Abstract
Background
Long waiting time (WT) for elective surgery is a frequent and important issue in many countries. This study examined the factors affecting the WT for elective surgery in a paediatric surgery department in a tertiary healthcare hospital in Niger, Africa. This descriptive retrospective study examined patients aged 0–15 years who underwent elective surgery in the paediatric surgery department of National Hospital Amirou Boubacar Diallo in Niamey, Niger, between April 1, 2019 and March 30, 2020. Socio-demographic, diagnostic, and therapeutic data were collected from medical records, and the WT, defined as the number of days between when surgery was proposed and performed was analysed. Statistical analyses were performed with the Kruskal–Wallis test, and a p < 0.05 was considered statistically significant.
Results
Three hundred fifty-four patients were included in the study. The umbilical hernia was the most common surgical indication (n = 103, 29.1%). The mean WT was 69.2 days (range, 8 days–11.3 months), and the majority of patients had a WT of less than two months (n = 240, 67.8%). Depending on the surgical indication, the mean WT ranged from 13 days (posterior urethral valve) to 8.5 months (epispadias). WT was significantly longer among patients living in rural areas (p = 0.012), with comorbidities (p = 0.0034), and whose procedures were postponed (p = 0.0026).
Conclusion
Patient and institution-related factors influenced the WT. It can be reduced by addressing the supply and demand aspects of surgical care, as well as by prioritising patients who need more urgent care.
Similar content being viewed by others
Background
The waiting time (WT) for elective surgery is defined as the time period between when a surgical procedure was proposed and performed [1]. In some countries, the overall WT also includes the outpatient WT, which refers to the time period between the referral from a general practitioner to a surgeon [2]. WT is one of the parameters by which the performance of healthcare systems and quality of care can be measured [3].
Long WTs are observed in most healthcare systems and occur when the demand for surgical care exceeds the supply [2]. While there is no consensus on what constitutes excessive or long WT, long WT for elective surgery is an important health policy concern [2]. Long WTs also reduce the therapeutic benefit of surgery, as well as promote distress and financial difficulties among patients who cannot undergo the necessary surgical treatment. Population and policy-makers can consider long WT as an inefficiency of the health care system to delivery and planning of health care [2, 4, 5].
Several countries have developed programs to reduce the excessive WT for elective surgeries [6, 7] by managing the supply and demand of surgical care; however, only a few studies have analysed WT for elective surgery in a paediatric population [8,9,10]. This study evaluated the WT for elective procedures in the paediatric surgery department of the National Hospital Amirou Boubacar Diallo in Niamey, Niger.
Methods
Context
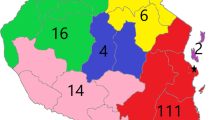
The paediatric surgery department of the National Hospital Amirou Boubacar Diallo is one of two paediatric surgery departments in Niger. The department has 36 beds, one dedicated operating room, and three paediatric surgeons on staff. In our hospital, conditions that usually require day surgery are managed with short-stay surgeries, which involve 24–72 h of hospitalisation. Short-stay surgeries are organised and integrated with the other types of scheduled surgeries.
Methodology
This was a retrospective descriptive study. It was approved by the Research ethics board of the hospital. Written informed consent for participation in this study was obtained from all parents or legal guardians of patients included in the study. Patients aged 0–15 years who underwent elective procedures in the paediatric surgery department of the National Hospital Amirou Boubacar Diallo in Niamey, Niger, between April 1, 2019 and March 30, 2020 were included in this study. Data, such as age, sex, place of residence, diagnosis, comorbidities, surgical indication, date when the surgery was proposed, date of the pre-anaesthetic consultation, date of hospitalisation, the reason for the postponement of surgery, and date of the actual surgery, were collected from medical records.
We defined overall WT as the number of days between when the surgical intervention was proposed and when the procedure was performed (Fig. 1). WT1 was defined as the number of days between when the surgery was proposed and the first pre-anaesthetic consultation. WT2 was defined as the number of days between the first pre-anaesthetic consultation and hospitalisation. WT3 was defined as the number of days between hospitalisation and the final surgery. We also determined whether any patients developed disease-related complications requiring emergency surgery during their WTs.
