Abstract
This review elucidates the intricate relationship between dietary habits and platelet function, emphasizing the influential role of berries. Both macronutrients and micronutrients in our diet have been found to profoundly affect platelet reactivity and aggregation, presenting a potential therapeutic intervention for platelet-associated disorders. The article particularly highlights the bioactive compounds in berries, such as flavonoids, which have demonstrated a correlation with diminished platelet aggregation and reduced thrombotic risk. The underlying molecular mechanisms, including the modulation of platelet activation pathways, are elaborated upon. Furthermore, the potential clinical implications are explored, suggesting dietary modifications and berry supplementation as complementary approaches to manage platelet-associated conditions. In culmination, the importance of dietary habits, predominantly the consumption of berries, in modulating platelet functionality is underscored, proposing avenues for future investigations in nutritional genomics to devise personalized dietary guidelines.
Similar content being viewed by others
Background
Platelets: a brief overview
Platelets, or thrombocytes, are the smallest cellular components in our blood [1], playing a crucial role in maintaining the balance of hemostasis [2]. Originating from the larger megakaryocytes within the bone marrow [3], these anucleate cell fragments circulate in the bloodstream, acting as the first responders to vascular injury [4, 5]. Upon recognizing damage, platelets adhere to the site, aggregate with one another, and initiate a cascade of reactions to form a hemostatic plug, effectively preventing further blood loss [6]. In addition to their key function in coagulation, platelets are also involved in a multitude of other biological processes, including inflammation, immunity, and angiogenesis, positioning them as significant players in various physiological and pathological conditions [7]. A complex array of signaling molecules, with thrombopoietin taking the lead, orchestrates this process. Once in the bloodstream, platelets are primed for their primary function—maintaining hemostasis [8]. They are the frontline defense against vascular injury, quickly adhering to damaged sites and forming a plug via aggregation [9]. This hemostatic plug is further stabilized through a series of biochemical reactions in the coagulation cascade, ultimately leading to the formation of a stable blood clot.
Effect of diet on platelet function
Diet plays a pivotal role in influencing various aspects of human health, and its impact on platelet function is no exception. Platelets, small cell fragments in the blood, play a crucial role in clotting and wound healing [10]. The foods we consume can either promote or inhibit platelet aggregation. For instance, foods rich in omega-3 fatty acids, such as fatty fish, have been shown to reduce platelet aggregation, potentially lowering the risk of thrombotic events [11, 12]. Conversely, diets high in saturated fats and processed foods might enhance platelet aggregation, elevating the risk for conditions like heart attacks or strokes [13]. Additionally, certain nutrients like flavonoids, found in berries and dark chocolate, and antioxidants, prevalent in fruits and vegetables, can modulate platelet function and improve vascular health [14]. Thus, a balanced diet, rich in whole foods and low in processed items, can be a strategic approach to optimize platelet function and, by extension, overall cardiovascular health.
Platelet activation and dietary factors
Recent research has begun to unravel the influence of dietary factors on platelet activation—a crucial step in the hemostatic process [15]. Various dietary components, ranging from fats, carbohydrates, and proteins to micronutrients like vitamins and minerals, have been found to modulate platelet activation and aggregation. For instance, high levels of dietary omega-3 fatty acids, commonly found in fish and flaxseeds, have been associated with reduced platelet activation. Conversely, diets high in saturated fats and cholesterol may enhance platelet reactivity, contributing to a pro-thrombotic state [16]. Furthermore, micronutrients such as vitamin E and certain polyphenols have been suggested to possess antiplatelet properties [17]. This influence of dietary factors on platelet function has substantial implications, not only for our understanding of hemostasis and thrombosis but also for the potential development of dietary interventions for managing cardiovascular health.
