Abstract
Background
The prevalence of hepatitis C (HCV) infection among the patients on hemodialysis (HD) varies from country to country and from one center to another in the same country. Despite the existence of guidelines for the infection control program, Egypt is one of the countries with high HCV prevalence. In Egypt, the prevalence of HCV among hemodialysis patients in 2015 survey was 50.7%. This study aimed to evaluate the prevalence and seroconversion rate of hepatitis C infection and the risk factors for seroconversion in our community hemodialysis units.
Results
The prevalence of HCV was 34.8% among hemodialysis patients. The seroconversion rate was 13.2%. The positive history of blood transfusion and the frequency of blood transfusion, in addition to the handling by medical staff to equipment and blood products and the number of inserted temporary dialysis catheters, were found to be significant risk factors for seroconversion.
Conclusion
We concluded that there is a high prevalence of HCV infection in the dialysis units of our community and a relatively high seroconversion rate among hemodialysis patients.
Similar content being viewed by others
Background
Hepatitis C virus (HCV) infection is one of the most common blood-borne infections in Egypt. A large number of Egyptians are exposed to infection due to low hygiene and sterilization measures in our community. The Egyptian Demographic Health Survey (EDHS) was conducted in 2008 on a large nationally representative sample. This study estimated HCV prevalence to be 14.7% among the 15–59-year age group. Accordingly, Egypt has the highest HCV prevalence in the world [1].
Most patients infected with HCV via blood transmission and HCV-RNA were detected at 7–21 days after blood transfusion. Blood transfusion is more important in patients who need repeated blood transfusion due to their disorders such as patients with thalassemia, hemophilia, and chronic renal failure and who require hemodialysis [2].
Nosocomial transmission occurred due to using unsterile medical equipment such as endoscopy, angiography, and surgical devices. Medical procedures such as gynecology and cardiology operation, angiography, endoscopy, and colonoscopy can increase the risk for HCV infection rates due to the use of unsterile devices [3].
The prevalence of HCV infection among hemodialysis (HD) patients is generally much higher than that among the general population due to underlying impaired cellular immunity which increases their susceptibility to infection. Also, hemodialysis patients are exposed to prolonged vascular access and exposure to contaminated equipment and handling by medical staff. In addition, HD patients required blood transfusion, frequent hospitalization, and surgery, which increase opportunities for getting nosocomial infection exposure [4].
HCV infection increases the morbidity and mortality rates of both dialysis patients and kidney transplant recipients. Conventional interferon-based therapy for HCV infection has a relatively low virologic response rate and is poorly tolerated by chronic kidney disease (CKD) patients. The recent development of novel direct-acting antiviral (DAA) agents has revolutionized the treatment of HCV infection, especially for CKD patients, a difficult-to-treat population [5].
There was no data registry in Assiut governorate (Egypt) at the time of our study regarding the prevalence of HCV-positive patients and the rate of HCV seroconversion in hemodialysis units. This is a large-scale study.
Methods
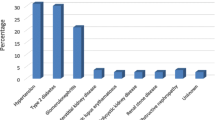
Our study was done in Assiut governorate including 14 dialysis units from January 2017 to January 2018. The study design was observational, a cross-sectional study that included all 1435 patients on regular hemodialysis in Assiut governorate. For HCV diagnosis, we used third-generation enzyme-linked immunosorbent assay (ELISA) for the detection of HCV antibodies. Further evaluation by HCV-RNA PCR was done for those who tested positive for HCV antibody. The initial screening and follow-up every 3 months divided the study population into three groups: patients with negative HCV antibody throughout the study, patients who seroconverted during the study from negative HCV antibody to positive HCV antibody, and patients who tested positive for HCV antibody before dialysis. The seroconverted patients were evaluated regarding the risk factors of HCV transmission (positive family history of HCV, duration of dialysis in years, frequency of blood transfusion and its handling by the medical staff, vascular access either permanent or temporary and surgical procedures) during dialysis period. In addition, observation for adherence to the basic infection control procedures (availability of operated water tap and sink, soap at the sink, paper towels, alcohol hand rub, posters for routine hand wash, gloves, and sharps containers) was conducted in all hemodialysis centers in Assiut governorate, Egypt. Only the basic measures were observed, and we considered any deficient item as nonadherence to guidelines.
