Abstract
Background
Obesity in children is a frequent and serious problem that can impede motor ability performance, necessitating extra attention and early intervention efforts. The purpose of this study was to determine the relation between body mass index (BMI) and motor proficiency in Egyptian children. Two-hundred normal healthy children from both sexes (6 to 8 years old) were enrolled. BMI was defined by dividing weight in kilograms by height in meters squared (kg/m2), and motor proficiency was evaluated by Bruininks-Oseretsky Test 2 of Motor Proficiency Short Form (BOT-2 SF). Participants were classified into four categories based on the Centers for Disease Control and Prevention (CDC) cutoff points including underweight, normal, overweight, and obese.
Results
Between-group analysis demonstrated a significant difference between groups where (χ2 (3) = 131.50, P = 0.0001), with the obese group showing the worst motor ability, with mean differences at 95% confidence intervals of 7.44 for underweight, 81.14 for overweight, and 108.92 for obese children. The correlation coefficients of BOT-2 SF and BMI show a significant negative correlation (R = −0.723, P = 0.0001). Regression analysis revealed that BMI can significantly predict the BOT-2 SF (F = 216.94, P = 0.0001).
Conclusion
Excess body weight in the period of early childhood in Egyptians has a deleterious effect on motor skill performance; also, children who were normal weight or underweight had higher motor skills than those who were overweight or obese.
Similar content being viewed by others
Key messages
-
Obesity is a common problem in Egyptian children.
-
BMI can predict the level of motor proficiency in children.
-
Normal-weight children have superior motor proficiency than overweight or obese children.
Background
Obesity and lack of activity in children are major issues in today’s society. Sedentary behavior in children has increased sharply, owing primarily to a rise in media consumption [1], and the percentages of people who are overweight or obese have remained stable at a high level [2]. This problem is global, affecting many low- and middle-income countries (LMICs), especially in urban areas [3]. Egypt is one of the LMICs where overweight and obesity among school children are becoming a serious problem, with rates rising from 6 to 15% between 1990 and 2010 [4]. In the USA, Ogden et al. [5] found that overweight and obese children are more likely to be obese as adults and are more likely to develop chronic diseases at an earlier age.
Obese people engage in physical activity at low levels, and inactive people are more liable to become obese; it is a vicious cycle. Whatever the origin or rationale, a large body of evidence suggests that a higher degree of body fat is linked to a lower level of physical performance [6].
Early childhood period is critical for motor skill development [7], as well as establishing a physically active lifestyle [8]. Interaction with the environment is critical for motor development, particularly in infancy. Early in life, environmental inputs, particularly repeated replications of these stimuli, are important clues for a child’s motor memory [9]. Children are more exposed to environmental factors that have negative health consequences; children’s heightened sensitivity to environmental changes is a significant indicator, as it helps us better comprehend present health hazards. Simultaneously, interpreting what is happening to children in the context of environmental causes of disease entails understanding not only the current burden of disease but also future burdens, because many of the effects on children's health are carried over into adulthood, adding to the disease burden [10].
Motor proficiency, a measure of a child’s motor development that can be judged by qualitatively various components of both gross and fine motor skills [11], is one of the most important factors that influences physical activity participation [12]. Obesity in children is related to a decline in motor proficiency, which is a vital competence in this stage of development [13]. Motor proficiency is also found to be related to the status of weight. For example, as compared to normal-weight children, overweight children have large difficulties with core physical abilities and also lower self-concept judgments [14]. The first-grade children’s higher BMI is linked to poor gross motor development. Also, children who engage in more activities in their spare time develop their gross motor skills more effectively [15]. There are, however, a number of additional variables that might affect the motor skills in children, including nutrition, illness, physical activity engagement, and social circumstances [16].
Globally, a few previous reports, with relatively conflicting outcomes, examined the relationships between physical activity, activity loss, motor proficiency, and body mass index [16]. While some demonstrated a negative relationship [14, 17,18,19], others demonstrated no association at all [20, 21]. These contradictory findings could be attributed to a small sample size or a heterogeneous sample, with most trials using a wide age range.