Dietary habits play a crucial role in influencing platelet function, a key component in the body's clotting mechanism [18]. For instance, the fatty acids in our diet can either promote or inhibit platelet aggregation. Omega-3 fatty acids, primarily found in fish oils, such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have been shown to exert antiplatelet effects. These beneficial fatty acids integrate into platelet cell membranes, altering their fluidity and functionality [19]. On the other hand, omega-6 fatty acids, which have pro-inflammatory properties, can promote platelet aggregation. Beyond fatty acids, polyphenols, which abound in fruits, vegetables, tea, and wine, can also impact platelet function. For instance, the specific polyphenols in green tea have demonstrated a reduction in platelet aggregation. Vitamins and minerals, too, weigh in on this balance. While Vitamin E acts as an antioxidant and can deter platelet adhesion and aggregation, Vitamin K is essential for the carboxylation of proteins vital for blood clotting [12, 20]. Furthermore, a deficiency in folate has been linked to increased platelet aggregation [21]. Interestingly, moderate consumption of alcohol, especially red wine, due to its polyphenol content, exhibits antiplatelet effects [22]. Flavonoids, present in various fruits, vegetables, and beverages, can inhibit platelet function, subsequently reducing thrombosis risks. Additionally, natural foods like garlic and onions release sulfur compounds inhibiting platelet aggregation [23]. The Mediterranean diet, characterized by high intakes of fruits, vegetables, whole grains, and olive oil, and moderate consumption of fish and wine, is associated with reduced platelet aggregation [24]. Lastly, certain functional foods and spices, such as curcumin from turmeric and capsaicin from chili peppers, also influence platelet function [25]. Given the myriad ways diet impacts platelet function, it is paramount to approach dietary changes with care, always consulting healthcare professionals, especially when one has underlying health conditions or is on specific medications.
Role of macronutrients and micronutrients on platelets function
Macronutrients, consisting of carbohydrates, proteins, and fats, form the cornerstone of our diet and have a substantial impact on platelet function [26]. High-fat diets, particularly those rich in saturated fats and trans fats, are associated with enhanced platelet aggregation and increased thrombotic risk [27]. Conversely, diets abundant in omega-3 fatty acids, a type of polyunsaturated fat found in foods like fish and walnuts, have been shown to reduce platelet activation and aggregation. Similarly, dietary proteins, particularly those rich in certain amino acids like glycine and arginine, may also influence platelet function [28, 29]. Carbohydrates, especially in their simple, refined forms, may heighten platelet reactivity when consumed excessively, highlighting the intricate relationship between macronutrient intake and platelet physiology. The role of micronutrients in modulating platelet function presents a fascinating avenue of research, revealing the subtle yet profound ways in which these minute dietary components influence cardiovascular health. Micronutrients, including vitamins, minerals, and trace elements, have been increasingly recognized for their potential to fine-tune platelet activity. For instance, vitamin E, known for its antioxidant properties, has been linked to reduced platelet adhesion, while zinc has shown promise in regulating platelet aggregation [30]. Similarly, the presence of adequate magnesium levels can influence platelet calcium channels, potentially modulating platelet responsiveness [31]. As we delve deeper into the molecular mechanisms, it becomes evident that micronutrient imbalances, either deficiencies or excesses, can disrupt the delicate balance of platelet function, with implications for clotting disorders, wound healing, and even chronic cardiovascular diseases (Fig. 1).