Inclusion criteria
We included all the patients who were on regular hemodialysis, the age group was 18–80 years.
Exclusion criteria
We excluded patients who died before the end of the study or received any HD sessions outside our government hemodialysis units. Also, we did not include new HD patients who initiated HD after the study had been started or those with hepatitis B coinfection. Patients with diabetes mellitus were excluded from the study.
Statistical analysis
The data were tested for normality using the Kolmogorov-Smirnov test and for homogeneity variances prior to further statistical analysis. Categorical variables were described by number and percent (N, %), where continuous variables described by the mean and standard deviation (mean, SD). The chi-square test used to compare between categorical variables where compare between continuous variables by t test. A two-tailed p < 0.05 was considered statistically significant. All analyses were performed with the IBM SPSS 20.0 software. Significant factors in multivariate analysis were entered into a logistic regression model to identify the independent predictors of HCV.
Results
The total number of ESRD patients in Assiut governorate is 1435 patients, throughout 14 hemodialysis units. Screening and further follow-up with HCV antibody (ELISA) divided the patients into 3 groups: patients with negative HCV antibody throughout the study, patients who seroconverted during the study from negative HCV antibody to positive HCV antibody, and patients who tested positive for HCV antibody before dialysis as shown in Table 1.
The prevalence of HCV infection among hemodialysis patients was 34.8% while the frequency of seroconversion was 13.2%.
Regarding the demographic data in the current study, the study groups had no significant statistical differences as shown in Table 2.
Comparison between the studied groups with regard to the risk factors for HCV seroconversion showed that repeated blood transfusion, the handling by medical staff to equipment and blood products, and the insertion of temporary dialysis catheters were significant risk factors for HCV seroconversion. Other factors such as the family history of HCV infection, duration of dialysis, and surgical procedures during the dialysis period were insignificant risk factors for HCV seroconversion as shown in Table 3.
According to the multivariate analysis (Table 4), history of blood transfusion, lack of implementation infection control measures, and history of frequent insertion of temporary dialysis catheters were significantly associated with HCV seroconversion.
Discussion
Egypt is the country with the highest HCV prevalence in the world; in 2008, the Egyptian Demographic Health Survey (EDHS), which was conducted on a large nationally representative sample, estimated the prevalence of HCV antibodies and HCV-RNA, among the 15–59-year age group, to be 14.7 and 9.8%, respectively [6].
The present study conducted in 14 dialysis units from January 2017 to January 2018 reviewed the health records of 1435 patients.
The high prevalence agreed with Zahran [7] in Menufia governorate, Egypt, who reported that the prevalence of HCV was 49.6%. Out of the 514 surveyed patients, 259 were found negative for HCV and 255 were found positive.
In addition, it agreed with the study of Sarhan and Kamel [8] in Cairo, Egypt, which reported that the prevalence of HCV antibody at the start of dialysis was 45.2% and the incidence rate of seroconversion was 10.7%. Their study included 987 patients who attended 22 HD centers.
Also, similar rates were reported by other Egyptian studies. A follow-up study including 2351 patients in eight towns of Al Gharbiyah governorate by Khodir et al. [9] revealed that at the start 35% of patients were anti-HCV reactive, and at the end, the seroconversion rate was 11%.
Another retrospective study that agreed with our results retrieved the registered data of the Nephrology Department of Ain Shams University Adult Hospital (El Fattah Abdallah et al.) [10] over a period of 5 years and included 1600 patients (2005–2009). The results indicated that positive HCV antibodies were found in 25.8% of patients.
The prevalence reported in other countries was much lower, which disagreed with our study, for example, Zabadi et al. [11] reported HCV prevalence of 7.4% among hemodialysis patients in the West Bank hospitals, Palestine. Their study included 868 hemodialysis patients attending nine hemodialysis hospitals.
Many factors are contributing to this high prevalence. Blood transfusion is an important factor in the transmission of HCV infection; we found a highly statistically significant difference between HCV seroconverted and HCV seronegative patients regarding the history of previous blood transfusion (P value 0.000).
Similar results, which agreed with our results, have been reported by Khattab [12] in Iraq who detected a positive correlation between blood transfusion and risk of HCV infection. According to their study, a total of 112 patients (66.3%) did not receive any blood transfusions; seven (6.3%) of them became anti-HCV positive, while 57 (33.7%) received blood transfusions of whom five (8.8%) became anti-HCV positive.
