counts were lower in CRSsNP patients.
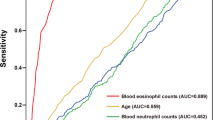
A recent study demonstrated that the specificity of peripheral eosinophils as a predictor for the diagnosis of eCRSwNP was only 75.3% [29]. In this regard, CT has more specificity by using Lund-Mackey scores with a specificity of 90% [17] or Japanese Epidemiological Survey of Refractory Eosinophilic Chronic Rhinosinusitis (JESREC) with a specificity of 66% [30]. In our opinion, specificity of CT could be affected by the improper reading of sinus shadow and whether the patient underwent previous sinus surgery or not. Even if, the specificity of peripheral eosinophilia is quite similar to CT especially when excluding other causes of peripheral eosinophilia.
The blood eosinophil count could be a good marker for the eosinophilic inflammation of NPs. All these data suggested that the occurrence of eosinophilic NPs was closely related to allergy. However, the role of allergy in the pathogenesis of NPs is still controversial. A few studies have questioned the role of allergy in the pathogenesis of NPs. After evaluating 3000 atopic patients, it was found that only 0.5% of patients had NPs [31]. Other reports were also unable to support either a higher incidence of atopy in patients with NPs or a pattern of allergic inflammation in the pathogenesis of NPs [32,33,34]. Thus, the present study requires further validation by studies with a larger sample size. It was also found that eosinophil infiltration was directly correlated with disease severity, since both total and each item’s score were higher in eosinophilic NPs; also, the peripheral eosinophil count was directly proportionate with the severity of nasal polyp grade; the eosinophil counts were high in grade 3 and 4 nasal polyps. Besides, higher Lund-Kennedy and Lund-Mackey scores in eosinophilic NPs were also found. Taken together, these results suggest that eosinophilic NPs predict long disease duration and poor prognosis.
So, eosinophil is part of the nasal polypi disease, and its level significantly increases on increasing polyp grading (severity), so it could be suggested to be a simple easy and available and repeatable indicator for nasal polypi servility and may recurrence and this need to be investigated after nasal surgery for nasal polyposis and in recurrent cases. It could be also used as an indicator of medical treatment efficiency even before polyps appear.
So, a basal level of the patient’s eosinophil should be available on the first visit to reassess. Thus, we in agree with Aslan et al. [35] that peripheral eosinophilia can be used as an easy, safe, and reliable marker to predict disease severity in nasal polyps. So, this investigation is safe, reliable, easily applicable, and cost-effective, and blood samples could be obtained from both outpatient and hospitalized patients and can be done even by a general practitioner to predict the severity of sinus disease preoperative and to follow-up patients postoperative and pickup early recurrence. It is recommended to be investigated on larger series of patients with a longer follow-up period.
Conclusion
Measuring peripheral eosinophil counts is simple, low cost, safe, and directly proportionate with different grades of nasal polyps. It can be used as a reliable marker to predict the severity of nasal polyps and consequently predict the prognosis of sinus disease and quality of life.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CRS:
-
Chronic rhinosinusitits
- CRSsNP:
-
CRS without NPs
- CRSwNP:
-
CRS with NPs
- NPs:
-
Nasal polyps
- Th2T:
-
Helper 2
References
Stevens WW, Schleimer RP, Kern RC (2016) Chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol Pract 4(4):565–572
Fokkens W, Lund V, Mullol J (2007) EP3OS 2007: European Position Paper on rhinosinusitis and nasal polyps 2007. A summary forotorhinolaryngology. Rhinology 45:97–101
Bachert C, Zhang L, Gevaert P (2015) Current and future treatment options for adult chronic rhinosinusitis: focus on nasal polyposis. J Allergy Clin Immunol 136(6):1431–1440
Fokkens WJ, Lund VJ, Mullol J et al (2012) EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50(1):1–12
Orlandi RR, Kingdom TT, Hwang PH et al (2016) International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol 6(Suppl 1):S22–S209
Fokkens WJ, Lund VJ, Hopkins C et al (2020) European Position Paper on chronic rhinosinusitis and nasal polyps 2020. Rhinol Suppl 58:1–464
Dennis SK, Lam K, Luong A (2016) A review of classification schemes for chronic rhinosinusitis with nasal polyposis endotypes. Laryngoscope Investig Otolaryngol 1(5):130–134
Liu JX, Liao B, Yu QH et al (2020) IL-37-Mex3B-TLR3 axis in epithelial cells in eosinophilic chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol 145(1):160–172
Ricciardolo F, Sorbello V, Folino A et al (2017) Identification of IL-17F/frequent exacerbator endotype in asthma. J Allergy Clin Immunol 140(2):395–406
Tosun F, Arslan HH, Karslioglu Y, Deveci MS, Durmaz A (2010) Relationship between postoperative recurrence rate and eosinophil density of nasal polyps. Ann Otol Rhinol Laryngol 119:455–459
