Abstract
Background
The fetu in fetu (FIF) is an extremely rare congenital condition characterized by a 2nd fetus that grows into the body of the healthy twin. Its thoracic location is more exceptional.
Case presentation
We report a case of intrathoracic mass in a 5-month-old female infant, diagnosed after an assessment for respiratory distress. She underwent an emergency left thoracotomy which allowed for the removal of a large thoraco-mediastinal mass inside a membranous sac containing a clear liquid mixed with vernix caseosa. The mass was completely covered with normal skin, three lobes similar to rudimentary outline of the head and limb. It was attached to a single large vascular pedicle. The pathological examination concluded that there was a high possibility of FIF. The postoperative follow-up was uncomplicated, and the child is still in good clinical condition after the 5-month follow-up.
Conclusion
The assessment of the respiratory distress in an infant with a mass centered by an axial skeleton on the chest x-ray and thoracic CT scan may suggest a diagnosis of intrathoracic FIF.
Similar content being viewed by others
Background
The frequency of thoracic masses in children is difficult to establish due to the publication bias. However, more than half of the cases are intrathoracic masses (62%), with mediastinal mass being the most common case [1]. The “fetus in fetu” (FIF) is an extremely rare congenital pathology characterized by the parasitic development of a malformed fetus within the body of the normal second twin [2]. FIF most often develops in the abdominal cavity; although not unheard of, the thoracic location is exceptional [3]. The main differential diagnosis of intrathoracic FIF is a mediastinal teratoma that is very rare in children and accounts for 8% of the extragonadal teratoma and 2% of mediastinal tumors in children [4]. We report a case of intrathoracic mass in a 5-month-old female infant that suggests a diagnosis of an FIF.
Case presentation
Patient information
A 5-month-old female infant weighing 5 kg was referred from a private clinic for presenting with respiratory distress progressing for 72 h. The anamnesis recorded a history of recurrent pulmonary infections progressing from the age of 2 months. The gestational history recorded a normal pregnancy without abnormality or fetopathy on antenatal ultrasound. By the 39th week of amenorrhea, delivery was performed by cesarean section for fetal distress. Her birth weight was 2600 g; the Apgar score was 9.
Clinical findings
On admission, she was presented with moderate respiratory distress: respiratory rate = 50 cycles per minute, SpO2 = 94%, discreet intercostal indrawing, and nasal flaring, the pulse at 137 beats per minute, dullness in percussion, and decreased breath sound on auscultation of the left pulmonary field.
Diagnostic assessment
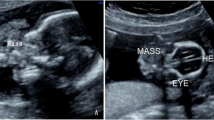
Series of chest x-rays showed persistent opacity of the left hemithorax with axial opacity of skeletal-looking bone density with a rightward deviation of the mediastinum (Fig. 1). Chest ultrasound suggested a large collection (21.1 mm) of liquid with an echogenic appearance in the thoracic cavity with passive atelectasis of the left pulmonary parenchyma. The biological assessment reveled anemia (10.3 g/dl), hyperleukocytosis (25G/L) with polynucleosis, thrombocytosis at 524 G/L, and a slight relative increase in tumor markers: alpha-fetoprotein (AFP) = 73.26 ng/ml, beta-human chorionic gonadotropin (BhCG) = 9.11 mIU/ml, and carcinoembryonic antigens (CEA) = 4.92 ng/ml. During the 72 h wait to perform the thoracic computed tomography (CT) scan, the patient presented a sudden clinical and radiological worsening of the respiratory distress forcing the realization of an emergency left thoracic drainage of 250 ml of a clear liquid mixed with a whitish substance similar to vernix caseosa. Cytological analysis of the chest fluid was conducted without findings of any abnormal cells or germs. We noted an obvious clinical and radiological regression of respiratory distress after thoracic drainage, allowing thoracic CT scan to be performed under better conditions, revealing a heterogeneous mass spanning the entire left hemithorax to the anterior and middle mediastinum, deviation of mediastinal organs toward the right hemithorax, compression of the left lung, and hypertrophy of the left lower lobe; this mass is centered by an opacity of bone density (Fig. 2).
Chest CT scan and 3D reconstruction series. A, B Heterogeneous mass spanning the entire left hemithorax to the anterior and middle mediastinum, deviation of mediastinal organs toward the right hemithorax, compression of the left lung, and hypertrophy of the left lower lobe; mass centered by an opacity of bone density. C, D Reconstruction showing the residual left lung, the axial skeleton of the mass
The radiologists had suggested as hypothesis FIF or a diaphragmatic hernia with a perforation of the bowel by the chest drain or thoracic mass.
