Abstract
Background
Gastrointestinal (GI) tract bezoars are aggregates or concretions of inedible and undigested material mostly found in the stomach but can also be found elsewhere in the gastrointestinal tract. Trichobezoar, an infrequent form of bezoar seen mostly in young females, consists of a compact mass of swallowed hair. It is primarily located in the stomach but may extend through the pylorus into the duodenum and small bowel, a condition labelled as Rapunzel syndrome.
Cases presentation
In this series, we report four consecutive cases of trichobezoars in the paediatric age group, all managed at a single institution King Saud Medical City Hospital Riyadh between 2019 and 2022. All the cases were girls between the ages of ten to fourteen with psychosocial problems. All the patients had a definite mass in the epigastrium and a history of not gaining weight. One presented with intestinal obstruction. X-ray abdomen and computed tomography (CT) scan abdomen were the imaging modalities that led to the diagnosis. All patients underwent surgery with successful removal of the trichobezoar and were referred to a psychiatrist for evaluation and treatment of a psychological disorder.
Conclusion
Trichobezoar is a rare entity that should be considered as a differential diagnosis in young female patients with vague, non-specific clinical symptoms and a palpable, upper-abdominal mass. In our experience and in line with the published literature, conventional laparotomy is still the gold standard in cases of GI trichobezoars.
Along with the removal of the trichobezoar, treatment of the existing psycho-social ailment is of utmost importance and needs long-term counselling with periodic psychological evaluation in follow-up clinics to avoid recurrence.
Similar content being viewed by others
Background
Bezoars are aggregates of indigestible swallowed foreign material retained in the gastrointestinal tract [1,2,3,4]. The word “bezoar” is derived from the Arabic word “bedzehr” or the Persian word “padzhar” meaning antidote [1, 5]. In history, bezoars removed from animals’ stomachs or intestines were used as precious stones with medicinal properties, antidotes to poisons, and today as part of traditional Chinese medicine [4]. The first reference to a bezoar in humans was reported in 1779 which was found during an autopsy of a patient who died from gastric perforation and subsequent peritonitis [4]. Many types of bezoars have been described in the literature as per their composition, including phytobezoar (fibres from plants, vegetables, and fruit), trichobezoar (hair), lactobezoar (milk protein), and medications (pharmacobezoars) etc [1, 2].
GI trichobezoar is a compact aggregate mass of swallowed hair and constitutes less than 6% of all bezoars [1,2,3], and mostly affects young females [1, 6, 7]. Up to 90% of cases have been reported in females in the age group between 13 and 20 years [4] with habits of trichotillomania (hair-pulling) and trichophagia (hair-ingesting: not only of one’s own hair but also of others, such as family members’ or toy dolls’) commonly observed in psychiatric disorders [1,2,3,4, 8, 9]. Human hair is resistant to digestion and owing to its smooth slippery surface, accumulates between mucosal folds of the stomach [2,3,4]. With continuous trichophagia over a period, the swallowed hair entangles together with mucus and food particles and is enmeshed into a ball that gradually assumes the shape of a stomach [2, 4]. The acidic content of the stomach denatures hair protein and gives trichobezoar its black colour and subsequent colonization by bacteria results in halitosis in patient [4, 5]. Trichobezoars usually reside in the stomach but rarely may pass to the small bowel as isolated or satellite concurrent small bowel bezoars and cause intestinal obstruction [2,3,4,5,6,7,8,9,10,11,12]. Rapunzel syndrome is a rare type of trichobezoar, first described by Vaughan et al. in 1968 [4,5,6, 9], in which there is a tail-like extension of gastric trichobezoar which may extend through the pylorus into the small intestine or even colon [3,4,5, 9, 13,14,15,16,17].
In this study, we are sharing our experience of three cases of gastric trichobezoar and one case of isolated small bowel trichobezoars who presented with acute abdomen, an extremely rare presentation.
Case presentation
A 10-year-old girl presented to the emergency department with a 1-month history of colicky central abdominal pain that worsened 3 days prior to the presentation. The pain was associated with early satiety and the gradual appearance of a lump in the upper abdomen. There was a history of weight loss but no history of associated vomiting, constipation, diarrhoea, rectal bleeding, or urinary symptoms. There was an initial denial of history related to trichophagia and trichotillomania.
