Abstract
Background
The current research aims to determine the pharmacokinetic parameters, mucoadhesive strength, and IVIVC correlation of the novel chronotherapeutic drug delivery system of montelukast sodium (MTS) loaded Parteck® SRP80 and hypromellose system. To accomplish this, an HPLC method was developed which is highly sensitive, precise, and rapid for quantifying pure MTS in rabbit plasma. Mucoadhesive strength and time-dependent mobility of developed formulation were established by ex-vivo study and X-ray radiography, respectively. Using a fraction of drug absorbed (FDA) and a fraction of drug released (FDR), Level-A in-vitro in-vivo correlation (IVIVC) was developed. According to ICH Q1A (R2) standards, stability experiments were conducted for 180 days.
Result
MTS retention time came as 3.971 min with a mobile phase of methanol: acetonitrile: 0.2 mM sodium acetate buffer (5:90:5). In-vitro dissolution showed pulsatile release of the drug up to 24 h with two lag phases. The in-vivo study showed a Cmax of 490.16 ± 33.95 ng/ml, Tmax of 9 h, and MRT of 14.08 ± 1.21 h. The correlation coefficient of 0.9899 confirmed the level-A IVIVC. Uncoated matrix tablet of Parteck® SRP 80 displayed mucoadhesive strength 1.25-fold higher than hypromellose. Stability experiments found no significant changes in drug content, physical appearance, and cumulative percentage release with a similarity factor of 87–90.
Conclusion
A single oral dose in-vivo study proved the sustained release of the drug for 24 h with satisfactory mucoadhesive strength. Moreover, X-ray radiography has confirmed the time-dependent presence of formulation at the needed spot. This study fulfilled all the requirements for chronotherapy of asthma and can be scaled up in the future.
Graphical abstract

Similar content being viewed by others
Background
Montelukast sodium (MTS) is an LTD4 receptor antagonist used to treat asthma and allergic rhinitis and prevent exercise-induced bronchoconstriction [1]. Chemically, it is C35H35ClNNaO3S with the IUPAC name sodium; 2-[1-[[(1R)-1-[3-[(E-2-(7-chloroquinolin-2-yl)ethenyl]phenyl]-3-[2-(2-hydroxypropan-2-yl)phenyl]propyl]sulfanylmethyl]cyclopropyl]acetate [2, 3]. With more effectiveness in the night-time administration of MTS, it is also beneficial to relieve the early morning symptoms of nocturnal bronchial asthma (NBA) [1, 4,5,6]. Chronotherapeutics deals with the delivery of drugs as per the variations of the intensity of the symptoms. Asthma is considered an early morning pathology where symptoms vary in the early morning and the entire day or night. Design and development of a time-dependent dosage form are the need of the hour [7,8,9,10].
Accordingly, the Once-a-day Chronotherapeutic drug delivery system (ChrDDS) was created in our previous research with Hypromellose (HPMC) and Parteck® SRP80 [11]. Two matrix tablets batches (T1 & T2) were punched one with HPMC K100/K15 M (T1) and another with Parteck® SRP 80 (T2). The drug and excipients showed excellent compatibility when assessed by using FTIR, DSC, and XRD [11]. From the in-vitro dissolution, data of individual batches of uncoated tablets T1F1 & T2F3 further proceeded for compression coating. The developed formulation was designed in such a way as to release the drug in two phases, one in the early morning for a duration of 3–4 h then a sustained release of the drug for 10–11 h. To initiate release in the early morning, a lag period of 4 h was framed by coating the first part of ChrDDS (T1F1) with HPMC K4M. For the second pause phase, a lag time of 10 h was provided with a coating of a 2:1 mixture of Carbopol 934P and ethyl cellulose. To protect DDS (drug delivery system) from gastrointestinal pH, both optimum-coated component was put in an Eudracap™ ready-to-fill enteric-coated capsule [11]. From in-vitro studies of individual parts, hypothesis has been made that 40% of the drug is released in the early morning and the remaining 60% till the end of 24 h [11]. This hypothesis has been tested by an in-vivo study in the current research work.