Therapeutic intervention
A left posterolateral thoracotomy (5th intercostal space) was performed urgently under general anesthesia with orotracheal intubation. We found a mass occupying the entire left hemithorax and mediastinum, compression of the heart and lungs, and pushing back the heart to the right (Fig. 3A). It was covered with a membranous sac containing a little clear liquid mixed with vernix caseosa. This mass had a normal hairy skin and vernix caseosa scattered over its entire surface; at its lower pole, there are three lobes resembling a rudimentary outline of head and limbs and of an organ on its internal face (Fig. 3A, B). It was attached to a single large vascular pedicle similar to an umbilical cord (Fig. 3A, B). A complete resection of the mass was performed after ligation section of the pedicle; this pedicle contained two vessels. The mass weighed 170 g with the following measurements 11 × 8 × 8 cm (Fig. 3C). Complementary and complete resection of a small sessile mass 1.5 cm in diameter was performed. We noted pulmonary re-expansion and decompression of the heart intraoperatively.
Follow-up and outcomes
The anatomopathological analysis found on the fragment studied a normal skin covering, normal adipose tissue, normal muscle tissue, and normal vascular tissue, all centered by a mature bone of normal structure, the absence of immature tissue or undifferentiated focus, and the absence of any sign of malignancy. Histopathology examination concluded that there was a high probability of a second digested twin. Analysis for genetic markers in the mass had failed after several attempts because the surgical specimen had been immersed in formalin. The postoperative care was uncomplicated; the patient was discharged on the 10th day. The left pulmonary re-expansion was incomplete on postoperative chest radiographs; this deficit was corrected by respiratory physiotherapy sessions. At a 5-month follow-up, the child was in good clinical condition with satisfactory radiological imaging with no signs of recurrence; the AFP was normal at 13.12 ng/ml.
Discussion
The term FIF was first described in 1800 by the German Anatomist Johann Friedrich Meckel, the first case report had been published by Young in 1809, and the first approach of definition by Willis in 1953 [2, 5].
FIF results from the abnormal embryogenesis of a diamniotic monochorionic twin pregnancy leading to asymmetric division and abnormal anastomosis of the yolk circulation [5]. It is a rare pathology, with a prevalence of 1/500,000 births; less than 200 cases have been reported worldwide [6]. FIF occurs in different age groups with a predominance in early childhood and in the majority of cases diagnosed in patients younger than 18 months with a presumed male prevalence [6, 7]. The clinical symptoms of FIF are related to the compression of neighboring organs by the mass (abdominal distension, feeding difficulties, vomiting, respiratory distress), but it can be asymptomatic [3, 5, 6]. Our patient presented with respiratory distress preceded by recurrent lung infections. She improved markedly after thoracic drainage and mass exeresis. The preoperative diagnosis of FIF is made in 16.7% of cases [3, 5]. In our case, the diagnosis of FIF was made intraoperatively. The chest x-ray points to the diagnosis, when it shows the axial skeleton, while computed tomography and MRI confirm the diagnosis, relations, and the mass effect [2, 5]. All these radiological specificities had been found in our case.
FIF can be the subject of prenatal diagnosis; however, a limited number of cases (7%) of FIF were diagnosed before birth [6]. In our case, the diagnosis was made after the birth intraoperatively. In most cases, the localization is abdominal; however, it can be detected in the brain, mouth, skull, neck, mediastinum, liver, scrotum, and even the sacrococcygeal region. The thoracic localization of FIF is extremely rare. Only 6 cases have been reported; in three patients, the mass was in the mediastinum, one in the lung parenchyma, one in the left hemithorax, and one in the anterior chest wall [3, 6]. In our case, the FIF straddled the left hemithorax and mediastinum.
Macroscopically, the FIF appears as a mass suspended by a vascular pedicle, within a sac containing liquid, or vernix caseosa. A vascular anastomosis with the host’s vessels is identifiable. FIF is generally anencephalic and acardiac. It has a varying degree of organogenesis with an axial skeleton and rudimentary limbs. The size of the FIF is related to the blood supply, and the weight varies between 13 and 2000 g. Most often, it is unique, but the presence of 2 or 3 FIFs, or even more, has been observed; Kimmel found more than 5 FIF intracerebral [5, 8]. Spencer recommends that a FIF should meet one or more of the following criteria: (a) be enclosed in a separate bag containing liquid or vernix caseosa, (b) be partially or completely covered with normal skin, (c) have roughly recognizable anatomical parts, and (d) be attached to the host by one or a few relatively large blood vessels [8]. Our clinical case met most of these criteria. AFP, BhCG, and CEA may be normal or elevated [5, 9]. In our case, AFP and BhCG were elevated, and CEA was normal.
