Abstract
Background
Chylolymphatic cysts are benign pathology in lymphatic vessels due to obstruction in the lymphatic system. Their incidence is still unknown. However, they account for approximately 3 to 9% of all pediatric lymphangiomas. Most of these lesions are asymptomatic and are discovered accidentally. They can be presented with nonspecific abdominal pain, vomiting, and changes in bowel habits. Rarely, chylolymphatic cysts can as intestinal obstruction, volvulus or even torsion.
Case presentation
A 3-month-old male presented to our unit with manifestations of acute intestinal obstruction. Abdominal examination revealed signs of generalized peritonitis and intestinal obstruction. Abdominal ultrasound revealed minimal turbid intraperitoneal collections and no motility of bowel loops. Plain erect abdominal radiograph revealed multiple small bowel air fluid levels. Abdominal exploration revealed a large chylolymphatic cyst causing acute intestinal obstruction. Excision of the cysts was done with preservation of adjacent bowel loop. The patient was discharged in good health on the 6th day postoperative. A chylolymphatic cyst with a diameter of 5 cm was identified by histological investigation.
Conclusions
Most chylolymphatic cysts in infants are asymptomatic, but they can cause fatal complications such as intestinal obstruction, volvulus, or even torsion.
Similar content being viewed by others
Background
Chylolymphatic cysts are benign pathology in lymphatic vessels due to obstruction in the lymphatic system. Their incidence is still unknown [1]. However, they account for approximately 3 to 9% of all pediatric lymphangiomas [2]. Most of these lesions are asymptomatic and are discovered accidentally. They can be presented with nonspecific abdominal pain, vomiting, and changes in bowel habits. Rarely, chylolymphatic cysts can as intestinal obstruction, volvulus, or even torsion [3].
Case description
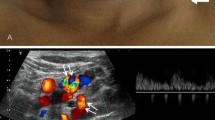
A 3-month-old male presented to our unit with his mother complaining of repeated bilious vomiting, abdominal distension, and absolute constipation for 2 days. General examination revealed toxic look of the infant and moderate dehydration. He had a temperature of 38.5 °C, respiratory rate of 34 breaths per minute, and pulse of 160 bpm, and his blood pressure was 70/40 mmHg. Abdominal examination revealed stepladder appearance of bowel loops, diffuse guarding, and empty rectum. The rest of the examination was unremarkable. After resuscitation with intravenous fluids and empirical antibiotics, a 10-French nasogastric tube was inserted. A white blood cell count showed a leukocytosis of 18,000 cells/mm3 with a neutrophilic predominance of 15,500 cells/mm3. We requested urgent abdominal ultrasound, which revealed minimal turbid intraperitoneal collections and no motility of bowel loops. Plain erect abdominal radiograph revealed multiple small bowel air fluid levels with no free air under diaphragm (Fig. 1). We prepared the infant for urgent abdominal exploration. Via right transverse supra umbilical incision, we performed formal abdominal exploration that revealed highly turbid fluid collection and a large multilocular chylolymphatic cyst adjacent to a jejunal loop 30 cm far from duodenojejunal junction causing intestinal obstruction (Fig. 2). Excision of the cysts was done with preservation of adjacent bowel loop (Fig. 3). Repair of a small mesenteric defect at the bed of the cyst was done with serosal repair of mesenteric border of adjacent jejunal loop (Fig. 4a, b). Peritoneal lavage was done, and a pelvic drain was inserted. The patient was discharged in good health on the 6th day postoperative. A chylolymphatic cyst with a diameter of 5 cm has been identified by histological investigation.
Discussion
Mesenteric cyst is a rare intra-abdominal tumor with prevalence of about 1:20,000 in pediatric age group. Chylolymphatic cysts are rare variants of mesenteric cysts; they account for 3 to 9.2% of all pediatric lymphangiomas [2].
They are benign cystic pathology lined with a thin endothelium or mesothelium that occurred due to gross proliferation of isolated or ectopic lymphatics in mesentery that lack communication with the rest of the lymphatic system. The accumulation in these channels results from an imbalance between the inflow and outflow of fluid [1]. They can occur in any part of the mesentery of the gastrointestinal tract but most commonly are localized in the mesentery of the small intestine, large intestine, and retroperitoneum. They can be single or multiple and unilocular or multilocular and can have serous, chylous, hemorrhagic, or mixed fluid [4]. Our case had a single multilocular chylolymphatic cyst in the mesentery of proximal jejunum.