In the past surgical history, she had laparoscopic cholecystectomy 4 years back secondary to gallstones and had an upper gastrointestinal endoscopy 3 and a half years back for chronic abdominal pain and was diagnosed as gastritis after gastric biopsy and was treated medically. There was no psychiatric illness in the past, and no relevant family history of any medical or psychiatric illness. Her immunization status was up to date. Although she achieved all typical developmental milestones of her age, she had a low to average school performance. Her intelligence quotient (IQ) score was 85 on the Stanford-Binet intelligence scale [18], which corresponds to average intellectual performance. She lived with her parents and five siblings, all of whom were healthy. She was the youngest of all with a significant age difference from her siblings. As per her mother, she mostly sat alone and used to play by herself and had less parental attention. Her family belonged to an average socioeconomic background.
On examination, she was thin built, weight 31 kg which put her below the 5th percentile for her age. There was no apparent baldness or thinning of hairs. She was vitally stable.
Upon abdominal examination, there was a visible bulge in the epigastrium and left upper quadrant. On palpation, there was a firm non-tender sausage-shaped mass approximately 15 × 8 cm in the left upper quadrant and epigastrium, which was slightly mobile. The rest of the abdomen was soft.
Her complete blood counts showed haemoglobin of 13.3 g/dl, with normal white blood cells count. In addition, the kidney function test, liver function test, and urine analysis were within normal limits.
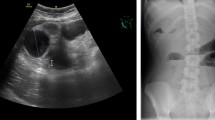
Ultrasound abdomen was done and showed a significantly dilated stomach with posterior acoustic shadowing- suggestive of bezoar. There were no significant abdominopelvic ascites or collections. CT scan of the abdomen showed a huge, heterogeneous, non-enhancing mass occupying and filling the gastric cavity- suggestive of a massive gastric bezoar (Fig. 1a). There was a slight gastric mucosal wall enhancement, suggestive of a thick gastric wall but no focal mass lesion. The large and small bowel loops were grossly unremarkable with no bowel dilatation.
An exploratory laparotomy was done through the upper midline incision. Per-operatively, a dilated stomach with a mass of trichobezoar taking the shape of the stomach was found and was removed through anterior gastrotomy (Fig. 1b, c). There was no extension of the bezoar into the duodenum or as separate satellite masses in distal bowel loops. The postoperative course was unremarkable.
Paediatric psychiatric consultation was also sought, and on the retrospective inquiry of the mother, there was a history of on and off trichophagia and trichotillomania. The patient was discharged in good health after counselling of patient and family with follow-up appointments in both paediatric surgery and paediatric psychologist clinics.
Case presentation
A 13-year-old female patient was referred to the emergency department with a history of intermittent abdominal pain for 4 months which increased in severity for a few days and was associated with bouts of yellowish-coloured vomiting. There was also a history of weight loss and a habit of eating hair. Upon examination, she was thin built with thinning of scalp hairs and vitally stable. Abdominal examination revealed upper abdominal distension with tenderness and a palpable mass in the epigastrium.
CT scan abdomen was suggestive of gastric trichobezoar. After initial optimization, exploratory laparotomy with anterior gastrotomy was done. A trichobezoar, which was extending into the duodenum (giant gastroduodenal trichobezoar), was removed (Fig. 2). There was no extension of the bezoar as separate satellite masses in distal bowel loops. The postoperative course was unremarkable.
Psychiatric consultation was done in the postoperative period alongside family and child counselling. The patient was discharged in good health with follow-up appointments for paediatric surgery and psychiatry clinics.
Case presentation
A 13-year-old female patient, medically free, was admitted through the emergency department with a history of intermittent abdominal pain for 3 months with weight loss. The pain became severe in intensity and persistent for 3 days and was associated with episodic, yellowish-coloured vomiting. The child was passing stool every other day and there was no associated history of rectal bleeding or urinary symptoms. There was also a history of thinning of scalp hairs.
On clinical examination, she was thin built. Abdominal examination revealed upper abdominal distension. It was soft on palpation with moderate tenderness in the centre of the abdomen. The patient was admitted for further workup. Laboratory work-up was done and found to be normal. X-ray abdomen showed a paucity of gas shadows with few air-fluid levels in the upper abdomen (Fig. 3a). CT scan abdomen raised suspicion of trichobezoars in the small intestine (Fig. 3b) suggestive of partial intestinal obstruction. After initial optimization, an exploratory laparotomy was done and two trichobezoar masses were found in the jejunum and proximal ileum (Fig. 3c–e). There were no concurrent masses in the stomach and duodenum. Ileal enterotomy was done, and both masses were removed from the same opening.
The postoperative course was unremarkable. On retrospective inquiry, there was a positive history of on and off trichophagia and trichotillomania. Psychiatric consultation and counselling of family and child were done. The patient was discharged with follow-up in the paediatric surgery and psychiatry clinics.