In Egypt, several studies performed in Cairo [22], Assiut [23], Menoufia [4], Sharkia [24], Sohaj [25], and Port Said [3] discussed the prevalence of childhood overweight and obesity. The prevalence of underweight and overweight in Egyptian school children, as well as their relationship with physical fitness, was also investigated [26]. However, none of the previous studies cleared the impact of both being overweight and being underweight on motor skill proficiency. Therefore, due to the insufficient data and lack of studies in this field in Egypt, it is necessary to conduct this in our research, which will aid in identifying the factors that may obstruct development. So, this will facilitate the creation of developmentally appropriate programs for regulating body weight and achieving optimum movement competence. Consequently, the purpose of the present study was to determine the relationship between BMI and motor proficiency in Egyptian children.
Methods
This cross-sectional study was performed in 2021 according to the code of ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Ethics approval was obtained from the Faculty of Physical Therapy, Cairo University, Egypt (no.: P.T.REC/012/003400). Initially, 215 Egyptian children were accepted, with 200 healthy children (92 girls and 108 boys) finally participated in the study. They were chosen from elementary schools in North Giza. Fifteen children did not participate because some of their family members were affected by covid-19. Before beginning the study procedures, a formal consent form was completed and received with parental approval for participation in the study and publication of the results. Inclusion criteria were normal children aged from 6 to 8 years, and they can follow directions and comply during evaluation. Excluded children were athletes, children with musculoskeletal or neuromuscular disorders, children with cardiac or respiratory disorders, and children with intellectual disabilities. Participants were classified into four categories for comparison (underweight, normal, overweight and obese).
Evaluation of BMI
Standard protocols for determining height and weight were followed. The height of children was measured to the closest 0.2 cm without shoes with the use of a handheld stadiometer (SECA, Hamburg, Germany). Children were standing with their heels together, gaze forward, shoulders relaxed, and arms at sides. A calibrated electronic scale was used to measure weight to the closest 0.1 kg (Tanita, Tokyo, Japan). Using the methodology recommended by CDC, BMI (kg/m2) was calculated and converted to z-scores [27]. BMI z-scores consider age and gender variances, allowing for comparisons. BMI percentiles in this study were classified into four categories based on age and gender: normal weight < 85th percentile, overweight ≥ 85th percentile, obese ≥ 95th percentile, and underweight (< 5th percentile).
Evaluation of motor proficiency
Using BOT-2 SF, a well-recognized product-oriented test for assessing gross and fine motor abilities in children aged 4 to 21 years [28]. The BOT-2 SF is a test of motor proficiency that is both valid and reliable [29]. It consists of 14 items drawn from the eight subtests of the entire form (Appendix 1). Seven of the 14 items were accessible in two trials, with the higher trial score being used to calculate the total score. Each child actively completed the 14 items, and after the testing was completed, raw scores were converted into point scores, which were then summed up to obtain the overall point score on the test sheet. To achieve uniformity of scores, eliminate the effect of age, and allow proper comparison of scores, each child’s total point score was converted to a standard score according to the test manual [28].
Data analysis
The data were checked for normality, variance homogeneity, and the presence of outliers before final analysis. Descriptive analysis utilizing histograms showed that the data violates the parametric assumption as determined by Shapiro-Wilk’s test (P > 0.05). The differences between groups in motor proficiency (BOT-2 SF) were examined using the Kruskal-Wallis H test with Dunn’s pairwise post hoc comparison using the Bonferroni correction. Correlations between BOT-2 SF and BMI were further analyzed with Spearman correlation coefficient. A simple linear regression analysis was carried out to create a prediction model for the value of BOT-2 SF in relation to BMI. For all statistical tests, the significance level was established at P < .05. All statistical tests were conducted using SPSS for Windows, version 23 (SPSS, Inc., Chicago, IL).