In this paper, an in-vitro dissolution study of previously developed ChrDDS was performed in different dissolution media with different pH to assess drug release. To establish in-vitro in-vivo correlation (IVIVC), an in-vivo pharmacokinetic study was conducted on white New Zealand rabbits and compared for both marketed (Montek 10 by Sun Pharma) and optimized ChrDDS. To accomplish this, a unique, sensitive, and precise HPLC method was developed which is an integral part of the characterization of a drug molecule to check its purity [12]. To release the drug in the gastrointestinal tract (GIT), the formulation needs to be stuck with the intestinal wall for a longer period so mucoadhesive strength and mucoadhesive time must be determined by the ex-vivo study [13]. The movement of the dosage form in the GIT is to be mapped by X-ray radiography by replacing the equivalent amount of the drug with barium sulfate [14]. This paper also includes the assessment of the stability of the developed dosage form as per ICH guidelines [15, 16].
Methods
Materials
Tropac rabbit dose dispenser of size 5 was purchased from Custom Capsules Pvt. Ltd. in Maharashtra (India). The gelatin capsule (size 5) was provided by Patco Pharmaceuticals Pvt Ltd., Mumbai (India). MTS was a generous gift from Torrent Pharmaceuticals Ltd., Gujrat (India). Sodium acetate was purchased from Sigma-Aldrich Pvt. Ltd. in Mumbai (India). Methanol and acetonitrile of HPLC quality were purchased from SD Fine-Chem Ltd., Mumbai (India). Wherever necessary, HPLC-grade water was used.
UHPLC (Agilent 1260, USA) equipped with an autosampler, quaternary pump, and PDA detector with ChemStation software was used for chromatographic analysis. Poroshell 120EC-C18 column (4.6 × 50 mm × 5.0 μm) was employed as the stationary phase.
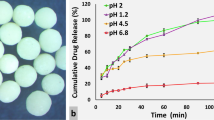
In-vitro dissolution study
The drug release characteristics of both the marketed formulation (Montek 10) and MTS ChrDDS were determined on a USP type II dissolution apparatus (Electrolab, TDT08L, India) at 37 ± 0.5 °C and 75 rpm. The study was performed with 0.1N HCl solution (pH 1.2) for 2 h, after that with acetate buffer (pH 4.5) for 1 h, then with pH 6.8 SLS solution (0.5% w/v) for the remaining time as dissolution medium. Samples were taken at predetermined time intervals, filtered with a 0.45-mm membrane filter, and subjected at 345 nm to a UV spectrophotometer for further analysis.
HPLC analysis
The stock solution of MTS was prepared by dissolving 100 mg of the drug in 100 ml methanol solution. 1 ml of prepared solution was taken and diluted up to 10 ml (100 μg/ml) to make a working solution. From the stock solution (1 mg/ml), series of dilutions were prepared in a range of 10–600 μg/ml to create a calibration curve. It will be used for validation of the developed bioanalytical method. The quantitative determination of the drug was performed with the mobile phase of a mixture of methanol: acetonitrile: 0.2 mM sodium acetate buffer (5:90:5) with a 0.5 ml/min flow rate. Analysis was performed at a wavelength of 285 nm [17]. To filter mobile phase glass vacuum-filtration microfilter (0.22 mm) and to remove entrapped air, degassing ultrasonic bath was used. The calibration curve in rabbit plasma was prepared by spiking 20 µl of MTS working solution (10, 20, 50, 100, 200, 500, 1000, 1500, and 2000 ng/ml) in the HPLC column. From the literature review, Zafirlukast was cast off as an internal standard with 5000 ng/ml plasma concentration [18]. It has an appropriate retention time and a good resolution from MTS under chromatographic conditions. No interference peaks were observed in the regions where the drug was eluted. Three quality control samples were prepared at 25, 250, and 1250 ng/ml by spiking the drug and internal standard into rabbit plasma. Before that drug-free plasma was tested to check any interferences in the peak of the drug and internal standard. The established method was verified for selectivity, specificity, accuracy, precision, robustness, and ruggedness.
In-vivo study
Pharmacokinetic studies were performed on two groups of white New Zealand rabbits (n = 4). Rabbits fasted overnight with only a water supply. The developed dosage form was administered orally in a size 5 capsule by using a Torpac animal dose dispenser [19,20,21]. Ears were shaved before taking out blood samples. From the marginal ear vein, 100 µl of blood samples were collected in Eppendorf tubes at times 0, 2, 4, 6, 8, 10, 12, 18, and 24 h after administration. Due to the high log p (8.49) value of MTS, 10 µl of the internal standard was injected into the sample before being retrieved with 1.5 ml tertiary butyl methyl ether [22]. The prepared mixture was vortexed for 15 min then centrifuged for 10 min at 10,000 rpm. After centrifugation, the organic supernatant was put into a glass tube and evaporated for 5 min at 50 °C under a stream of Nitrogen Evaporator (Caliper Life Sciences, Hopkinton, MA, USA). The remaining residue after complete drying was reconstituted with mobile phase (150 μl) with vertexing for 1 min. The prepared drug sample was stored at − 70 °C till analysis.
