Abstract
Background
Spontaneous perforation of the urinary bladder is a rare disease entity. Due to its rarity, it is often hard to diagnose.
Case presentation
We present a case of a 2-year-old patient who presented with bowel obstruction and renal failure after scheduled correctional vertebroplasty due to congenital kyphosis. During exploratory laparotomy, two perforations were found at the dome of the urinary bladder, and an idiopathic spontaneous perforation of the urinary bladder was diagnosed. Primary double repair of the perforations was done, and no primary or secondary cause of the perforation was found.
Conclusion
The constellation of an acute abdomen and abnormal kidney function tests should increase the index of suspicion towards urinary bladder perforation. Due to its rarity, exploratory laparotomy is the gold standard method of diagnosis and treatment.
Similar content being viewed by others
Introduction
A perforated urinary bladder is a rare disease entity that can present differently in a variety of settings and with unexpected etiologies. A perforated bladder can present as in our case, with bowel obstruction, although alcohol intoxication [1], urethral stricture [2], and bladder carcinoma [3] are all reported cases of urinary bladder perforation.
Idiopathic and spontaneous perforation is a very rare entity; we present a case of a 2-year-old female who presented with bowel obstruction after a congenital kyphosis correction surgery, during exploratory laparotomy urinary bladder perforation was diagnosed.
Case presentation
A 2-year-old female with a known case of congenital kyphosis was admitted to the hospital for scheduled correctional vertebroplasty, posterior spinal fusion, and spinal decompression at levels T12–L4. The patient was surgically free and developmentally mature for her age.
As part of the preoperative assessment, an MRI was done, which revealed a horseshoe kidney that her parents did not know of. Her preoperative labs were within a normal range (Table 1). The surgery went uneventfully, and a hip spica cast was applied. On post-operative assessment, the patient had normal neurological exam findings. After 2 days after surgery, she tolerated a regular diet, and the Foley catheter was removed.
Post-operative day 4, the patient’s mother noticed that the patient developed fecal soiling; a digital rectal exam was performed, and deep rectal contractions were palpated; anal sphincter was not assessed as the patient was uncooperative. The next day, the patient vomited twice, two episodes of non-projectile vomiting consisting of partially digested food particles, which were associated with decreased oral intake. It was then followed by another episode of fecal vomiting. During the examination, the cast was found to be tight, putting pressure on her abdomen that protruded from the anterior window of the cast. The cast was split immediately, and we examined the abdomen; during palpation, the abdomen was slightly tense and distended, but no rigidity was noticed. Chest and abdominal X-rays were done, and no findings were seen. We inserted an NG tube and a Foley catheter and kept the patient on IV fluids and NPO; manual aspiration from the NG tube revealed 60 cc of fecal material.
The next day (post-op day 6), the patient was still experiencing episodes of vomiting despite the presence of an NG tube, and her abdomen was mildly distended and tender. She was tachycardic and febrile, and she passed small amounts of watery stool. She was transferred to the PICU for management and observation. Her labs showed evidence of acute kidney injury and dehydration, and her urine culture was positive for Escherichia coli.
Meropenem (adjusted dose for her renal injury) and omeprazole were initiated. Chest and abdominal X-rays were repeated, and proximally dilated and distally collapsed bowels were noted (Fig. 1). The pediatric surgery team was consulted, and an impression of post-operative paralytic ileus was made. She was managed conservatively.
The following day (post-op day 7), an abdomen and pelvis CT scan with contrast was ordered since there was no improvement in her status, and urine retention developed in the past 3 days. The CT scan showed dilated jejunal and mid-ileal loops with a narrow zone of transitions seen at the mid-ileal loops. Moderate free fluid was seen in the abdomen and pelvis. The findings were suggestive of mechanical obstruction, possibly adhesions.
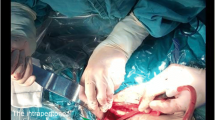
The pediatric surgery team mandated an urgent laparotomy. During the incision, a large amount of serous fluid gushed out the incision. Fibrous bands constricting the mid-ileal segment were released. Formal exploration of the stomach, liver, spleen, small bowels, large bowels, and retroperitoneum showed normal findings. Two perforations at the dome of the urinary bladder were found (Fig. 2); debridement of the necrotic tissue and refreshment of the edges were done first, then a primary double repair of the perforations with PDS 2–0 was done. A suprapubic catheter was inserted while keeping a urethral foley.
The bladder was filled with normal saline to test the repair, and there was no leakage. After irrigation of the abdomen with saline, suctioning, and removal of all the fibrin co-material, another run of the bowel was done. All were healthy-looking.
The patient labs quickly normalized after the surgery; adequate urine output was noted, and she passed stool (Table 1). The NG tube was removed, and the patient tolerated oral intake on a clear fluid diet and then a regular diet with no vomiting. She was kept on IV omeprazole. The patient was discharged from the hospital 5 days after the laparotomy. A cystogram was done after 1 month, before removing the suprapubic catheter, and it showed no leakage of urine.