Results
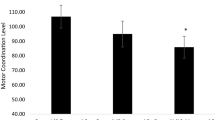
The baseline characteristics and descriptive analysis of all variables addressed in this study are listed in Table 1. There were no statistically significant differences between groups in terms of gender or age (P > 0.05). However, regarding BOT-2 SF, there was a considerable difference between groups where (χ2 (3) = 131.50, P = 0.0001). A significant difference between groups in terms of their differential impact on BOT-2 SF was revealed, while normal and underweight children showed better motor proficiency scores than overweight and obese groups. Pairwise comparison analysis revealed a significant difference between groups compared to normal, with the obese group showing the worst motor ability, with mean differences at 95% confidence intervals of (7.44) for underweight, (81.14) for overweight, and (108.92) for obese children (Table 2, Fig. 1).
The correlation coefficients of BOT-2 SF with different degrees of BMI show statistically significant negative correlation (R = 0.723, P = 0.0001). Regression analysis revealed that BMI can significantly predict the BOT-2 SF (F = 216.94, P = 0.0001), (Table 3, Fig. 2). The R2 was 0.520, indicating that the BMI model can account for 52% of the changes in BOT-2 SF. The prediction equation BOT-2 SF = (107.84) + (−4.315×).
Discussion
This study was conducted to determine the relation between BMI and motor proficiency in Egyptian children aged 6–8 years old. Indeed, obesity and overweight in children affect their sports and physical activities involvement and also their capacity to perform motor skills. Our findings showed that BMI and motor proficiency in Egyptian children had a significant negative relationship. This finding is similar to that of Wrotniak et al. [6] who discovered a strong relationship between normalized BMI values and BOT-2 SF scores. Also, Möller et al. [30] discovered significant associations between greater BMI and poorer motor skills. Cheng et al. [31] found that a high relative weight causes future motor skill decreases, not the other way around, confirming our results that obesity has a deleterious effect on motor proficiency in childhood. Hamilton et al. [32] discovered a negative association between preschoolers’ motor skill performance and their BMI scores. This could mean that obesity in preschoolers will hinder and prolong their motor skills in the future. This is reinforced by Stodden et al. [33] who reported that if children are not proficient in performing basic motor abilities (such as running, hopping, single limb support, and so on), they may be insufficiently active at preschool age, which can lead to a rise in their obesity level later on. As a result, obesity and motor skill limitations in this study participants may represent a continuation of their preschool attitude. Moreover, obese children in school before puberty have a greater risk of remaining obese in adulthood and acquiring chronic health problems related to obesity [34]. Obviously, childhood obesity at different ages is a persistent condition that may take a long time to resolve, and this may have an impact on children’s motor skills.
Recent research performed in the Eastern Mediterranean region (EMR) show that the prevalence of overweight among school-aged children (6–18 years old) has reached alarming levels [35], with Kuwait having the highest rate (32%) [36]. There was also an alarming rate of overweight (including obese subjects) among Egyptian children from Assiut, with a prevalence of 24.06% among those aged 6–11 years [26]. Indeed, in most EMR nations, economic improvement has resulted in nutrition transitions in food consumption, centered on energy-dense diets high in fats (i.e., saturated fat, cholesterol, and refined carbohydrates) and low in polyunsaturated fatty acids and dietary fiber. This eating pattern, along with a sedentary lifestyle and elevated levels of stress, has resulted in a significant gain in weight [37]. Previous research has also found a small decline in physical fitness among Egyptian students in primary school age [38].
Our findings also cleared that the Egyptian children who were normal weight or underweight had higher motor proficiency scores than those who were overweight or obese. Logan et al. [20], who discovered that overweight and obese children perform poorly on motor tasks compared to normal and underweight ones, confirm this conclusion. Another study by Gentier et al. [39] said that when compared to their healthy-weight counterparts, overweight and obese children performed badly in manual dexterity, gross, and fine motor skills. According to Abdelkarim et al. [26], the total performance of overweight and obese children was poorer than that of normal-weight children, particularly for balance and motor abilities. Furthermore, these findings are congruent with the findings of Abdel-aziz et al. [40], who found that overweight Egyptian children have considerably lower physical functioning than children with a normal BMI.