In the provided figure, the multifaceted roles of macronutrients and micronutrients in cardiovascular health are depicted, highlighting how different nutrients like fats, proteins, vitamins, and minerals influence the risk and progression of cardiovascular disease. It emphasizes the importance of balanced diets rich in omega-3 fatty acids, antioxidants, and dietary fiber for preventing and managing cardiovascular conditions. This visualization underscores the complex interplay between diet and heart health, aligning with current nutritional strategies in cardiovascular disease prevention and treatment
Influence of specific foods and dietary patterns risk factor in thrombotic disorders
The intricate dance between specific foods, dietary patterns, and platelet function is an evolving area of scientific exploration, shedding light on how our daily dietary choices can shape the very mechanisms of clotting and wound repair [32]. Foods such as berries, rich in flavonoids, and fatty fish, abundant in omega-3 fatty acids, have been spotlighted for their potential to temper platelet aggregation, potentially offering protection against thrombotic events [33,34,35]. In contrast, diets heavy in processed foods, saturated fats, and sugars may hyperactivate platelets, elevating cardiovascular risks [29]. Beyond individual foods, emerging research is also examining the influence of broader dietary patterns. For instance, the Mediterranean diet, characterized by its emphasis on whole grains, fresh produce, and healthy fats, has been associated with improved platelet function and reduced inflammation [36]. Conversely, Western diets, often dominated by processed foods and red meats, might exacerbate platelet reactivity. As we continue to chart this nutritional landscape, it becomes increasingly clear that both specific foods and overarching dietary patterns play pivotal roles in modulating platelet function, with profound implications for cardiovascular health and beyond [37]. Diet, often viewed as a cornerstone of health, has emerged as a significant modifiable risk factor in the realm of thrombotic disorders. Thrombosis, the formation of blood clots within blood vessels, can lead to severe complications such as strokes and heart attacks [38]. While genetic predispositions and certain medical conditions undeniably influence thrombotic risks, dietary habits offer a tangible avenue for intervention [39]. Diets rich in saturated fats, trans fats, and excessive sugars have been linked to increased platelet aggregation and a pro-thrombotic state [40]. Conversely, foods abundant in omega-3 fatty acids, antioxidants, and other anti-inflammatory compounds can potentially mitigate these risks by promoting a more balanced platelet response and vascular health [12, 41]. As we deepen our understanding of nutrition’s role in thrombosis, it becomes evident that embracing a heart-healthy diet can be a powerful strategy in the fight against thrombotic disorders.
Diet-based interventions and their effect on platelet function
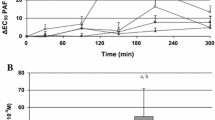
Diet-based interventions have increasingly come to the forefront of research as potential modulators of platelet function, offering a promising avenue for both the prevention and management of related disorders [42]. The intricate relationship between what we consume and how our platelets respond is becoming clearer, with specific dietary components showing the capacity to either inhibit or enhance platelet aggregation. For instance, the inclusion of omega-3 fatty acids, predominantly found in fatty fish, has been associated with reduced platelet reactivity, potentially diminishing the risk of thrombotic events [43]. On the other hand, diets high in sodium and saturated fats might amplify platelet activation, posing cardiovascular challenges [44]. Beyond individual nutrients, holistic dietary patterns, such as the Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diets, have been studied for their collective impact on platelet function, often showing favorable outcomes [45]. As this review article delves into ‘Diet-based Interventions and Their Effect on Platelet Function,’ it underscores the transformative potential of dietary shifts, not just as adjuncts, but as central players in optimizing platelet function and overall vascular health (Fig. 2).
The figure illustrates the link between high-fat diets and increased cardiovascular risks, particularly in the development of thrombotic disorders. It highlights how unhealthy fats contribute to arterial plaque and thrombosis and also shows the influence of other factors like genetics, lifestyle, and existing health conditions. This visual summary underscores the importance of a holistic approach to understanding and managing cardiovascular health
The influence of dietary habits on platelet-focused drug efficacy
The interplay between dietary habits and the efficacy of platelet-focused drugs is an emerging area of research, revealing the nuanced ways in which our food choices can impact pharmacological outcomes. Certain foods and dietary components have been identified to either potentiate or diminish the effectiveness of drugs targeting platelet function [16]. For instance, grapefruit and its derivatives, known to interfere with the cytochrome P450 enzyme system, can alter the metabolism of some antiplatelet medications, potentially leading to altered drug levels and efficacy [46]. Similarly, high vitamin K-containing foods might counteract the effects of anticoagulants like warfarin, necessitating dose adjustments [47]. Beyond individual foods, broader dietary patterns outcomes [48]. “The Influence of Dietary Habits on Platelet-focused Drug Efficacy,” it underscores the imperative for a holistic approach, considering not just the drug, but also the dietary backdrop against which it operates, ensuring optimal therapeutic results and patient safety.
