Abstract
Background
Literatures revealed syndrome of inappropriate antidiuretic hormone (SIADH) as the most common mechanism of hyponatremia in COVID-19. However, it is important to rule out other etiologies of hyponatremia.
Methods
This is a case series, retrospective study. Four patients were reviewed from the Mesaieed Hospital, Hamad Medical Corporation, Qatar. The patients were admitted during the second wave of pandemic because of mild to moderate COVID pneumonia. The patients received medications according to the protocol; after few days of treatment, their blood laboratory results showed hyponatremia; as compared to the initial readings, hyponatremia workup excluded SIADH. History revealed that the patients were drinking large amounts of water, around 4–5 L/day, due of certain reasons: one patient had dysgeusia, and the other three patients thought that excessive drinking of water is beneficial for COVID-19 infection.
Results
The hyponatremia level was less than 135 mmol/L, other laboratory tests excluded SIADH, and the provisional diagnosis was dilutional hyponatremia. Male/female ratio was 3/1, age from 29- to 45-year-old patients with no associated comorbidities. Fluid restriction up to 1.5 L/day showed dramatic improvement of their sodium blood level. The patients are discharged in a stable condition.
Conclusions
In COVID-19 patients, hyponatremia not only is secondary to SIADH but can also be due to other etiologies. Hyponatremia can be induced by excessive water drinking and considered an extremely rare reported cases.
Similar content being viewed by others
Background
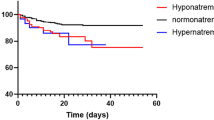
Hyponatremia is one of the most frequently observed electrolyte disturbances in coronavirus disease 2019 (COVID-19). Literature describes syndrome of inappropriate antidiuretic hormone (SIADH) as the mechanism of hyponatremia in COVID-19 requiring fluid restriction for management. However, it is important to rule out other cause of hyponatremia in such cases keeping in consideration the effect of an alternate etiology on patient management and outcome [1, 2]. Hyponatremia is defined when serum sodium level less than 135 mmol/L. In many cases, this electrolytic abnormality is caused by a variety of factors [3, 4]. Hyponatremia is the most common electrolyte disorder seen in clinical practice and is associated with increased risk of morbidity and mortality [5, 6]. This electrolytic disequilibrium is classified in hypovolemic, euvolemic, and hypervolemic hyponatremia, each category’s therapeutic approach being different [7]. The most recognizable cause of hyponatremia in COVID-19 is the SIADH; it is found in about 40–50% of patients with this electrolyte disorder [8, 9]. These percentages may be higher in some conditions, such as pneumonia, traumatic head injury, or subarachnoid hemorrhage [10]. In order to establish the diagnosis and etiology of hyponatremia, a careful history and thorough physical examination are required; investigations such as serum sodium level, urine sodium level, serum osmolality, urine osmolality, thyroid function tests, and serum cortisol may be indicated (Fig. 1) [11, 12].
The aim of our study was highlighted on rare cause of hyponatremia happened in COVID-19 patients, which was the dilutional hyponatremia; the reasons for dilutional hyponatremia were due to excessive water intake which is considered as extremely rare reported cases.
Methods
This is a case series, retrospective study. Four patients were reviewed from the Mesaieed Hospital, which is one of the COVID-19 facilities of the Hamad Medical Corporation, Qatar. The patients were admitted during the second wave of pandemic (from March until July 2021) because of mild to moderate COVID pneumonia. The patients experienced cough and fever, and one of them had shortness of breath (PO2 94%) and one with hyposmia and dysgeusia, dysgeusia manifested by the bitterness sensation of tongue. Vital signs were within normal limits except for fever and low oxygen saturation for one patient. Physical examination revealed a well-hydrated patients, a fully conscious, and oriented, with no focal neurological deficit. The rest of the physical examination was unremarkable except for the patient with dyspnea; there was chest crackle mainly on the basal area. Initial laboratory results are shown in Table 1, with a mild to moderate increase in C-reactive protein. Chest X-ray showed a typical ground-glass appearance mainly on the right side for three patients. They received medication according to the protocol; after few days of treatment, their blood laboratory results showed hyponatremia; as compared to the initial readings, hyponatremia workup excluded SIADH. History revealed that the patients were drinking large amounts of water, around 4–5 L/day, because of certain reasons: one patient had dysgeusia, and the other three patients thought that excessive drinking of water is beneficial for COVID-19.
