Abstract
Background
Anomalous left coronary arteries are rare congenital defects. These are often detected incidentally unless they have a malignant course whereby patients present with acute coronary syndromes. We describe a rare presentation of a benign variant of this pathology and a proposed diagnostic and management plan.
Case presentation
A 41-year-old female was admitted following an out-of-hospital cardiac arrest. Cardiac imaging demonstrated an anomalous left main coronary artery arising from a single right coronary ostium with a trans-septal course and associated ischaemic changes on functional testing. Given her clinical presentation, she underwent successful left coronary reimplantation surgery.
Conclusions
This case highlights that even supposedly ‘benign’ variants can have malignant outcomes and that functional testing can be useful in further risk-stratifying anomalous coronary anatomy. Surgical reimplantation is a feasible and effective treatment for achieving optimal long-term results
Similar content being viewed by others
Background
Coronary artery anomalies are relatively common, seen in 1% to 5% of the population [1, 2]. Although most lesions are detected incidentally, approximately 20% have the potential to cause coronary ischaemia and infarction [1]. The anomalous left coronary artery that arises from the right coronary artery is particularly rare with a prevalence of 0.02% to 0.05% [3]. This case report illustrates an unusual presentation of a benign variant of this pathology.
Case presentation
A 41-year-old female was admitted following an out-of-hospital cardiac arrest. She was found collapsed by family members who immediately initiated cardiopulmonary resuscitation. Paramedics arrived within 10 min, and she received two direct current shocks for a ventricular fibrillation rhythm with subsequent return of spontaneous circulation. On arrival to the emergency department, she was intubated and admitted into the intensive care unit. Cardiovascular, respiratory, and abdominal examination revealed no abnormalities.
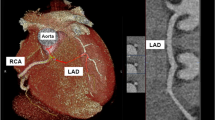
An electrocardiogram after return of circulation demonstrated no abnormalities and her peak high-sensitivity troponin I level was modestly elevated at 659 ng/L (normal range <16 ng/L). A transthoracic echocardiogram illustrated a preserved ventricular function with no valvular abnormalities. Invasive coronary angiography (Fig. 1A, B) revealed an aberrant origin of the left main coronary artery (LMCA) from the right coronary cusp, sharing the same coronary ostia as the right coronary artery. The left anterior descending coronary (LAD) artery was of relatively small calibre with no evidence of obstructive coronary artery disease (CAD). Coronary computed tomography angiography (CTA) was performed to further delineate the course of the anomalous LMCA and identify any malignant features. The CTA demonstrated that the aberrant LMCA was extra-mural and originated from the right coronary ostium. The LMCA had a transeptal/subpulmonic course between the right ventricular outflow tract (RVOT) and the aortic root (Fig. 2A, B). There was a long segment of mild luminal narrowing as the LMCA passed between the aorta and the RVOT. A dipyridamole myocardial perfusion study was undertaken to assess the functional significance of the anomalous coronary artery. Significant 3-mm ST-segment depression in the anteroseptal and inferolateral leads was present during and after the study with symptoms of chest tightness that self-resolved. There was a small reversible defect in the mid to basal anteroseptal wall, with an equivocal defect in the lateral wall.
Invasive coronary angiography (preoperative). A A cranial left anterior oblique projection. B A cranial right anterior oblique projection. Both images demonstrate the right coronary artery (green arrows) and the anomalous left main coronary (red arrows) before it bifurcates into the relatively small calibre left anterior descending (LAD) (blue arrow) and left circumflex arteries (white arrows)
Pre- and post-operative coronary CTA with 3D volume-rendered images. Coronary computed tomography angiography (CTA) demonstrates the single right coronary ostium (yellow arrow) giving rise to the left (red arrow) and right (green arrow) coronary arteries (A and B). Coronary computed tomography angiography (CTA) images postoperatively show the new origin of the left coronary artery (red arrows) which is now more posterior and inferior on the aortic sinus (C and D). The dominant right coronary artery (green arrows) is also demonstrated
Following discussion at a multi-disciplinary heart team meeting, the cardiothoracic surgical team were consulted for consideration of reimplantation of the anomalous coronary artery. Given the risk of further adverse cardiac events, inpatient surgery was performed. The procedure was carried out through a standard median sternotomy, cardiopulmonary bypass was instituted and a hyperkalemic cardioplegia solution was administered to achieve myocardial protection. As expected, the aberrant LMCA originated from the single coronary ostia in the right aortic sinus. The LMCA traversed inferiorly and adjacent to the right coronary cusp towards the RVOT and under the pulmonary valve. The aorta was transected and the LMCA was mobilised proximally and throughout its subpulmonic course. Once the LMCA was mobilised, it was divided at the single right coronary ostia. On inspection, there was an obvious region of narrowed tissue at the origin of the LMCA which had the appearance of a slit-like ostium. The right coronary ostial side was oversewn with a continuous suture.