In-vitro in-vivo correlation
By plotting a graph, Level A IVIVC was developed for optimized formulation. The graph was plotted between the fraction of drug release (FDR) from the in-vitro dissolution study and the fraction of drug absorbed (FDA) from the in-vivo dissolution study [23]. From the deconvolution approach of the Wagner–Nelson method, fraction of the absorbed drug was determined from AUC. It was calculated from the Plasma concentration profile by using concentration at time t (Ct), elimination rate constant (Ke), and area under the plasma concentration curve (AUC0−t & AUC0−∞).
Statistical analysis
All the statistical analyses were performed by GraphPad Prism v 9.4.1 to assess the p values (statistical significance) between the groups.
Ex-vivo study
To determine the mucoadhesive strength and time, ex-vivo studies were performed.
Mucoadhesive strength
It was measured in grams which are required for the complete detachment of the tablet from the intestinal mucosa [24]. From a local slaughterhouse, the fatty acid-free freshly cut porcine intestine membrane was obtained and stored for 30 min in Krebb’s buffer solution at pH 6.8 and temperature 37 ± 0.5 °C. The experiment was conducted on a modified physical double beam balance where the right pan was replaced by a glass slide. The left pan was carrying weight to measure the mucoadhesive strength. A 2 × 2 × 2 cm wooden cubicle block tied with intestinal membrane was dipped in Krebb’s buffer solution till the upper layer of mucosa was. The tablet was adhered to the glass slide with cyanoacrylate glue and allowed to maintain contact with the membrane under a constant weight of 5 g. Mucoadhesive strength was determined for both T1F1 and T2F3 with n = 3 by estimating the force necessary to break the contact between the tablet surface and intestinal mucosa [25, 26].
Mucoadhesion time
This study was conducted for both coated and uncoated tablets of T1F1 and T2F3 similar to mucoadhesive strength [26]. The tablet was stuck on the wet intestinal membrane tied over the glass slide, and a stirring of 50 rpm was applied to simulate peristaltic movement. Time taken by a tablet to separate from mucosa was noted in triplicate and averaged as mucoadhesion time [27].
X-ray radiography
X-ray radiography was adopted to track the ChrDDS's time-dependent mobility after receiving approval from the College IEAC (Institutional Animal Ethics Committee). MTS (Montelukast sodium) of T1F1 and T2F3 of formulated ChrDDS was replaced by BaSO4 to take X-ray radiographs [14, 28]. Two white New Zealand rabbits fasted overnight and a size 5 capsule containing individual parts of ChrDDS was administered through a Tropac oral dispenser followed by 10–15 ml of water [14]. For the entire duration of the study, rabbits had free access to water only. To take X-ray radiographs, rabbits were anesthetized with ketamine hydrochloride (20 mg/kg dose) and exposed to the lateral and ventral abdominal region. Images were taken at 0 h (before administration), 2 h, and 6 h for T1F1 and 0 h (before administration), 2 h, 6 h, and 9 h for T2F3 by X-ray generator (Orvee medical solutions) at 100 mA, 100 KVP, 230 V, 50 Hz in a single phase [29]. The position of tablets was observed and noted.
Stability studies
Developed ChrDDS was kept for 6 months in a stability chamber (HICON® 216 Grover Enterprises, New Delhi, India) to conduct accelerated stability studies following ICH guideline Q1A (R2) at 40 ± 2 °C temperature and 75% relative humidity [16, 30]. Samples were evaluated at 0, 90, and 180 days for cumulative percentage release, drug content, and disintegration time. All data were investigated for similarity factors regarding the zero-minute release profile. Capsules were also monitored for physical appearance. Optimized formulations' in-vitro drug release was statistically analyzed using GraphPad Prism's 9.4.1 one-way ANOVA.