Statistical analysis
The Kruskal–Wallis test was used to compare the mean WT with different variables. The threshold for statistical significance was set at a p-value < 0.05.
Results
A total of 354 patients were analysed in the study, which comprised 59.7% of the department's hospitalisation for the study period (n = 592). There were no cases of patients operated on emergency for a complication of her / his pathology for which she/ he was awaiting intervention in elective surgery.
The mean age of our patients was 3.95 years (range, 3 months to 15 years). The majority of patients were 3–5 years of age (n = 136, 38.4%) and male (n = 252, 71%); the male-to-female ratio was 2.57. The majority of patients lived in rural areas (n = 259, 73.1%), whereas only a minority lived in urban areas (n = 95, 26.9%). Seventy-four (20.8%) patients had comorbidities, of which anaemia was the most common; anaemia was documented in 55 (74.3%) of the cases. A preoperative blood transfusion was required in 29 (52.7%) of the patients with anaemia. Malaria and urinary tract and pulmonary infections comprised 6 (6.8%) and 14 (18.9%), respectively, of the other comorbidities.
The most common pathology requiring surgical intervention was an umbilical hernia, of which 103 (29%) cases were documented (Table 1). Twenty-five (7.1%) of these cases were postponed because the operating room had to be prioritised for an emergency procedure (n = 13), medical supplies for the intervention were not purchased (n = 4), bed in the postoperative department was unavailable (n = 4), patient was not cleared for surgery (n = 3), and diagnosis changed (n = 1).
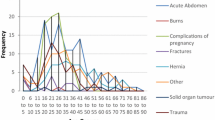
The mean WT was 69.2 days (range, 8–340). The majority of patients (n = 240, 67.8%) had a WT < 60 days (Fig. 2). The mean WT1 was 52.1 days (range, 5–180), and WT1 constituted 75.2% of the overall WT (Table 2).
The mean WT for patients residing in rural areas was significantly longer than for those residing in urban areas (73.9 days vs. 56.9 days, p = 0.012). Depending on the disease, the mean WT ranged from 13–255 days (8.5 months) (Table 3). The mean WT for patients with comorbidities was significantly longer than in patients without comorbidities (100.9 days vs. 69 days, p = 0.0034). The mean WT for patients whose procedures were postponed was significantly longer than for patients whose procedures were not postponed (132.9 days vs. 64.6 days, p = 0.0026). None of the patients developed disease-related complications requiring emergency surgery during their WTs.
Discussion
Although the waiting time has been assessed and characterised, our study has limitations. Regarding the research design limitations, the study was realized during a relatively short period and was monocentric. The time period between referral from primary care provider to consultation with a paediatric surgeon, has not included in the overall waiting time. This time period could be very variable and influenced by multiple factors linked to the patient and his or her entourage or to the health structures that refer the patient.
Concerning the impact limitations of the results, some specificities in our practice can influence the WT and so limitate the transposability of our results: frequencies of conditions, differences for the surgical indication, realisation of pre-anaesthetic consultation, and reception capacities of the department. Waiting time may be also significantly influenced by social and economic factors.
The mean WT mean in our study was 69.2 days, and most patients (62.6%) had a WT of less than two months. A WT of 3–6 months for surgery is regarded as excessive by several Organisation for Economic Co‑operation and Development (OECD) countries [2, 11].
The longest delay in our patients was during the time between when the surgery was proposed and the first pre-anaesthetic visit. Our institution offers a limited number of pre-anaesthetic consultations each week. Acquiring the proper laboratory tests for the pre-anaesthetic consultation may have also contributed to the delay in patient management.
In our study, WTs varied greatly depending on the patient’s condition to another. WTs do not always correspond with the severity of the patient’s condition [1]. The Saskatchewan classification system was established by a panel of Canadian paediatric surgeons and proposed WTs for certain conditions [1, 12]. Our study identified 22 conditions; the WT for 11 of these conditions exceeded the acceptable WT recommended by the Saskatchewan classification system. These 11 conditions had the shortest recommended WTs (Table 3).