Case presentation
A 14-year-old female patient was referred from an outside hospital with a diagnosis of trichobezoar. She has a history of colicky abdominal pain associated with non-bilious vomiting after every feed for 1 week. There was no history of fever, urinary symptoms, or constipation. There was a history of early satiety and weight loss for the last 1 year. On inquiry from the mother regarding the patient’s psychosocial history, she has a quiet personality and is good in academics. She has 5 siblings and herself 3rd in order with some element of social issues with elder sisters. As per the patient herself, she does not remember when she started pulling and eating her hair. She was evaluated and worked up in referring hospital in terms of an ultrasound abdomen and CT scan abdomen that were suggestive of gastric bezoar. Upper GI endoscopy was also done which was suggestive of trichobezoar.
On examination, she was a thin-built patient with a weight of 56 kg and a height of 162 cm. There was no bald patch or thinning of hairs. Her abdominal examination revealed a hard mass in the epigastrium and left upper quadrant.
After initial optimization, exploratory laparotomy with anterior gastrotomy was done and a huge gastric trichobezoar approximately 25 cm removed from the stomach with its tail extending into the small bowel (Rapunzel syndrome) (Fig. 4).
Discussion
GI trichobezoars are extremely rare, and constitute 6% of all bezoars [3]. They are mostly seen in females in their teens with an unrevealed inciting psycho-social ailment [3, 4]. In our series, all four cases were female in the 10 to 14 years age group, with a history of trichotillomania and trichophagia. For all four cases, the parents were initially hesitant in sharing information about their children’s behavioural disorders suggestive of trichotillomania and trichophagia, but upon conciliation with the paediatric clinical psychologist, they revealed the information. There was no family history of any psychological problem in any of our cases, and all the patients showed average academic performance. We presume that in this age group shift from pre-teens to teens, there are numerous pressor factors that can incite such behavioural changes. These behavioural problems can be due to causes ranging from true psychiatric ailments or mental retardation to temporary pressor factors such as hormonal changes, academic pressures, childhood neglect, or any sudden emotional event [4, 9].
Clinical manifestation of GI trichobezoars depends upon its size and site [2, 3]. It may remain undiagnosed for years with non-specific signs and symptoms of abdominal pain, vomiting, and early satiety, till it grows to a size to present as a palpable lump in the abdomen with gastric outlet obstruction or its secondary complications such as GI bleeding, gastric erosion, perforation, and peritonitis [2, 3, 5, 6, 9,10,11,12,13, 19]. In addition, intussusception, obstructive jaundice, and pancreatitis have been reported in the literature as complications of unrecognized GI trichobezoar [5, 6, 13,14,15,16]. The rare presentation of trichobezoar is acute abdomen with intestinal obstruction secondary to concurrent or isolated trichobezoar masses in the small intestine [1, 2, 9].
Three cases in our series were of gastric trichobezoars who presented late with a palpable mass in the abdomen with features of gastric outlet obstruction, while one case presented with symptoms and signs of acute abdomen. History of thinning of hairs, trichotillomania, and trichophagia gave us a clue to the diagnosis in such cases.
A plain X-ray abdomen is a nonspecific aid in investigating cases of GI trichobezoars but gives useful information in clinically suspected cases of intestinal obstruction or peritonitis with GI perforation [2]. Diagnosis can be made with a CT scan and upper GI endoscopy [4, 19]. Though upper gastrointestinal endoscopy is considered gold standard [19], a CT scan abdomen, especially contrast-enhanced CT, is the preferred image study for the evaluation of suspected cases of gastric trichobezoar [2, 4]. Although small-bowel bezoars CT findings are nonspecific, it is superior to other radiological modalities for bezoars diagnosis and in suspected cases of small-bowel intestinal obstruction [2]. Diagnostic features of CT images of gastric trichobezoar are the appearance of hypodense and heterogenous mass with mesh-like pattern and mottled air pattern of interspersed air [2, 4]. It is also useful to detect concomitant gastric and small bowel bezoars [2]. In our case series, we did a CT scan abdomen in all cases, and it aided us in the diagnosis-making process and further surgical management.
Management of GI trichobezoar has two main elements; one is its surgical removal with the management of possible complications if any, and secondly, evaluation and management of any underlying psychiatric or social disorder to prevent its recurrence [1, 4, 19,20,21]. The reported recurrence rate in literature is 20% [22] and that underpins the need for periodic psychological assessment in follow-up clinics. Some literature reports an association between trichobezoar and pica [23], which is a compulsive disorder resulting in ingestion of inedible items. This calls for psychiatric evaluation and treatment in the management of trichobezoar cases.