Cao PP, Li HB, Wang BF et al (2009) Distinct immunopathologic characteristics of various types of chronic rhinosinusitis in adult Chinese. J Allergy Clin Immunol 124:478–484
Tomassen P, Vandeplas G, Van Zele T et al (2016) Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clin Immunol 137:1449–1456.e4
Kim JW, Hong SL, Kim YK, Lee CH, Min YG, Rhee CS (2007) Histological and immunological features of non-eosinophilic nasal polyps. Otolaryngol Head Neck Surg 137:925–30.9
Avord ID, Brightling CE, Woltmann G, Wardlaw AJ (1999) Non-eosinophilic corticosteroid unresponsive asthma. Lancet 353:2213–4.11
Sun C, Ouyang H, Luo R (2017) Distinct characteristics of nasal polyps with and without eosinophilia. Braz J Otorhinolaryngol 83:66–72
Wang E, Zheng Y, Liu P et al (2014) Eosinophilic chronic rhinosinusitis in East Asians. World J Clin Cases 2:873–882
Meng Y, Lou H, Wang C, Zhang L (2016) Predictive significance of computed tomography in eosinophilic chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol 6:812–819. https://doi.org/10.1002/alr.21749
Meltzer EO, Hamilos DL, Hadley JA et al (2006) Rhinosinusitis: developing guidance for clinical trials. J All Clin Immun 118:17–61
Chen S, Zhou A, Emmanue B, Thomas K, Guiang H (2020) Systematic literature review of the epidemiology and clinical burden of chronic rhinosinusitis with nasal polyposis. Curr Med Res Opin 36(11):1897–1911
Hellquist HB (1996) Nasal polyps update. Histopathology. Allergy Asthma Proc 17:237–242
Ishitoya J, Sakuma Y, Tsukuda M (2010) Eosinophilic chronic rhinosinusitis in Japan. Allergol Int 59:239–245
Ferguson BJ (2004) Categorization of eosinophilic chronic rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg 12:237–242
Ferguson BJ, Orlandi RR (2006) Chronic hypertrophic rhinosinusitis and nasal polyposis. In: Bailey BJ, Johnson JT, Newlands SD (eds) Head and neck surgery–otolaryngology. Lippincott Williams & Wilkins, Philadelphia, pp 394–399
Bernstein J (2001) Nasal polyps. In: Kennedy DW, Bolger WE, Zinreich SJ (eds) Diseases of the sinuses: diagnosis and management. B.C. Decker Inc., London, pp 69–75
Armengot M, Garin L, Carda C (2009) Eosinophil degranulation patterns in nasal polyposis: an ultrastructural study. Am J Rhinol Allergy 23:466–470
Kim JW, Hong SL, Kin YK et al (2007) Histological and immunological features of non-eosinophilic nasal polyps. Otolaryngol Head Neck Surg 137:925–930
Kountakis SE, Arango P, Bradley D, Wade ZK, Borish L (2004) Molecular and cellular staging for the severity of chronic rhinosinusitis. Laryngoscope 114:1895–1905
Ikeda K, Shiozawa A, Ono N et al (2013) Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope 123:E1–E9
Hu Y, Cao P, Liang G et al (2012) Diagnostic significance of blood eosinophil count in eosinophilic chronic rhinosinusitis with nasal polyps in Chinese adults. Laryngoscope 122:498–503
Lou H, Zhang N, Bachert C, Zhang L (2018) Highlights of eosinophilic chronic rhinosinusitis with nasal polyps in definition, prognosis, and advancement. Int Forum Allergy Rhinol 8:1218–1225
Caplin I, Haynes JT, Spahn J (1971) Are nasal polyps an allergic phenomenon? Ann Allergy 29:631–634
Drake-Lee AS (1989) Nasal polyps. In: Mackay IS (ed) Rhinitis: mechanism and management. Royal Society of Medicine, London, pp 141–152
Bachert C, Gevaert P, Holtappels G, van Cauwenberge P (2002) Media-tors in nasal polyposis. Curr Allergy Asthma Rep 2:481–7.24
Baroody FM, Hughes CA, McDowell P, Hruban R, Zinreich SJ, Naclerio RM (1995) Eosinophilia in chronic childhood sinusitis. ArchOtolaryngol Head Neck Surg 121:1396–1402
Aslan F, Altun E, Paksoy S, Turan G (2017) Could Eosinophilia predict clinical severity in nasal polyps? Multidiscip Respir Med 12(21):1–5
Acknowledgements
Not applicable.
Funding
None; the authors declare no financial support or interest in this study.
Author information
Authors and Affiliations
Contributions
MWE suggested and modified the idea, reviewed the literature, designed the study and concept, revised the results, did the statistical analysis, interpreted the data, tabulate the interpreted data, wrote and revised the article, and approved the final manuscript to be published. MAM developed the idea, collected the data, tabulated the data, kept the patient records, analyzed the data, revised the article, and contributed to the final approval of the article. EH developed the research idea, reviewed the literature, contributed to the data interpretation, revised the manuscript, and contributed to the final approval of the article. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the study participants, and Zagazig University IRB approved the study proposal (IRB 117-1-18).
Consent for publication
Not applicable (no images or videos related to participants).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Anwar, M.W., Mobasher, M.A. & Hindawy, E. Assessment of the blood eosinophil count in different grades of nasal polyps. Egypt J Otolaryngol 38, 82 (2022). https://doi.org/10.1186/s43163-022-00276-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00276-0