A Canadian study that evaluated WTs according to the same classification system demonstrated that 27% of paediatric patients underwent surgery after the recommended waiting period [13]; however, it was difficult to compare waiting times between studies because the surgical management differed between study populations. For example, we treated anorectal malformations and omphaloceles beyond the neonatal period because our anaesthesia and intensive care departments were not equipped to handle these cases at an earlier age.
None of our patients required emergency surgery for disease-related complications. In contrast, a multicentre study established a correlation between long WTs for inguinal hernia repair and a higher incidence of hernia incarceration or emergency department visits [8]. A longer study in our department could certainly better assess the risk of complications when the waiting time is too long.
Our study identified several factors that contributed to longer WTs. Patients living in rural areas may have had significantly longer WT because the distance made it difficult for them to access our service. Moreover, the financial burden for traveling and other expenses, as well as the lack of people and places in town for receiving the patient and his family, may have forced families to return home prior to receiving complete care. The accessibility of paediatric surgical departments is a major issue in Africa because one-third of the population lives in rural areas, whereas 90% of paediatric surgeons practice in tertiary healthcare institutions located in the major cities [14].
Patients with comorbidities had significantly longer mean WT (100.9 days) than patients without comorbidities because comorbidities had to be managed prior to surgery, which compounded the total WT. Patients with more severe conditions likely had more comorbidities, which explained why these patients also had relatively longer mean WT compared with patients with less severe conditions. For example, patients with Hirschsprung’s disease had a mean WT of 84.4 days, whereas patients with hydroceles had a mean WT of 39.9 days. Among patients with anaemia requiring transfusion, the lack of blood products was identified as a key factor in prolonging WT [3].
The postponement of surgery also had a significant impact on the WT of our patients. The reasons for postponement are multifactorial [15]. In our study procedures were mostly postponed because the operating theatre was unavailable. In other studies there was also a too short operating time [3, 15]. Surgery is also commonly delayed when patients with respiratory infections or uncontrolled comorbidities cannot be cleared for surgery [15].
The combination of two phenomena favours the occurrence of long WTs: a supply of care limited by insufficient resources of the health system; a demand for care favoured by no or low patient participation in the costs of care [2]. Since 2006, patients up to 5 years of age in Niger are assured free access to healthcare; however, in public healthcare infrastructures there is a lack of human and material resources [16].
Some of the surgical indications in our study are managed with day surgery in other countries. In Nigeria and several OECD countries, day surgery constitutes more than 50% of all surgical activities [2, 9]. Day surgery development has been one of the solutions that proved effective in reducing significantly the surgical WT [6].
Overall, long WTs for elective procedures can be reduced by expanding care capacity, rationing and/or prioritising demand, and restructuring the intake assessment and/or referral process [4]. While augmenting health care supply with the appropriate human and material resources, it is necessary but not enough; reducing WT by acting on the demand of care is a more economic measure [17, 18]. In our context a second operating room is building and the department is the site of formation of paediatric surgeon. A waiting list for pre-anaesthetic consultation could also be established. Better patient management protocols in surgical departments should also be considered. An Indian study demonstrated that 39% of elective procedures were cancelled for preventable reasons [15]. Establishing a priority list with explicit guidelines may partially reduce the WT for patients with the most serious conditions [2, 4]. The priority list should account for the severity of the patient’s condition and his area of residence.
Conclusions
WT varied depending on the surgical indication. Patient- (area of residence, comorbidities) and institution-related factors (unavailable operating rooms) also influenced the overall WT. While the characteristics and consequences of long WTs in our department remained unclear, establishing new protocols and managing how surgical care is provided are of topmost priority.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- WT:
-
Waiting times
- OECD:
-
Organisation for Economic Co-operation and Development
References
Wright J. Development of pediatric wait time access targets. Can J Surg. 54(2): 107‑10. https://doi.org/10.1503/cjs.048409.
-Hurst J, Siciliani L. Tackling Excessive Waiting Times for Elective Surgery: A Comparison of Policies in Twelve OECD Countries. Paris: OECD Health Working Papers; 2003. Available from: http://www.oecd.org/els/health‑systems/5162353.pdf. [Last accessed on 14 Sep 2020].