Several factors must be considered in order to understand why children with obesity have lower levels of motor proficiency than children of normal weight. Individual, task, and environmental constraints all play a role in motor development, which is a continuing process with multiple variables and interactions [41]. Constrains can affect each other as follows: first, body weight gain changes the body structure and increases the size of various body parts, making actions that are not stationary such as jumping, sprinting, and lifting the weight of one’s own body, more complex and demanding biomechanically [17]. Second, extra body weight has been associated with a drop in perceived physical skill in addition to a reduction in actual physical ability [42]. Obese children’s lower actual and perceived motor skill competence may prevent them from participating in sports and recreational activities that they enjoy with their usual peers [43]. Furthermore, overweight or obese children are more likely to suffer from orthopedic issues, which can result in pain and, as a result, a reduction in motoric function [13]. Stodden et al. [33] stated that the development of motor skill competence encourages regular physical activity, which in turn also promotes motor skill proficiency. These considerations reinforce the current study’s findings, emphasizing the dangers of childhood obesity.
The findings of this study contradict those of Abdelkarim et al. [26], who claimed that, similar to overweight and obese subjects’ lower physical performance, underweight children’s overall performance was also lower than normal-weight children’s, particularly in motor tests based on speed and strength abilities (e.g., sprint, push-ups, and sit-ups). These findings imply that, in the same way that greater focus is paid to overweight and obesity issues, more attention is needed to control abnormal weight loss and prevent its negative impact on children’s physical fitness.
Based on the current study, the percentage of BMI can predict the level of motor performance in early childhood, emphasizing the importance of physical educators in primary schools being aware of children’s weight gains and losses and how to monitor their weight and motor skills to determine the need for referral to specialists who can devise a therapeutic intervention plan. Coordination between specialists and physical educators is critical for facilitating engagement in motor skills that can help children lose weight and maintain an active lifestyle.
Study limitations
-
1.
Convenience sampling that does not represent the entire population.
-
2.
The sample was taken from a localized population area.
Conclusions
Motor proficiency in children is adversely associated with BMI, and normal-weight children have superior motor proficiency than overweight or obese children. Early childhood obesity can predict the motor proficiency. Consequently, early intervention programs may aid in the prevention of motor skill decreases; this could have a good impact on children’s physical activity and fitness.
Recommendations
We recommend future researchers to perform studies on a wider population from different Egyptian environments to draw meaningful conclusion.
Availability of data and materials
The data collected and/or analyzed during the study are available from the corresponding author on reasonable request and after institutional approval.
Abbreviations
- BMI:
-
Body mass index
- BOT-2 SF:
-
Bruininks-Oseretsky Test 2 of Motor Proficiency Short Form
- CDC:
-
Centers for Disease Control and Prevention
- LMICs:
-
Low- and middle-income countries
- EMR:
-
Eastern Mediterranean region
References
Auhuber L, Vogel M, Grafe N, Kiess W, Poulain T. Leisure Activities of Healthy Children and Adolescents. Int J Environ Res Public Health. 2019;16(12):2078. https://doi.org/10.3390/ijerph16122078.
Keß A, Spielau U, Beger C, Gausche R, Vogel M, Lipek T, et al. Further stabilization and even decrease in the prevalence rates of overweight and obesity in German children and adolescents from 2005 to (2015): a cross-sectional and trend analysis. Public Health Nutr. 2017;20(17):3075–83 pmid:28931448.
El-Said NB, Abo Barakat A, El Sherbini SA, Fawzy HM. Prevalence of overweight and obesity in primary school children in Port Said city. Gaz Egypt Paediatr Assoc. 2013;61:31–6.
Taha AA, Marawan HM. Socio-behavioral determinants of overweight and obesity in Egyptian primary school children. J. Child Adolesc. Behav. 2015;3:236.
Ogden CL, Carroll MD, Flegal KM. Epidemiologic trends in overweight and obesity. Endocrinol. Metab. Clin. N. Am. 2003;32:741–60.
Wrotniak BH, Epstein LH, Dorn JM, Jones KE, Kondilis VA. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006;118:e1758–65.