A suitable site in the posterior and basal aspect of the right coronary sinus was then identified for reimplantation of the LMCA. It was anastomosed in an end-to-side fashion and easily accepted a 3-mm probe. The aorta was then repaired, and the patient was easily weaned off cardiopulmonary bypass and the chest closed in a routine manner. The patient had an uncomplicated post-operative course and was discharged home 4 days after her procedure.
Follow up
At 3-month post-operative follow-up, the patient was stable with no further symptoms. Post-operative coronary CTA demonstrated that the reimplanted LMCA arose from the left anterolateral aspect of the right coronary cusp, approximately 1 cm from the origin of the right coronary ostia (Fig. 2C, D) with no evidence of anastomotic kink or luminal narrowing. Repeat myocardial perfusion scan demonstrated interval resolution of previously demonstrated perfusion defect and ischaemic ECG changes.
Conclusions
Anomalous coronary arteries can take five potential paths. These include (1) prepulmonic, anterior to the right ventricular outflow tract; (2) retroaortic, posterior to the aortic root; (3) transeptal, through the proximal interventricular septum; (4) interarterial, between the aorta and pulmonary artery; and (5) retrocardiac, behind the mitral and tricuspid valves in the posterior atrioventricular groove [4]. Other associated abnormalities include an intramural course (within the tunica media of the aortic wall) and an ostial stenosis of the anomalous coronary artery [1]. The current gold standard for diagnosis of coronary anomalies is coronary CTA [5].
High-risk features of anomalous coronary arteries include interarterial course, ostial stenosis, slit-like ostium, intramural course, acute angle take off and elliptical vessel shape. Underlying mechanisms for the malignant consequences are usually a result of decreased diastolic filling time and tachycardia associated with physical exercise [2].
Our patient had a transeptal or subpulmonic course of the left coronary artery with an ostial stenosis due to a slit-like ostium. Traditionally, a transeptal/subpulmonic course is not anatomically classified as malignant; however, given the slit-like ostium and dramatic clinical presentation with cardiac arrest, we had a high index of suspicion. The presence of ischaemia on myocardial perfusion imaging provided evidence that the coronary anomaly identified in this patient was likely relevant to her clinical presentation and therefore surgical reimplantation was performed. Given her young age, surgical reimplantation as opposed to percutaneous coronary intervention or coronary bypass was most appropriate to allow for optimal long-term outcomes.
The left coronary artery arising from a single right coronary ostium with a trans-septal course is a rare anomaly which is typically classified as benign. This case highlights that even supposedly ‘benign’ variants can have malignant outcomes and that functional testing can be useful for further risk-stratifying anomalous coronary anatomy. Surgical reimplantation is a feasible and effective treatment for achieving optimal long-term results.
Availability of data and materials
Not applicable.
Abbreviations
- CTA:
-
Computed tomography angiography
- LAD:
-
Left anterior descending (artery)
- LMCA:
-
Left main coronary artery
- RVOT:
-
Right ventricular outflow tract
- RCA:
-
Right coronary artery
References
Kouchoukos N, Blackstone EH, Hanley FL, Kirklin JK (2013) Cardiac Surgery. Elsevier Inc, Philadelphia
Angelini P (2007) Coronary artery anomalies: an entity in search of an identity. Circulation 115:1296–1305
Villa AD, Sammut E, Nair A, Rajani R, Bonamini R, Chiribiri A (2016) Coronary artery anomalies overview: The normal and the abnormal. World J Radiol 8:537–555
Angelini P (2002) Coronary artery anomalies--current clinical issues: definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J 29:271–278 Young PM, Gerber TC, Williamson EE, Julsrud PR, Herfkens RJ. 2011. Cardiac imaging: Part 2, normal, variant, and anomalous configurations of the coronary vasculature. AJR Am J Roentgenol 197:816-26
Ashrafpoor G, Danchin N, Houyel L, Ramadan R, Belli E, Paul JF (2015) Anatomical criteria of malignancy by computed tomography angiography in patients with anomalous coronary arteries with an interarterial course. Eur Radiol 25:760–766
Acknowledgements
Not applicable.
Funding
No funding was received for this case report.
Author information
Authors and Affiliations
Contributions
UA was involved in the care of this patient preoperatively, intraoperatively, and postoperatively. UA was the major contributor to the initial draft and writing. AG was also involved in the care of this patient and critically reviewed the article. JO provided the CT and angiographic image for this case report. RS was involved in the care of this patient preoperatively and proofread the article. DA was the primary surgeon and critically revised the article. GD and AI were involved in the patient’s care preoperatively and critically revised the article. The author(s) read approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient for this case report.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report including the patients angiographic and CT images.
Competing interests
Dr Ihdayhid has received consulting honorarium from Boston Scientific and Artrya. The remaining authors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, U.S., Geldenhuys, A., Otto, J. et al. Anomalous left coronary artery presenting with out-of-hospital cardiac arrest: a malignant outcome for a ‘benign’ variant. Egypt J Intern Med 34, 89 (2022). https://doi.org/10.1186/s43162-022-00182-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-022-00182-0