Musonda M, Choolwe J, Jean R, Jakub G, Chiara P, Cheelo M. Factors Associated with Waiting Time for Patients Scheduled for Elective Surgical Procedures at the University Teaching Hospital (UTH) in Zambia. Ann Med Health Sci Res. 2020;10:1040–5.
Ballini L, Negro A, Maltoni S, Vignatelli L, Flodgren G, Simera I, et al. Interventions to reduce waiting times for elective procedures. Cochrane Database Syst Rev. 2015;23(2):CD005610. https://doi.org/10.1002/14651858. (CD005610.pub2).
Kreindler SA. Policy strategies to reduce waits for elective care: A synthesis of international evidence. Br Med Bull. 2010;95(1):7–32. https://doi.org/10.1093/bmb/ldq014.
Caldinhas PM, Ferrinho P. Day-surgery and surgical waiting time. Rev Bras Epidemiol. 2013;16(2):314–27. https://doi.org/10.1590/S1415-790X2013000200008.
Fixler T, Menaker RJ, Blair GK, Wright JG. Pediatric surgical capacity and demand: analysis reveals a modest gap in capacity and additional efficiency opportunities. Healthc Q. 2011;14 Spec No 3:28–34.
Chen LE, Zamakhshary M, Foglia RP, Coplen DE, Langer JC. Impact of wait time on outcome for inguinal hernia repair in infants. Pediatr Surg Int. 2009;25(3):223–7. https://doi.org/10.1007/s00383-013-3429-y.
Abdur-Rahman LO, Kolawole IK, Adeniran JO, Nasir AA, Taiwo JO, Odi T. Pediatric day case surgery: experience from a tertiary health institution in Nigeria. Ann Afr Med sept. 2009;8(3):163–7.
Ali Ada MO, Moustapha H, Habou O, Abarchi H. Waiting time for short-stay surgery in a pediatric surgery department. Afr J Paediatr Surg. 2021;18:39–42.
Waddell JP. Improving waiting times for surgery. Can J Surg. 2008;51(5):333–4.
OCHN - Surgical Services Wait Time Task Force April 19, 2007 - O. Appendix 1 to Wright JG, Li K, Seguin C, et al. Development of pediatric wait time access [cited 22 june 2021]. Available on: http://canjsurg.ca/wp-content/uploads/2014/02/54-2-107app1.pdf.
Wright JG, Menaker RJ. Waiting for children’s surgery in Canada: the Canadian Paediatric Surgical Wait Times project. CMAJ. 2011;183(9):E559–64.
Chirdan LB, Ameh EA, Abantanga FA, Sidler D, Elhalaby EA. Challenges of training and delivery of pediatric surgical services in Africa. J Pediatr Surg. 2010;45:610–8.
Bathla S, Mohta A, Gupta A, Kamal G. Cancellation of elective cases in pediatric surgery: An audit. 2010;15(3):90–2.
-Institut National de la Satistique Direction des Statistiques et des Etudes Démographiques et Sociales. Etude sur la gratuité des soins de santé au Niger; 2015. Available from: http://www.statniger.org/statistique/file/DSEDS/Rapport_Etude_gratuite_soins_Sante.pdf. [Last accessed on 9 Oct 2020].
Gawad N, Davies DA, Langer JC. Determinants of wait time for infant inguinal hernia repair in a Canadian children’s hospital. J Pediatr Surg. 2014;49(5):766–9. https://doi.org/10.1016/j.jpedsurg.2014.02.064.
Aiono S, Faber RG, Galland RB. Surgeons have little control over general surgical waiting lists. Ann R Coll Surg Engl. 2000;82:304–7.
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
MOAA: Designing the study and collecting data and final approval of the version. HM: Review the written material and edited. OH: Interpretation of data. IASE: Collection analysis of data. SI: Organizing data. HA: Revising critically. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research ethics board of the hospital (reference number is not available). A written informed consent for participation at this study was obtained from all parents or legal guardians of participants included in the study.
Consent for publication
Not applicable.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ada, M.O.A., Moustapha, H., Habou, O. et al. Waiting times for elective surgery in an African paediatric surgery department. Ann Pediatr Surg 19, 24 (2023). https://doi.org/10.1186/s43159-023-00257-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-023-00257-9