Discussion
Spontaneous and idiopathic rupture of the bladder is a rare entity which is defined by Sisk and Wear as “If the bladder ruptures without external stimulation, it is spontaneous and deserves to be reported as such.” [4]. There are different cases reported in the literature, and one of the most common causes of perforation in children is pelvic injuries associated with road traffic accidents [5]. Rupture occurs in 20% of children with pelvic fractures [5]. In most of the reviewed literature, lower abdominal pain, which later becomes diffuse with positive peritoneal signs; oliguria or anuria; and renal dysfunction evident biochemically have been the most common symptom of spontaneous bladder perforation.
Although we thoroughly investigated our patient, we found no primary or secondary causes. Multiple cases were reported as idiopathic and spontaneous, Alshareef et al. described a case of a 2.5-year-old patient who presented with ascites and acute kidney injury, who was also managed surgically as in our case; interestingly, when inserting a Foley catheter, it alleviated the symptoms dramatically and corrected biochemical abnormalities [6].
The cause of the rupture may be caused by a structural, congenital abnormality in the bladder wall that may predispose patients to perforations. A 40-year-old female presented with a recurrent episode of bladder dome rupture, due to a non-specific cause and experienced the same symptoms as her previous episode; this mandates a follow-up with the patients to prevent the recurrence of episodes [7].
Moreover, some etiologies can directly cause a perforation; a 70-year-old man had a sudden bladder rupture due to an undetected bladder tumor. He had progressive abdominal distention, vomiting, and biochemical markers that suggested he was suffering from acute renal failure [8]. A biopsy intraoperatively to exclude malignancy as a primary cause would be a reasonable suggestion.
Alcohol intoxication can be a cause. A 45-year-old Sri Lankan man presented with drowsiness, diffuse abdominal pain, vomiting with an odor of alcohol, and urinary retention for 24 h prior to admission. A CT cystogram confirmed the urinary bladder rupture at the dome, which was repaired through exploratory laparotomy [9].
The bladder can rupture due to extreme distention, such as during vaginal delivery; puerperal bladder perforation has also been reported [10].
Conclusion
Finally, every patient presenting with an acute abdomen, signs and symptoms of peritonitis, oliguria, and renal failure should have urinary bladder perforation considered in their differential diagnosis. Because of its rarity, preoperative diagnosis of the perforation is challenging. Whatever the cause, a perforated urinary bladder can manifest in a variety of ways in different circumstances. The diagnosis requires a high index of suspicion and must be on the differential diagnosis list when there is a similar clinical picture.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during this study.
References
Parker H, Hoonpongsimanont W, Vaca F, Lotfipour S. Spontaneous bladder rupture in association with alcoholic binge: a case report and review of the literature. J Emerg Med. 2009;37(4):386–9. https://doi.org/10.1016/j.jemermed.2007.03.049.
Palthe S, Dijkstra GA, Steffens MG. A case of spontaneous urinary bladder rupture secondary to urinary retention due to urethral stricture. Urology Case Rep. 2018;17:85–7. https://doi.org/10.1016/j.eucr.2018.01.009.
Ahmed J, Mallick IH, Ahmad SM. Rupture of urinary bladder: a case report and review of literature. Cases J. 2009;2(1). https://doi.org/10.1186/1757-1626-2-7004.
Sisk IR, Wear JB. Spontaneous rupture of the urinary bladder. J Urol. 1929;21(4):517–22. https://doi.org/10.1016/S0002-9610(36)90638-4.
Bakal U, Sarac M, Tartar T, Ersoz F, Kazez A. Bladder perforations in children. Niger J Clin Pract. 2015;18(4):483. https://doi.org/10.4103/1119-3077.151752.
Alshareef TA, Almaiman W, Figueroa VH, Gooden MA, Bägli DJ, Harvey E. Idiopathic urinary bladder perforation in early childhood. Kidney Int Rep. 2018;3(6):1497–500. https://doi.org/10.1016/j.ekir.2018.07.022.
Bartholomew R, Ahmeti M. A case of idiopathic recurrent spontaneous bladder rupture. Case Rep Surg. 2021;30(2021):1–4. https://doi.org/10.1155/2021/6615817.
Chakraborty A, Mandal K, Bhunia A, Hasnat S, Dutta S. Spontaneous intraperitoneal bladder rupture: a rare case report. J Clin Diagn Res. 2019. https://doi.org/10.7860/jcdr/2019/39616.12581.
Muneer M, Abdelrahman H, El-Menyar A, Zarour A, Awad A, Al-Thani H. Spontaneous atraumatic urinary bladder rupture secondary to alcohol intoxication: a case report and review of literature. American J Case Reports. 2015;16:778–81. https://doi.org/10.12659/ajcr.894992.
Sailo SL, Sailo L. Spontaneous puerperal bladder perforation presenting with urinary retention. Urology J. 2014;11(4):1854–54. https://doi.org/10.22037/uj.v11i4.2534.
Acknowledgements
None.
Funding
This study received no funding from any funding agency in the public, commercial, and not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NAO and AA made the diagnosis. SA-H, DAH, and MAB wrote the manuscript. All authors revised the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent was taken.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AlAbadla, A., AlOmari, N., Al-Halaseh, S. et al. Spontaneous urinary bladder perforation presenting as bowel obstruction in a child: a case report. Ann Pediatr Surg 19, 17 (2023). https://doi.org/10.1186/s43159-023-00250-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-023-00250-2