Gallahue D, Donnely F. Developmental physical education for all children Champaign, IL: Human Kinetics; 2003.
Timmons BW, LeBlanc AG, Carson V, Connor-Gorber S, Dillman C, Janssen I, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37:773–92.
Hopkins B, Geangu E, Linkenauger S. The Cambridge Encyclopedia of child Development. 2nd ed: Cambridge University Press; 2017.
World Health Organization (WHO). Inheriting a sustainable world? Atlas on Children’s Health and the Environment. Geneva: WHO; 2017.
Kambas A, Michalopoulou M, Fatouros I, Christoforidis C, Manthou E, Giannakidou D, et al. The relationship between motor proficiency and pedometer-determined physical activity in young children. Pediatr Exer Sci. 2012;24:34–44.
Bruininks RH. Bruininks-Oseretsky test of motor proficiency: examiners manual. Circle Pines: American Guidance service; 1978.
Okely AD, Booth ML, Chey T. Relationships between body composition and fundamental movement skills among children and adolescents. Res. Q. Exerc. Sport. 2004;75:238–47.
Graf C, Koch B, Kretschmann-Kandel E, et al. Correlation between BMI, leisure habits and motor abilities in childhood (CHILT-Project). Int. J. Obes. Relat. Metab. Disord. 2004;28:22–6.
Cliff DP, Okely AD, Morgan PJ, Jones RA, Steele JR, Baur LA. Profi-ciency deficiency: mastery of fundamental movement skills and skill components in overweight and obese children. Obesity. 2012;20:1024–33.
Balli OM. Motor proficiency and body mass index of preschool children: in relation to socioeconomic status. J Educ Train Stud. 2016;4(4):237–43.
D’Hondt E, Deforche B, De Bourdeaudhuij I, Lenoir M. Relationship between Motor skill and body mass index in 5- to 10- year old children. Adapt. Phys. Activ. Q. 2009;26:21–37.
Siahkouhian M, Mahmoodi H, Salehi M. Relationship between fundamental movement skills and body mass index in 7 to 8 year-old children. World Appl Scencesi J. 2011;15(9):1354–60.
Lopes VP, Stodden DF, Bianchi MM, Maia JAR, Rodrigues LP. Correlation between BMI and motor coordination in children. J Sci Med Sport. 2012;15:38–43.
Logan SW, Scrabis-Fletcher K, Modlesky C, Getchell N. The relationship between motor skill proficiency and body mass index in preschool children. Res Q Exer Sport. 2011;82(3):442–8.
Nervik D, Martin K, Rundquist P, Cleland J. The relationship between body mass index and gross motor development in children aged 3 to 5, years. Pediatr Phys Therapy. 2011;23:144–8.
Hassan NE, El-Masry SA, Farid T, Khalil A. Influence of parental and some demographic characteristics on overweight/obesity status among a sample of Egyptian children. Open Access Maced. J. Med. Sci. 2016;4:342–7.
Abdelkarim O, Ammar A, Soliman AMA, Hökelmann A. Prevalence of overweight and obesity associated with the levels of physical fitness among primary school age children in Assiut city. Egypt. Pediatr. Assoc. Gaz. 2017;65:43–8.
Talat MA, El Shahat E. Prevalence of overweight and obesity among preparatory school adolescents in Urban Sharkia Governorate, Egypt Dietz WH. Overweight in childhood and adolescence. Egypt. Pediatr. Assoc. Gaz. 2016;64:20–5.
Hadhood SESA, Ali RAE, Mohamed MM, Mohammed ES. Prevalence and correlates of overweight and obesity among school children in Sohag. Egypt. Open J. Gastroenterol. 2017;7:75–88.
Abdelkarim O, Ammar A, Trabelsi K, Cthourou H, Jekauc D, Irandaust K, et al. Prevalence of underweight and overweight and its association with physical fitness in Egyptian schoolchildren. Int. J. Environ. Res. Public Health. 2020;17:75.
Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat. 2002;11(246).