The main differential diagnosis of FIF is teratoma due to the risk of malignancy associated with the latter. FIF is almost always benign with only one reported case of malignancy. The presence of a spine is a differentiator between a FIF and a teratoma. However, radiologists and pathologists have concluded that FIF can be retained even in the absence of a vertebral axis. Although fewer than 200 cases of FIF have been reported, the presence of a well-formed spine has only been documented in a limited number of cases. In about 9% of FIF cases, no spine was found [2, 3, 5, 10]. Gonzalez-Crussi suggested that the term FIF be applied to any structure in which the fetal form has highly developed organogenesis or the presence of a vertebral axis [8, 9].
There is a theory of FIF as being “a highly differentiated mature teratoma” and the theory of “parasitic twins” [2, 5, 6].
Analysis of genetic markers, such as blood group, karyotype, and DNA, shows no genetic difference between host and FIF. Therefore, this result is compatible both with the theory of “parasitic twins” and the “monozygous teratoma” theory [6, 8]. The final diagnosis of FIF is not made until the pathological analysis. The recommended surgical treatment is complete surgical excision. The design of the type of surgical approach is an important preoperative consideration. Close postoperative follow-up by ultrasound and serology (AFP or beta-HCG level) is recommended to exclude even rare cases of recurrence [6, 9].
Conclusions
The assessment of respiratory distress in infants with a mass centered by an axial skeleton on the chest x-ray and thoracic CT scan may suggest a diagnosis of intrathoracic FIF. Intrathoracic FIF must meet most of Spencer’s criteria. Clinical and paraclinical monitoring is required to exclude even rare cases of recurrence.
Availability of data and materials
Not applicable.
Abbreviations
- FIF:
-
Fetus in fetu
- AFP:
-
Alpha-fetoprotein
- BhCG:
-
Beta-human chorionic gonadotropin
- CEA:
-
Carcinoembryonic antigens
References
Orman G, Masand P, Hicks J, et al. Pediatric thoracic mass lesions: beyond the common. Eur J Radiol Open. 2020;7:100240. https://doi.org/10.1016/j.ejro.2020.100240.
Sitharama SA, Jindal B, Vuriti MK, et al. Fetus in fetu: case report and brief review of literature on embryologic origin, clinical presentation, imaging and differential diagnosis. Pol J Radiol. 2017;82:46–9. https://doi.org/10.12659/PJR.899956.
Reddy RK, Kannaiyan L, Srirampur S, et al. Thoracic fetus in fetu. J Indian Assoc Pediatr Surg. 2012;17(4):178–9. https://doi.org/10.4103/0971-9261.102344.
Liew WX, Lam HY, Narasimman S, et al. Mediastinal mature teratoma in a child- a case report. Med J Malaysia. 2016;71(1):32–4.
Kahloul N, Adouani M, Khattat N, et al. Fœtus in fœtu: à propos d’un cas. Archives de pédiatrie. 2010;17(3):249–52. https://doi.org/10.1016/j.arcped.2009.10.028.
Ruffo G, Di Meglio L, Di Meglio L, et al. Fetus-in-fetu: two case reports. J Matern Fetal Neonatal Med. 2019;32(17):2812–9. https://doi.org/10.1080/14767058.2018.1449207.
Liu J, Tian B, Zeng Q, et al. Mediastinal teratoma presenting with hemoptysis and pleuritis misdiagnosed as tuberculosis (empyema). BMC Pediatr. 2018;18(1):382. https://doi.org/10.1186/s12887-018-1357-7.
Khope S, Phaldesai N, Borkar J, et al. Fetus in fetu in the scrotal sac of newborn. Annals of Pediatric Surgery. 2016;12:68–70. https://doi.org/10.1097/01.XPS.0000481340.83228.54.
Ji Y, Chen S, Zhong L, et al. Fetus in fetu: two case reports and literature review. BMC Pediatr. 2014;14:88. https://doi.org/10.1186/1471-2431-14-88.
Sharma A, Goyal A, Sharma S. Fetus in fetu: a rare case report. J Res Med Sci. 2012;17(5):491–4.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AKBB and GMAB managed the child. AKBB operated the child. AKBB wrote down the case; JA managed the procedure of anesthesiology, ASG assisted and supervised in operating upon the child; ASG, JMA, and AMF supervised and did the critical revision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication was obtained from patient’s mother as the patient was less than 16 years old.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bata, AK.B., Akodjènou, J., Bognon, G.M.A. et al. Intrathoracic mass in a 5-month-old infant: fetus in fetu—a case report. Ann Pediatr Surg 18, 30 (2022). https://doi.org/10.1186/s43159-022-00167-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-022-00167-2