We did laparotomy in all 4 cases, in three cases trichobezoars were removed through anterior gastrostomy while in the fourth case, enterotomy was done for the removal of small bowel trichobezoars. This fourth case was a rare presentation with subacute intestinal obstruction, where only isolated small bowel trichobezoars were found. Paediatric psychiatric consultation was also done in all the cases for assessment and management of the underlying psycho-social problems. Trichobezoar when being removed is potentially infective because of the prolonged time it takes in presentation and entrapment of food particles becoming rancid over time, extreme care was taken to prevent infection in each case. We isolated the part to be opened from the surrounding viscera by abdominal sponges and avoided spillage in the abdominal cavity. Before closing the abdominal wound, it was thoroughly cleaned with povidone and normal saline. We used broad-spectrum antibiotics in all cases. There were no wound infections in our series.
All four patients were later referred to the hospital’s clinical nutritionist for assessment to develop a suitable dietary plan as they were all lean and thin built.
In the literature review, removal of GI trichobezoars by endoscopic techniques or surgical (laparoscopic or open) has been described with varying success rates depending upon available resources, technical expertise, location, consistency, and size of bezoar [4, 24,25,26,27]. Gorter et al. [6], in a retrospective review of 108 cases of trichobezoars, evaluated the success rate of available management options and found that attempted endoscopic removal was not promising and was successful in only 5% of cases, 75% of attempted laparoscopies with different techniques were successful with reported advantages of better cosmesis, reduced hospital stay, whereas reported disadvantages were more spillage in the peritoneal cavity, more operative time, difficulty in assessing concurrent small bowel trichobezoars in cases of intestinal obstruction [4, 6]. Laparotomy was successful in 100% of cases and found the preferred mode of removal of large trichobezoars that allows careful examination of the entire gastrointestinal tract with less complication rate [4, 6, 19, 20, 24]. Other modalities of medical management and enzymatic degradation have been reported as ineffective in cases of trichobezoars [6, 9].
Conclusion
Trichobezoar is a rare entity that should be considered as a differential diagnosis in young female patients with vague, non-specific clinical symptoms and a palpable, upper-abdominal mass.
Small bowel obstruction secondary to trichobezoars, though extremely rare, should raise suspicion that is further supported by presentations of alopecia, a history of trichophagia and trichotillomania, pica, and/or other behavioural disorders.
In our experience and in line with published literature, conventional laparotomy is still the gold standard in cases of GI trichobezoars.
Along with the removal of the trichobezoar, treatment of the existing psycho-social ailment is of utmost importance and needs long-term counselling with periodic psychological evaluation in follow-up clinics to avoid recurrence.
Availability of data and materials
Available upon request.
Abbreviations
- GI:
-
Gastrointestinal
- CT:
-
Computed tomography
- IQ:
-
Intelligence quotient
References
Kwok AMF. Trichobezoar as a cause of pediatric acute small bowel obstruction. Clin Case Rep. 2020;8(1):166–70. https://orchid.org/0000-0002-8742-6236.
García-Ramírez Bertha E, Nuño-Guzmán Carlos M, Zaragoza-Carrillo Ricardo E, Salado-Rentería H, Gómez-Abarca A, Corona JL. Small-bowel obstruction secondary to ileal trichobezoar in a patient with rapunzel syndrome. Case Rep Gastroenterol. 2018;12(3):559–65. https://doi.org/10.1159/000492810.
Mirza MB, Talat N, Saleem M. Gastrointestinal trichobezoar: an experience with 17 cases. J Pediatr Surg. 2020;55(11):2504–9.
Kajal P, Bhutani N, Tyagi N, Arya P. Trichobezoar with and without Rapunzel syndrome in paediatric population: A case series from a tertiary care centre of Northern India. Int J Surg Case Rep. 2017;40:23–6.
Gonuguntla V, Joshi D-D. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res. 2009;7(3):99–102. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2757434/. [Cited 2020 Nov 30].
Gorter RR, Kneepkens CMF, Mattens ECJL, Aronson DC, Heij HA. Management of trichobezoar: case report and literature review. Pediatric Sur Int. 2010;26(5):457–63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2856853/. [Cited 2021 Dec 6].
Sharma RD, Kotwal S, Chintamani, Bhatnagar D. Trichobezoar Obstructing the Terminal Ileum Tropical Doctor. 200232(2):99–100.
Ahmed MM, Tahir KS, Gubari MIM, Rasul RHK, Rashid MJ, Abdul Aziz JM. Large trichobezoar associated with misdiagnosis, a rare case report with a brief literature review. Int J Surg Case Rep. 2021;88:106551.