Based on their etiology, Beahrs et al. [2] classified mesenteric cysts into embryonic or developmental, traumatic, or acquired, neoplastic, or non-neoplastic and infective or degenerative. Based on their contents, mesenteric cysts can be divided into serous, chylous, hemorrhagic, and chylolymphatic cyst. Regarding pathology, mesenteric cysts are classified into four types including type 1 (pedicled) and type 2 (sessile), which are limited to the mesentery, hence can be excised completely with or without resection of the involved gut. Type 3 and type 4 are multicentric, so they require complex surgery and often sclerotherapy because of their extension into retroperitoneum [3]. This case is type 2 (sessile) chylolymphatic cyst.
Most of mesenteric cysts may present as asymptomatic abdominal mass or incidental finding on imaging or laparotomy for other abdominal conditions. In rare occasions, mesenteric cysts may cause acute abdomen from cyst rupture, infection, hemorrhage, intestinal obstruction, and volvulus [5]. In our case, a large chylolymphatic cyst presented as acute intestinal obstruction.
Preoperative diagnosis of mesenteric cyst in most cases is difficult as they have no definite characteristic features. Abdominal ultrasound which is the imaging modality of choice can reveal mesenteric cysts as cystic tumors [6]. Plain X-ray abdomen may show gasless, homogenous mass displacing bowel loops. Multiple air fluid levels may be seen in erect film [5]. Computed tomography can be also used to confirm the diagnosis [3]. In our case, preoperative plain radiograph revealed multiple air fluid levels due to compression and inflammatory adhesion caused by a large multilocular chylolymphatic cyst. Postoperative diagnosis is confirmed with histopathology, which can differentiate the chylolymphatic cyst from other mesenteric cysts [3].
Surgical removal of the cyst is the standard treatment for chylolymphatic cysts. The cyst is removed along with the adjacent bowel loop. Enucleation and cyst drainage were two more techniques mentioned [7]. We just remove the cyst in our case.
Conclusions
Most chylolymphatic cysts in children are asymptomatic, but they can cause fatal complications as intestinal obstruction, volvulus, or even torsion.
Availability of data and materials
Data sharing is not applicable to this article.
References
Javed A, Pal S, Chattopadhyay TK. Chylolymphatic cysts of the mesentery. Trop Gastroenterol. 2011;32(3):219–21.
Ricketts RR. Mesenteric and omental cysts. Pediatric surgery: Elsevier; 2012. p. 1165–70.
Rattan KN, Nair VJ, Pathak M, Kumar S. Pediatric chylolymphatic mesenteric cyst - a separate entity from cystic lymphangioma: a case series. J Med Case Rep. 2009;3:111.
Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg. 1985;120(11):1266–9.
Sahin DA, Akbulut G, Saykol V, San O, Tokyol C, Dilek ON. Laparoscopic enucleation of mesenteric cyst: a case report. Mt Sinai J Med. 2006;73(7):1019–20.
Sehrawat R, Bansal N, Kour H, Sinha A. A giant pediatric chylolymphatic cyst: an extremely rare entity. JPGN Rep. 2023;4(1):e274.
Hebra A, Brown MF, McGeehin KM, Ross AJ 3rd. Mesenteric, omental, and retroperitoneal cysts in children: a clinical study of 22 cases. South Med J. 1993;86(2):173–6.
Acknowledgements
The authors would like to thank the child’s parents for permission to share their child’s medical histories for educational purposes and publication.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
AKA contributed to management and wrote the manuscript. TAS contributed to acquisition of data and revision of manuscript. AKA and TAS were the surgeon who operated this case. AHM was the anesthesiologist. AKA and IMA, critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval no. E9854 from Assiut University Ethics Committee was taken. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor in chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, A.K., Abdelhamid, I.M., Mohamed, A.H. et al. Chylolymphatic cyst as a rare cause of acute intestinal obstruction in infants. Ann Pediatr Surg 19, 33 (2023). https://doi.org/10.1186/s43159-023-00264-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-023-00264-w