Bruininks RH, Bruininks BD. Manual of Bruininks-Oseretsky Test of Motor Proficiency. 2nd ed: PsychCorp; 2005.
Tecklin JS. Pediatric physical therapy. 5th ed. Philadelphia: lippinacott Williams and Wilkins; 2015.
Möller S, Poulain T, Körner A, Meigen C, Jurkutat A, Vogel M, et al. Motor skills in relation to body-mass index, physical activity, TV-watching, and socioeconomic status in German four-to-17-year-old children. PLoS ONE. 2021;16(5):e0251738. https://doi.org/10.1371/journal.pone.0251738.
Cheng J, East P, Blanco E, Kang ES, Castillo M, Lozoff B, et al. Obesity leads to declines in motor skills across childhood. Child Care Health Dev. 2016;42(3):343–50.
Hamilton M, Liu T, ElGarhy S. The Relationship between body weight and motor skill competence in Hispanic low-SES preschool children. Early Childhood Educ J. 2017;45:529–35.
Stodden DF, Goodway JD, Langendorfer SJ, et al. A developmental perspective on the role of motor skill competence in physical activity: a emergent relationship.p. Quest. 2008;60:290–306.
Biro FM, Wien M. Childhood obesity and adult morbidities. Am. J. Clin. Nutr. 2010;91:1499–505.
Musaiger AO. Overweight and obesity in Eastern Mediterranean region: prevalence and possible causes. J. Obes. 2011;2011:407237.
El-Bayoumy I, Shady I, Lotfy H. Prevalence of obesity among adolescents (10 to 14 years) in Kuwait. Asia Pac. J. Public Health. 2009;21:153–9.
World Health Organization (WHO). Diet, nutrition and prevention of chronic diseases—report of aJoint WHO/FAO Expert Consultation. Geneva: WHO; 2003.
Abdelkarim O, Ammar A, Chtourou H, et al. A comparative study of physical fitness among Egyptian and German children aged between 6 and 10 years. Adv Phys Edu. 2015;5:7–17.
Gentier I, D’Hondt E, Shultz S, Deforche B, Augustijn M, Hoorne S, et al. Fine and gross motor skills differ between healthy-weight and obese children. Res Dev Disabil. 2013;34:4043–51.
Abdel-Aziz EA, Hmza RT, Youssef AM, Mohamed FM. Health related quality of life and psychological problems in Egyptian children with simple obesity in relation to body mass index. Egypt J Med Hum Genet. 2014;15:149–54.
Haywood K, Getchell N. Life span motor development. Champaign, IL: Human Kinetics; 2005.
Southall JE, Okely AD, Steele JR. Actual and perceived physical competence in overweight and nonoverweight children. Pediatr Exerc Sci. 2004;16:15–24.
Cairney J, Hay JA, Veldhuizen S, Missiuna C, Faught BE. Developmental coordination disorder, sex, and activity deficit over time: a longitudinal analysis of participation trajectories in children with and without coordination difficulties. Dev. Med. Child Neurol. 2010;52:e67–72.
Acknowledgements
We appreciate the role of children who participated in this study and their parents.
Funding
Nil
Author information
Authors and Affiliations
Contributions
The authors testify that both people named as authors are qualified to be authors. AMS designed the study, conducted research, and collected and organized the data. YMA analyzed and interpreted data and provided logistic support. Both authors wrote the initial and final drafts of the article; also, they were in charge of the content of manuscript and similarity index after critically reviewing and approving the final text.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval from the Faculty of Physical Therapy, Cairo University, Egypt (no.: P.T.REC/012/003400), and a signed written consent form with parent acceptance for participation in the study and publication of the results were obtained before starting the study procedures.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Bruininks-Oseretsky Test 2 of Motor Proficiency Short Form (BOT-2 SF)

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Awad, A.S., Aneis, Y.M. Correlation between body mass index and motor proficiency in Egyptian children: a cross-sectional study. Bull Fac Phys Ther 27, 26 (2022). https://doi.org/10.1186/s43161-022-00087-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43161-022-00087-7