Genomic and metabolomic interactions: platelets and diet
The intricate nexus between genomics, metabolomics, platelets, and diet offers a compelling glimpse into the future of personalized nutrition and medicine [49]. Genomic variations can influence how individuals respond to specific dietary components, and cART drugs subsequently affect platelet function [50, 51]. For instance, certain genetic polymorphisms might render an individual more responsive to the anti-aggregatory effects of omega-3 fatty acids [52]. On the metabolomic front, the array of small-molecule metabolites resulting from food digestion can directly or indirectly modulate platelet activity [53]. For example, specific metabolites derived from the gut microbiota’s breakdown of dietary fibers might influence platelet responsiveness [54]. As we delve deeper into this confluence of genomics and metabolomics in the context of “Platelets and Diet, it becomes evident that understanding these interactions can pave the way for tailored dietary recommendations [55]. Such precision nutrition, informed by an individual's genetic makeup and metabolic profile, holds the promise of optimizing platelet function and, by extension, cardiovascular health, marking a paradigm shift from generalized guidelines to individualized dietary strategies [56].
Personalized nutrition: the future of platelet function modulation
Personalized nutrition stands at the forefront of a transformative approach to modulating platelet function, heralding a new era where dietary recommendations are tailored to individual genetic and metabolic profiles [57, 58]. Rather than adhering to broad dietary guidelines, personalized nutrition delves into the unique genetic makeup of an individual, identifying specific susceptibilities and strengths that can influence platelet responsiveness to certain foods [59]. For instance, an individual with a specific genetic variant might benefit more from a diet rich in omega-3 fatty acids in terms of platelet aggregation inhibition [60]. Additionally, with advancements in metabolomics, we can now understand how an individual’s unique metabolic landscape interacts with dietary components, further refining dietary interventions [61]. As we navigate the realm of “Personalized Nutrition: The Future of Platelet Function Modulation”, it becomes clear that the future of nutrition lies not in one-size-fits-all recommendations, but in bespoke dietary strategies that cater to individual nuances, maximizing therapeutic potential and paving the way for optimal cardiovascular health [62].
Conclusion
The interplay between platelets and diet is an expanding realm of research with the potential to significantly influence our understanding and management of thrombotic disorders. This review has underscored the fact that dietary factors, both macronutrients and micronutrients, can notably modulate platelet function. Consequently, diet represents a critical and modifiable risk factor for thrombosis, with potential implications for the prevention and management of thrombotic disorders. Our understanding of these interactions, while growing, is far from complete. Future research in genomics and metabolomics is expected to shed more light on the complex biochemical pathways and genetic variations that determine individual responses to dietary factors. This knowledge could pave the way for more personalized dietary interventions capitalizing on the emerging field of personalized nutrition. Embracing a holistic view of platelet function, one that incorporates the role of diet, can enrich our understanding of thrombosis and potentially provide new therapeutic strategies. The prospect of personalized nutrition offers a tantalizing opportunity to enhance our ability to modulate platelet function through diet, underscoring the importance of continued research in this dynamic and vital field of biomedicine.
Availability of data and materials
Not applicable.
References
Fabricius H-Å, Starzonek S, Lange T. The role of platelet cell surface P-selectin for the direct platelet-tumor cell contact during metastasis formation in human tumors. Front Oncol. 2021;11:642761.
Das RK, Datta T, Biswas D, Duss R, O’Kennedy N, Duttaroy AK. Evaluation of the equivalence of different intakes of Fruitflow in affecting platelet aggregation and thrombin generation capacity in a randomized, double-blinded pilot study in male subjects. BMC Nutrition. 2021;7(1):80.
Qu M, Zou X, Fang F, Wang S, Xu L, Zeng Q, et al. Platelet-derived microparticles enhance megakaryocyte differentiation and platelet generation via miR-1915-3p. Nat Commun. 2020;11(1):4964.
Menter DG, Kopetz S, Hawk E, Sood AK, Loree JM, Gresele P, et al. Platelet “first responders” in wound response, cancer, and metastasis. Cancer Metastasis Rev. 2017;36(2):199–213.
Martin JF, Kristensen SD, Mathur A, Grove EL, Choudry FA. The causal role of megakaryocyte–platelet hyperactivity in acute coronary syndromes. Nat Rev Cardiol. 2012;9(11):658–70.
Johansson P, Ostrowski S, Secher N. Management of major blood loss: an update. Acta Anaesthesiol Scand. 2010;54(9):1039–49.