Results
In-vitro dissolution study
90% of the medication was released immediately by Montek 10 in 2 h [11], while developed ChrDDS releases 99.98 ± 0.02% of the drug in 24 h (Fig. 1). Due to enteric coating, there is no release till pH 6.8. Then, there is a lag time of 4 h due to the compression coating of HPMC K4M. Drug release starts after 7 h of administration and releases for 4 h approximately. The second pause phase of release remains for 3 h (starts from the 11th h of administration and continues up to the 14th h). Till that time, 40% of the total dose (10 mg) has been released in the dissolution medium. There was a sustained and regulated release of the drug up to 24 h after administration following the second lag time.
HPLC analysis
From the calibration plot of peak area vs drug concentration (mcg/ml), the regression coefficient came as 0.9995 conforming to its linearity. Chromatograms were obtained by incorporating 300 μg/ml of MTS and 200 μg/ml of internal standard in the rabbit plasma. It showed a retention time of 3.971 min for MTS and 6.613 min for internal standard as displayed in Fig. 2b (Table 1). The peak area ratio vs drug concentration (ng/ml) in rabbit plasma plot has given the correlation coefficient as 0.9989 with regression equation which has been further used to determine sample concentration as displayed in Fig. 2a. The accuracy of the calibration curve is summarized in Table 2 with LOD and LOQ values identified as 15.1 and 49.8 ng/ml, respectively.
Drug solution concentrations were estimated for intra-day and inter-day fluctuation at 25, 250, and 1250 ng/ml for the precision and accuracy of the established bioanalytical approach (Table 3).
In-vivo studies
To ascertain the drug's pharmacokinetic properties, the developed bioanalytical approach was applied. The concentration of samples was calculated from the regression equation. The marketed formulation showed immediate release of the drug with higher Cmax and less Tmax value than ChrDDS (Table 4). The Phoenix WinNonlin 8.3 software (trial version Certara University, Princeton, NJ, USA) was used to calculate the pharmacokinetic parameters [31]. Figure 3 displayed the in-vivo profile of the marketed formulation and developed DDS.
In-vitro in-vivo correlation
FDR was determined from the dissolution test and FDA from Eq. 1. Utilizing GraphPad Prism 9.4.1 a simple linear regression analysis was carried out (Fig. 4). From graph R2 value came as 0.9899 with a slope of 0.964 establishing a point-to-point correlation [32, 33].
Statistical analysis
From drug release data of Montek 10 and MTS statistical analysis was achieved by GraphPad Prism 9.4.1. Non-parametric Mann–Whitney test was used and the p value < 0.05 indicates both are significantly different. Mann–Whitney coefficient U was 41 with the actual difference between them as − 195 and Hodges–Lehmann difference as − 107.5.
Ex-vivo study
Mucoadhesive strength was determined for uncoated and coated optimized tablets. For hypromellose uncoated and coated tablets, it came as 54.83 ± 0.82 mg and 61.17 ± 0.91 mg, respectively. With Parteck® SRP 80 for an uncoated and coated tablet, it came as 68.93 ± 0.71 and 78.14 ± 1.08 mg, respectively. The obtained value confirmed sufficient adhesion of matrix tablets on the mucosal wall which was further proved by the mucoadhesion time [34].
Mucoadhesion time To enhance and prolong the retention time of the tablet in GIT, it should adhere to the site of absorption and the mucoadhesion process does this by making a rigid and intimate contact between the intestinal layer and tablet surface [35]. Mucoadhesion time is determined for both coated and uncoated tablets. The uncoated matrix tablet of T1F1 is attached for 5.5 h and T2F3 for 11 h, while the coated tablet of T1F1 adheres for 2.5 h and 12 h for T2F3. Results from uncoated tablets are in simulation with in-vitro drug release data and coated tablets conform to the lag time duration.
X-ray radiography
From the radiographs of BaSO4-loaded T1F1 and T2F3, mobility of the developed formulation was monitored. T1F1 was present in the stomach for up to 6 h, and T2F3 was adhered in the intestine wall for up to 9 h (Fig. 5).
Stability studies
These studies assessed any alterations in the samples' physical characteristics, drug content, drug release, and disintegration speed for 180 days. No significant changes are observed in all parameters after a specified time. From Table 5, it has been confirmed that the developed chronosystem is stable and suitable for long-term storage conditions [36]. Statistical analysis of in-vitro drug release for optimized formulation for 0, 3rd, and 6th month given p value of 0.9987 from Brown-Forsythe test and > 0.9999 from Bartlett's test showed no significant difference. The p value of 0.9998 from the ANOVA summary also confirmed the stability of the developed chronosystem.