Results
The hyponatremia level was less than 135 mmol/L, other laboratory tests excluded SIADH, and the provisional diagnosis was dilutional hyponatremia. Male/female ratio was 3/1, age from 29- to 45-year old patients with no associated comorbidities. Fluid restriction up to 1.5 L/day showed dramatic improvement of their sodium blood level. The patients discharged in a stable condition. The studied four-patient blood laboratory results are shown in Table 1.
Discussion
Hyponatremia is one of the most common electrolyte disorders, which has a high prevalence of morbidity and mortality rates [13], especially in patients suffering from COVID-19 pneumonia. The physiological control of body water level and electrolyte balance is extremely related to the hypothalamus function. When 0.5% or more of the body water is lost, we feel thirsty. The kidney can excrete about 20–28 L of water a day to control water load, and an excessive intake of water rarely causes hyponatremia [14], which provided with a significant renal function. A decrease in sodium level inhibits an antidiuretic hormone (ADH) secretion, and subsequently, the excreted amount of water via the kidney increases. In case of excessive water intake, hyponatremia develops only when the water intake amount exceeds the water excretion capacity of the kidney [15]. Many publications showed that hyponatremia is associated with prolonged hospitalization and severity, as well as mortality in a number of infectious diseases, especially COVID-19-infected patients [16, 17]. Yousaf et al. mentioned the mechanism of hyponatremia in COVID-19-infected patients secondary to SIADH and its pathophysiology. The hypothesis referring to increased interleukin-6 (IL-6) levels stimulates ADH release [18]. In Yousaf et al. case series, all three patients recovered with fluid restriction. However, it is essential to consider other possible etiologies as a cause of hyponatremia in COVID-19 patients. Hypovolemic hyponatremia should be distinguished from SIADH as these conditions employ different management guidelines and strategies; therefore, early diagnosis and management of hypovolemic hyponatremia affect morbidity and mortality [2]. In our presented case series study, hyponatremia is due to a dilutional one, and due to water intoxication, the diagnosis was done after exclusion of SIADH as well as taking a thorough history from the patient regarding excessive water intake; therefore, hyponatremia was corrected by fluid restriction. Anosmia-hyposmia and dysgeusia are common symptoms of mild-to-moderate COVID-19 cases. They are usually but not always reversible; it can be manifested in different and distorted taste feelings, and in our patient, dysgeusia felt as a bitterness of the tongue; therefore, the patients should try to overcome this sensation by frequent water drinking. We appreciate that the remaining three patients with excessive water intoxication thought that excessive water intake is beneficial to COVID-19 infection. We regard our presented cases were extremely rare, because our search for causes of hyponatremia due to excessive water intake was not existed in COVID-19 patients.
Conclusions
The pathophysiological mechanisms of hyponatremia among COVID-19 patients are multifactorial, and it is not only secondary to SIADH but can also be due to other etiologies. Hyponatremia can be induced by excessive water drinking and considered an extremely rare reported cases.
Availability of data and materials
The data that support the findings of this study are available upon reasonable request from the corresponding author, A. Al-juboori. The data are not publicly available due to privacy restrictions.