In our study, there was a statistically insignificant difference between conversion to HCV-positive state and previous surgeries. This result agreed with the study of Jabbari et al. [13] in Iran, presumed that medical procedures including surgery were not significantly related to HCV antibody positivity. The study was a descriptive-analytical study; HCV antibody was measured in 93 hemodialysis patients in all hospitals affiliated to Golestan University of Medical Sciences.
However, Surendra Kumar et al. [14] did not agree with our results as their study revealed that previous surgery plays a role in developing HCV in their patients. Kumar’s study included 145 patients.
Also, a study conducted by Zarkoon et al. [15] stated that surgical procedures represented a risk factor for HCV seroconversion in hemodialysis patients. His study included 97 patients.
Also, a study conducted in Menufia governorate by Zahran [7] which included 514 patients revealed that the duration of dialysis, a positive family history of HCV infections, and the socioeconomic level were significant among the study groups which disagree with our study where the above-mentioned factors are insignificant.
Another study from Saudi Arabia, Mohamed [16] which agreed with our study, also concluded that isolation of HCV patients, minimizing blood transfusion, and strict application of infection control guidelines help in the prevention of HCV transmission among hemodialysis units. The study included 36 patients over 5 years.
A study conducted by Saxena et al. [17] agreed with our result and found that vascular access played a role in the transmission of HCV and concluded that those with arteriovenous fistula and synthetic grafts were more liable to HCV nosocomial infections more than those with permanent catheters. This could be attributed to the accessibility of HCV to blood circulation due to possible breakdown of standard infection control measures during repeated punctures and cannulations of AVF and PTFE to perform hemodialysis, in a unit with high baseline HCV prevalence. It was a retrospective study that reviewed the records of 189 patients.
Conclusion
The high prevalence of HCV among hemodialysis patients (34.8%) and frequency of seroconversion (13.2%) of HCV in HD patients confirm that HCV infection still remains a major health problem among patients on maintenance HD.
HCV transmission in HD units is multifactorial and includes modifiable factors; the study showed that blood transfusion and the lack of implementation of infection control measures by the medical staff during the handling of equipment and blood products, in addition to temporary dialysis catheter insertion, are statistically significant risk factors for HCV seroconversion in our community.
Recommendations
We recommend the following:
-
Health education program and training of patients, their families, and all hemodialysis staff about HCV and methods of transmission and prevention.
-
Implementation of strict infection control measures during insertion of hemodialysis catheters, wearing sterile gown, mask, overhead, and overshoes. The procedure should be done in a sterile operating room. Also, decontamination and sterilization of ultrasound probe after each procedure.
-
Implementation of isolation procedures by room, machine, and medical requirement to avoid the common and risky handling of the medical and nursing staff.
-
Measures ought to be taken to maintain a strategic distance from blood transfusion as much as possible and ensure the safety of the transfused blood units.
-
Surveillance for detection of the virus by screening all patients before dialysis and when leaving or returning to the center. In initially anti-HCV-negative hemodialysis patients, re-testing with EIA should be considered every 6–12 months.
-
Encouraging the patients to receive the antiviral treatment which showed high efficacy achieving sustained viral response.