Nurden AT. Platelets, inflammation and tissue regeneration. Thrombosis Haemostasis. 2011;105(S 06):S13–33.
van der Meijden PE, Heemskerk JW. Platelet biology and functions: new concepts and clinical perspectives. Nat Rev Cardiol. 2019;16(3):166–79.
Gaertner F, Massberg S, editors. Blood coagulation in immunothrombosis—at the frontline of intravascular immunity. Seminars in immunology; 2016: Elsevier.
Nilsson RJA, Karachaliou N, Berenguer J, Gimenez-Capitan A, Schellen P, Teixido C, et al. Rearranged EML4-ALK fusion transcripts sequester in circulating blood platelets and enable blood-based crizotinib response monitoring in non-small-cell lung cancer. Oncotarget. 2016;7(1):1066.
Pierre S, Crosbie L, Duttaroy AK. Inhibitory effect of aqueous extracts of some herbs on human platelet aggregation in vitro. Platelets. 2005;16(8):469–73.
Basak S, Das RK, Banerjee A, Paul S, Pathak S, Duttaroy AK. Maternal obesity and gut microbiota are associated with fetal brain development. Nutrients. 2022;14(21):4515.
Duttaroy AK. Postprandial activation of hemostatic factors: role of dietary fatty acids. Prostaglandins Leukot Essent Fatty Acids. 2005;72(6):381–91.
Steinberg FM, Bearden MM, Keen CL. Cocoa and chocolate flavonoids: implications for cardiovascular health. J Am Diet Assoc. 2003;103(2):215–23.
Lordan R, Tsoupras A, Zabetakis I. The potential role of dietary platelet-activating factor inhibitors in cancer prevention and treatment. Adv Nutr. 2019;10(1):148–64.
Santhakumar AB, Bulmer AC, Singh I. A review of the mechanisms and effectiveness of dietary polyphenols in reducing oxidative stress and thrombotic risk. J Hum Nutr Diet. 2014;27(1):1–21.
Skalski B, Rywaniak J, Szustka A, Żuchowski J, Stochmal A, Olas B. Anti-platelet properties of phenolic and nonpolar fractions isolated from various organs of Elaeagnus rhamnoides (L.) A. Nelson in whole blood. Intern J Mol Sci. 2021;22(6):3282.
Renaud S, Godsey F, Dumont E, Thevenon C, Ortchanian E, Martin J. Influence of long-term diet modification on platelet function and composition in Moselle farmers. Am J Clin Nutr. 1986;43(1):136–50.
De Carvalho CC, Caramujo MJ. The various roles of fatty acids. Molecules. 2018;23(10):2583.
Tsugawa N, Shiraki M. Vitamin K nutrition and bone health. Nutrients. 2020;12(7):1909.
Tomic-Smiljanic M, Vasiljevic D, Lucic-Tomic A, Andjelkovic N, Jakovljevic V, Bolovich S, et al. Influence of different supplementation on platelet aggregation in patients with rheumatoid arthritis. Clin Rheumatol. 2019;38:2443–50.
Snopek L, Mlcek J, Sochorova L, Baron M, Hlavacova I, Jurikova T, et al. Contribution of red wine consumption to human health protection. Molecules. 2018;23(7):1684.
Olas B. Anti-aggregatory potential of selected vegetables—promising dietary components for the prevention and treatment of cardiovascular disease. Adv Nutr. 2019;10(2):280–90.
Schwingshackl L, Morze J, Hoffmann G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br J Pharmacol. 2020;177(6):1241–57.
Srinivasan K. Anti-cholelithogenic potential of dietary spices and their bioactives. Crit Rev Food Sci Nutr. 2017;57(8):1749–58.
Akowuah PK. Diet-based strategies for mitigating obesity-induced corneal dysregulation: timing of diet intake vs. macronutrient composition of diet 2022.
Violi F, Pastori D, Pignatelli P, Carnevale R. Nutrition, thrombosis, and cardiovascular disease. Circ Res. 2020;126(10):1415–42.
Golanski J, Szymanska P, Rozalski M. Effects of omega-3 polyunsaturated fatty acids and their metabolites on haemostasis—current perspectives in cardiovascular disease. Int J Mol Sci. 2021;22(5):2394.