Swami GA, Binorkar AB, Asawa GR, Halnikar CS. Case presentation on a rare cause of small bowel obstruction- trichobezoar: a case report. Int Surg J. 2021;8(7):2172.
Sharma V, Sharma ID. Intestinal trichobezoar with perforation in a child. J Pediatr Surg. 1992;27(4):518–9.
Nwankwo E, Daniele E, Woller E, Fitzwater J, McGill T, Brooks SE. Trichobezoar presenting as a gastric outlet obstruction: a case report. Int J Surg Case Rep. 2017;34:123–5.
Rattan KN, Yadav V, Yadav V, Singh J. Ileal trichobezoar presenting as intestinal obstruction and peritonitis. APSP J Case Rep. 2017;8(2):11.
Malhotra-Gupta G, Janowski C, Sidlow R. Gastric perforation secondary to a trichobezoar: a case report and review of the literature. J Pediatr Surg Case Rep. 2017;26:11–4.
Laamiri R, Kechiche N, Mnari W, Besbes H, Belhassen S, Mosbahi S, et al. Gastrointestinal trichobezoar causing atypical intussusception in a child: report of two cases. J Pediatr Sci. 2016;8:e214.
Baheti AD, Otjen JP, Phillips GS. A hairy situation: trichobezoar presenting with intussusception, and intestinal and biliary perforation in a child. Radiol Case Rep. 2017;12(1):42–4.
Ibrahim A I. (PDF) Jejunal trichobezoar: a case report. ResearchGate. Annals of Pediatric Surgery; 2016. https://www.researchgate.net/publication/341395680_Jejunal_trichobezoar_a_case_report.
KoushkJalali B, Bingöl A, Reyad A. Laparoscopic management of acute pancreatitis secondary to rapunzel syndrome. Case Rep Surg. 2016;2016:1–4.
Roid GH, Pomplun M. 920120. The Stanford-Binet Intelligence Scales. Fifth Edition, in D. P. Flanagan& P. L. Harrison (Eds). Contemporary intellectual assessment: Theories, tests, and issues (PP. 249–268). The Guilford Press.
Ksia A, Haggui B, Hidouri S, Oumaya M, Mosbahi S, Messaoud M, et al. Management of trichobezoar: about 6 cases. Afr J Paediatr Surg. 2022;19(2):102.
Gaujoux S. Trichobezoar: a rare cause of bowel obstruction. World J Gastrointest Surg. 2011;3(4):54.
Sanneerappa PBJ, Hayes HM, Daly E, Moodley VN. Trichobezoar: a diagnosis which is hard to swallow and harder to digest. Case Rep. 2014;2014(apr30 2):bcr2013201569-9.
Couceiro A, Viveiro C, Capelão G, Nobre J, Laureano M, Gonçalves I, et al. Trichobezoar – a rare cause of abdominal mass and gastric outlet obstruction. GE Port J Gastroenterol. 2016;23(1):50–3.
Mehra A, Avasthi A, Gupta V, Grover S. Trichophagia along with trichobezoar in the absence of trichotillomania. J Neurosciences Rural Pract. 2014;5(01):055–7.
Dong Z-H, Yin F, Du S-L, Mo Z-H. Giant gastroduodenal trichobezoar: a case report. World J Clin Cases. 2019;7(21):3649–54.
Hernández-Peredo-Rezk G, Escárcega-Fujigaki P, Campillo-Ojeda ZV, Sánchez-Martínez ME, Rodríguez-Santibáñez MA, del Ángel-Aguilar A, et al. Trichobezoar can be treated laparoscopically. J Laparoendosc Adv Surg Tech. 2009;19(1):111–3.
Wang Z, Cao F, Liu D, Fang Y, Li F. The diagnosis and treatment of rapunzel syndrome. Acta Radiologica Open. 2016;5(11):205846011562766.
Jain S, Jain P, Prasad A. Role of laparoscopy in gastric trichobezoar: a case report and review of laparoscopic techniques in pediatric and adolescents. World J Laparoscopic Surg DVD. 2021;14(1):58–60.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors were involved in writing and reviewing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Case reports approval is waived from the Institutional Review Board.
Consent for publication
Consent from parents has been taken.
Competing interests
There are no financial or non-financial competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jalil, S., Azhar, M., ElKadi, T.T.H. et al. Paediatric gastrointestinal trichobezoar—an uncommon entity: a case series with recent literature review. Ann Pediatr Surg 19, 27 (2023). https://doi.org/10.1186/s43159-023-00256-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-023-00256-w