Abbreviations
- COVID-19:
-
Coronavirus disease of 2019
- SIADH:
-
Syndrome of inappropriate antidiuretic hormone
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- ADH:
-
Antidiuretic hormone
References
Gina G, Madalina I, Simona B, Anca MP, Nicolae B, Camelia CD (2021) Is there a relationship between COVID-19 and hyponatremia? Medicina 57:55
Khan AA, Ata F, Munir W et al (2020) Fluid replacement versus fluid restriction in COVID-19 associated hyponatremia. Cureus 12(7):9059
MSV E, Cucchiara BL, Koralnik IJ (2020) Coronavirus disease 2019 (COVID-19): neurologic complications and management of neurologic conditions. UpToDate Available online: https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-neurologic-complications-and-management-of-neurologic-conditions?. Accessed 15 Oct 2019
Sterns RH (2020) Diagnostic evaluation of adults with hyponatremia. UpToDate Available online: https://www.uptodate.com/contents/diagnostic-evaluation-of-adults-with-hyponatremia? Accessed 15 Oct 2020
Corona G, Giuliani C, Parenti G, Norello D, Verbalis JG, Forti G et al (2013) Moderate hyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLoS One 8:e80451
Hugo DC, Thibault L, Matilde K, Geoffrey D, Hélène C, Emmanuelle P et al (2021) Hyponatremia is associated with poor outcome in COVID-19. J Nephrol. 1-8
de la Flor C, Merino J, Amado FV, Rodil BB, Marschall A, Rodeles del Pozo M (2020) Hyponatremia in COVID-19 infection: possible causal factors and management. J Allergy Infect Dis 1:53–56
Berni A, Malandrino D, Parenti G, Maggi M, Poggesi L, Peri A (2020) Hyponatremia, IL-6, and SARS-CoV-2 (COVID-19) infection: may all fit together? J Endocrinol Investig 43:1137–1139
Cuesta M, Thompson CJ (2016) The syndrome of inappropriate antidiuresis (SIAD). Best Pract Res Clin Endocrinol Metab 30:175–187
Johannes K, Benjamin S, Björn H (2021) SARS-CoV-2-induced SIADH: a novel cause of hyponatremia. Z Gerontol Geriat 54:301–304
Decaux G, Much W (2008) Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol 3:1175–1184
Andrea B, Danilo M, Giovanni C, Mario M, Gabriele P, Benedetta F (2021) Serum sodium alterations in SARS CoV-2 (COVID-19) infection: impact on patient outcome. Eur J Endocrinol 185(1):137–144
Smith DM, McKenna K, Thompson CJ (2000) Hyponatraemia. Clin Endocrinol (Oxf) 52:667–678
Weiss GJ (2005) Non-psychogenic polydipsia with hyponatremia. Internet J Nephrol [Internet]. 2(1). [cited 2012 Nov 24]
Joo MA, Kim EY (2013) Hyponatremia caused by excessive intake of water as a form of child abuse. Ann Pediatr Endocrinol Metab 18:95–98
Sharma R, Agarwal M, Gupta M, Somendra S, Saxena SK (2020) Clinical characteristics and differential clinical diagnosis of novel coronavirus disease 2019 (COVID-19). In: Coronavirus disease 2019 (COVID-19). 2020 (ed). Springer, Singapore, pp 55–70
Lippi G, South AM, Henry BM (2020) Electrolyte imbalances in patients with severe coronavirus disease 2019 (COVID-19). Ann Clin Biochem 57:262–265
Yousaf Z, Al-Shokri SD, Al-soub H, Mohamed MFH (2020) Covid-19 associated SIADH; a clue in the times of pandemic! Am J Physiol Endocrinol Metab. https://doi.org/10.1152/ajpendo.00178.2020
Acknowledgements
The authors would like to thank the nursing and laboratory staff in the Mesaieed Hospital, Hamad Medical Corporation, Qatar, for their help and support to achieve this work.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AA contributed in manuscript writing. AAH contributed in logistics. ZA contributed in data collection. Each author contributed important intellectual content during manuscript drafting or revision and agrees to be personally accountable for the individual’s own contributions. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent for participation
The cases at hand have already been approved by the authors and the institution’s medical research and ethics committee at the medical research center, and no consent for participation had been obtained because it was retrospective study.
Consent for publication
Not applicable, because the study is retrospective study.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-juboori, A.N., Al Hail, A. & Ahmad Al-juboori, Z. Hyponatremia due to excessive water intake in COVID-19 patients: case series study. Egypt J Intern Med 34, 71 (2022). https://doi.org/10.1186/s43162-022-00158-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-022-00158-0