Mallick R, Basak S, Das RK, Banerjee A, Paul S, Pathak S, et al. Fatty Acids and their Proteins in Adipose Tissue Inflammation. Cell Biochemistry and Biophysics. 2023:1–17.
Gallo CG, Fiorino S, Posabella G, Antonacci D, Tropeano A, Pausini E, et al. The function of specialized pro-resolving endogenous lipid mediators, vitamins, and other micronutrients in the control of the inflammatory processes: possible role in patients with SARS-CoV-2 related infection. Prostaglandins Other Lipid Mediat. 2022;159:106619.
Gotru SK, Mammadova-Bach E, Sogkas G, Schuhmann MK, Schmitt K, Kraft P, et al. MAGT1 deficiency dysregulates platelet cation homeostasis and accelerates arterial thrombosis and ischemic stroke in mice. Arterioscler Thromb Vasc Biol. 2023;43(8):1494–509.
Gioia C, Lucchino B, Tarsitano MG, Iannuccelli C, Di Franco M. Dietary habits and nutrition in rheumatoid arthritis: can diet influence disease development and clinical manifestations? Nutrients. 2020;12(5):1456.
Barin A, Das RK, Bastani NE, Iversen PO, Duttaroy AK. Extracts of tamarillo, horned melon, and raspberries, but not extract of pear, inhibit human blood platelet aggregation: Investigating the underlying factors for their differential mechanisms. 2023.
Das D, Adhikary S, Das RK, Banerjee A, Radhakrishnan AK, Paul S, et al. Bioactive food components and their inhibitory actions in multiple platelet pathways. J Food Biochem. 2022;46(12):e14476.
Mallick R, Duttaroy AK. Modulation of endothelium function by fatty acids. Mol Cell Biochem. 2022;477(1):15–38.
Tsigalou C, Konstantinidis T, Paraschaki A, Stavropoulou E, Voidarou C, Bezirtzoglou E. Mediterranean diet as a tool to combat inflammation and chronic diseases. An overview Biomedicines. 2020;8(7):201.
English CJ, Mayr HL, Lohning AE, Reidlinger DP. The association between dietary patterns and the novel inflammatory markers platelet-activating factor and lipoprotein-associated phospholipase A2: a systematic review. Nutr Rev. 2022;80(6):1371–91.
Rawish E, Nording H, Münte T, Langer HF. Platelets as mediators of neuroinflammation and thrombosis. Front Immunol. 2020;11:548631.
Patel P, Michael JV, Naik UP, McKenzie SE. Platelet FcγRIIA in immunity and thrombosis: adaptive immunothrombosis. J Thromb Haemost. 2021;19(5):1149–60.
Hutachok N, Angkasith P, Chumpun C, Fucharoen S, Mackie IJ, Porter JB, et al. Anti-platelet aggregation and anti-cyclooxygenase activities for a range of coffee extracts (Coffea arabica). Molecules. 2020;26(1):10.
Oppedisano F, Macrì R, Gliozzi M, Musolino V, Carresi C, Maiuolo J, et al. The anti-inflammatory and antioxidant properties of n-3 PUFAs: their role in cardiovascular protection. Biomedicines. 2020;8(9):306.
Rathod KS, Velmurugan S, Ahluwalia A. A ‘green’diet-based approach to cardiovascular health? Is inorganic nitrate the answer? Mol Nutr Food Res. 2016;60(1):185–202.
Brar SS, Ten Berg J, Marcucci R, Price MJ, Valgimigli M, Kim H-S, et al. Impact of platelet reactivity on clinical outcomes after percutaneous coronary intervention: a collaborative meta-analysis of individual participant data. J Am Coll Cardiol. 2011;58(19):1945–54.
O’Kennedy N, Crosbie L, van Lieshout M, Broom JI, Webb DJ, Duttaroy AK. Effects of antiplatelet components of tomato extract on platelet function in vitro and ex vivo: a time-course cannulation study in healthy humans. Am J Clin Nutr. 2006;84(3):570–9.
Fung TT, Hu FB, Wu K, Chiuve SE, Fuchs CS, Giovannucci E. The mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets and colorectal cancer. Am J Clin Nutr. 2010;92(6):1429–35.