Availability of data and materials
The datasets used and/or analyzed during the current study are available on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- DAA:
-
Direct-acting antiviral
- DM:
-
Diabetes mellitus
- EDHS:
-
Egyptian Demographic Health Survey
- EIA:
-
Enzyme immunoassay
- ELISA:
-
Enzyme-linked immunosorbent assay
- ESRD:
-
End-stage renal disease
- HCV:
-
Hepatitis C virus
- HD:
-
Hemodialysis
- INF:
-
Interferon
- SVR:
-
Sustained viral response
References
Lavanchy D (2011) Evolving epidemiology of hepatitis C virus. Clinical Microbiology and Infection 17(2):107–115
Grebely J, Prins M, Hellard M, Cox AL, Osburn WO, Lauer G, Page K, Lloyd AR, Dore GJ (2012) Hepatitis C virus clearance, reinfection, and persistence, with insights from studies of injecting drug users: towards a vaccine. The Lancet infectious diseases 12(5):408–414
Zamani F, Sohrabi M, Poustchi H, Keyvani H, Saeedian FS, Ajdarkosh H, Khoonsari M, Hemmasi G, Moradilakeh M, Motamed N (2013) Prevalence and risk factors of hepatitis C virus infection in Amol city, north of Iran: a population-based study (2008-2011). Hepatitis Monthly 13(12)
Khan S, Attaullah S, Ali I, Ayaz S, Naseemullah KSN, Siraj S, Khan J (2011) Rising burden of hepatitis C virus in hemodialysis patients. J Virol. 8:438
Scott DR, Wong JK, Spicer TS, Dent H, Mensah FK, Mcdonald S, Levy MT (2010) Adverse impact of hepatitis C virus infection on renal replacement therapy and renal transplant patients in Australia and New Zealand. Transplantation 90(11):1165–1171
El-Zanaty F, Way A (2015) Egypt health issue survey 2015. Egyptian Ministry of Health and Population, Cairo
Zahran AM (2014) Hepatitis C virus seroconversion in hemodialysis units with a high prevalence of hepatitis C: do we need isolation? Menoufia Medical Journal 27(3):551
Sarhan II, Kamel CR (2015) Prevalence of hepatitis C virus seroconversion among hemodialysis patients in Egypt. Egyptian Liver Journal 5(2):34–39
Khodir S, Alghateb M, Okasha K, Shalaby S-S (2012) Prevalence of HCV infections among hemodialysis patients in Al Gharbiyah Governorate, Egypt. Arab journal of nephrology and transplantation 5(3):145–147
El Fattah Abdallah, M. A., Baki, A. H., Hakim, S. A. & Kamel, C. R. (2014): Epidemiological study of end-stage renal disease at Ain Shams University Hospital. A five-year retrospective study. Life Science Journal, 11(12).
Zabadi H, Rahal H, Fuqaha R (2016) Hepatitis B and C prevalence among haemodialysis patients in the west bank hospitals. Palestine. BMC. Infect Dis 16:411359–411358
Khattab OS (2008) Prevalence and risk factors for hepatitis C virus infection in hemodialysis patients in an Iraqi renal transplant center. Saudi Journal of Kidney Diseases and Transplantation 19(1):110
Jabbari A, Besharat S, Khodabakshi B (2008) Hepatitis C in hemodialysis centers of Golestan province, northeast of Iran (2005). Hepatitis Monthly 8(1):61–65
Surendra Kumar P, Venu G, Madhusudhana Rao A, Balakrishnan N, Saravanan T, Sofia Rani A (2011) Prevalence and risk factors of hepatitis C among maintenance hemodialysis patients at a tertiary care hospital in Coimbatore, India. Journal Of Clinical and Diagnostic Research 5(4):725–728
Zarkoon AK, Shah K, Habib-Ur-Rehman DA, Ahmed J (2008) Hepatitis C virus infection in patients on long term hemodialysis. Gomal Journal of Medical Sciences 6(1):1–4
Mohamed WZ (2010) Prevention of hepatitis C virus in hemodialysis patients: five years experience from a single center. Saudi Journal of Kidney Diseases and Transplantation 21(3):548
Saxena A, Panhotra B, Sundaram D (2002) The role the type of vascular access plays in the transmission of hepatitis C virus in a high prevalence hemodialysis unit. The journal of vascular access 3(4):158–163
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
HA substantively revised the work. LA: substantial contributions to the conception of the work. NM: substantial contributions to the design of the work. KM: acquisition, analysis, and interpretation of data. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
There was no risk during the application of the research. Privacy and confidentiality was maintained during all stages of assessment. Every patient subjected to this study was informed about the results of the research. The work is approved by Ethical Committee of Faculty of Medicine of Assiut University (approval number 17100520). Consent (verbal) was obtained from the patient to participate in this study. Refusal would not affect medical services which are usually offered. Verbal consent is approved by the ethics committee.
Consent for publication
Consent for publication (verbal) was obtained from all the participating patients. Verbal consent is approved by the ethics committee.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kerollos, K.M.N., El-Ameen, H.A., El Wahed, L.A. et al. Prevalence and seroconversion of hepatitis C among hemodialysis patients in Assiut governorate, Egypt. Egypt J Intern Med 32, 2 (2020). https://doi.org/10.1186/s43162-020-00005-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-020-00005-0