Holmberg M, Tornio A, Neuvonen M, Neuvonen P, Backman J, Niemi M. Grapefruit juice inhibits the metabolic activation of clopidogrel. Clin Pharmacol Ther. 2014;95(3):307–13.
Schurgers LJ, Teunissen KJ, Hamulyák K, Knapen MH, Vik H, Vermeer C. Vitamin K–containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7. Blood. 2007;109(8):3279–83.
Tapsell LC, Neale EP, Probst Y. Dietary patterns and cardiovascular disease: insights and challenges for considering food groups and nutrient sources. Curr Atheroscler Rep. 2019;21:1–8.
Semwal P, Painuli S, JP SB, Jamloki A, Rauf A, Olatunde A, et al. Exploring the nutritional and health benefits of pulses from the Indian Himalayan region: a glimpse into the region’s rich agricultural heritage. Food Chemistry. 2023;422:136259.
Kunicki TJ, Williams SA, Nugent DJ. Genetic variants that affect platelet function. Curr Opin Hematol. 2012;19(5):371–9.
Das RK, Roy D, Sahoo N, Roy U. IFIT3 gene expression and function contribute to hand pathology even with antiretroviral therapies (CARTS). Innov Aging. 2022;6(Suppl 1):843.
Cambria-Kiely JA, Gandhi PJ. Aspirin resistance and genetic polymorphisms. J Thromb Thrombolysis. 2002;14:51–8.
Zhao HW, Serrano K, Stefanoni D, D’Alessandro A, Devine DV. In vitro characterization and metabolomic analysis of cold-stored platelets. J Proteome Res. 2021;20(5):2251–65.
Kumar J, Rani K, Datt C. Molecular link between dietary fibre, gut microbiota and health. Mol Biol Rep. 2020;47:6229–37.
Dutta-Roy AK. Dietary components and human platelet activity. Platelets. 2002;13(2):67–75.
Simopoulos AP, Serhan CN, Bazinet RP. The need for precision nutrition, genetic variation and resolution in Covid-19 patients. Mol Aspects Med. 2021;77:100943.
Atlante A, Amadoro G, Bobba A, Latina V. Functional foods: an approach to modulate molecular mechanisms of Alzheimer’s disease. Cells. 2020;9(11):2347.
De Gregori M, Muscoli C, Schatman ME, Stallone T, Intelligente F, Rondanelli M, et al. Combining pain therapy with lifestyle: the role of personalized nutrition and nutritional supplements according to the SIMPAR feed your destiny approach. J Pain Res. 2016;9:1179–89.
Scharf RE, editor Drugs that affect platelet function. Seminars in thrombosis and hemostasis; 2012: Thieme Medical Publishers.
Gajos G, Rostoff P, Undas A, Piwowarska W. Effects of polyunsaturated omega-3 fatty acids on responsiveness to dual antiplatelet therapy in patients undergoing percutaneous coronary intervention: the OMEGA-PCI (OMEGA-3 fatty acids after pci to modify responsiveness to dual antiplatelet therapy) study. J Am Coll Cardiol. 2010;55(16):1671–8.
Ali A, Mughal A, Ahmad S, Abbas S, Mumtaz A, Ahmed I. Microbial metabolomics: recent advancements and applications in infectious diseases and drug discovery. Recent Advances and Future Perspectives of Microbial Metabolites: Elsevier; 2023. p. 269–335.
Albadawi DA, Ravishankar D, Vallance TM, Patel K, Osborn HM, Vaiyapuri S. Impacts of commonly used edible plants on the modulation of platelet function. Int J Mol Sci. 2022;23(2):605.
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Contributions
Susma Roy conceived the research topic, conducted the literature review, and took the lead in writing the manuscript. Kumar Paul contributed to refining the research focus, assisted in reviewing the literature, and participated in writing and revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roy, S., Paul, K. Nourishing the clot: a comprehensive review of dietary habits and their implications for platelet function. Bull Fac Phys Ther 29, 7 (2024). https://doi.org/10.1186/s43161-023-00173-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43161-023-00173-4