Discussions
From the literature, it has been found that once daily evening dose of montelukast improves NBA (Nocturnal Bronchial asthma). To date, no chronotherapeutic formulation has been marketed with montelukast [4, 10]. In the previous research work, an in-vitro dissolution study was performed for the individual uncoated tablet (T1 and T2) to assess the drug release. For coated tablets, it was executed to finalize the lag time duration of optimized tablets (T1F1 and T2F3) [11]. Once a ChrDDS was developed in-vitro dissolution study has been performed in the current research work in the different dissolution media for a specified time duration. From in-vitro dissolution data, it was found that the drug was released in a pulsatile manner with two lag phases followed by sustained release of the drug. The obtained drug release data is used in establishing IVIVC.
From different combinations of mobile phases and system parameters like flow rate, injection volume, and temperature best separation condition was achieved as mentioned in the methodology. The developed method was thoroughly validated as per FDA [12] and ICH guidelines [37]. The suggested method's suitability parameters, such as retention time, peak area, height, tailing factor, resolution, and theoretical plate number are summarized in Table 1 to confirm the method’s appropriateness for resolution and repeatability. Six consecutive injections with a relative standard deviation RSD of less than 2% demonstrated excellent injection repeatability and precision. Between MTS and Zafirlukast, the tailing factor was close to one and the resolution was 1.671, indicating good peak separation and symmetry. High theoretical plate numbers served as evidence of superior column efficiency. Over the concentration range of 10–2000 ng/ml of MTS, an exceptional correlation between the peak area ratios of the drug and the internal standard was seen. The excellent linearity and accuracy of the calibration graph between the peak area ratio and the rabbit plasma drug concentration were confirmed by a correlation coefficient (R2) value of 0.9989 and regression equation y = 0.0016x + 0.1211(Table 2). From this equation, concentration of samples was calculated to determine pharmacokinetic parameters. For three distinct concentrations, the established method's precision and accuracy were evaluated. The results are summarised in Table 3, which reveals that the RSD for all concentrations was under 2%. It verified that the results for precision and accuracy were robust, reproducible, and within the permitted range under the validation requirements [38].
Utilizing internal standard, drug, and blank rabbit plasma, the HPLC-developed technique's selectivity was evaluated. Retention times obtained were comparable to real samples with no interfering peaks. As MTS belongs to a BCS class II drug with a log P value of 8.49 [22, 39], extraction of the drug from plasma needs to be done by a non-polar solvent. Among all tried non-polar solvents tetra-butyl-methyl-ether showed good recovery and zero interference with both drug and internal standard [22]. Using Phoenix WinNonlin 8.3 software, the non-compartmental pharmacokinetic parameters were estimated. By examining the plasma concentration and time plot, the maximum concentration (Cmax) and the time to attain it (Tmax) were calculated. The software was used to calculate the clearance, volume of distribution (Vd), mean residence time (MRT), and elimination half-life (t1/2) (Table 3). In comparison with the marketed product, the created ChrDDS demonstrated an extended stay in blood circulation which had been confirmed by a larger area under the curve in the drug plasma concentration vs. time profile (Fig. 3). The marketed tablet showed immediate release of the drug with a higher value of Cmax (648.29 ± 121.63 ng/ml) in a short span of 2 h as Tmax which may cause dose dumping [40], while developed ChrDDS showed a slow rate of absorption of the drug with a Tmax of 9 h and less Cmax (490.16 ± 33.95 ng/ml) value. A lower value of AUC0–24 (2181.65 ± 309.18 ng h/ml) from the marketed formulation confirmed a lesser extent of absorption of the drug as compared to developed DDS AUC0–24 (4958.51 ± 418.29 ng h/ml). Because of the slow rate of elimination (ke = 0.10 ± 0.03 h−1) and clearance (CL = 0.112 ± 0.05 ml/h), half-life (t1/2 = 7.27 ± 0.71 h), and mean residence time (MRT = 14.08 ± 1.21 h) of MTS ChrDDS have been increased by 3.07 and 5.89-fold, respectively, as compared to marketed formulation. Formulated DDS displayed a Tlast of 24 h which was more than 5 times as Tlast of Montek 10 (Table 4). It was established that developed ChrDDS displayed level A IVIVC with a correlation coefficient value of 0.9899 from FDR in-vitro dissolution and FDA in-vivo analysis (Fig. 4).
For a sustained and prolonged release of the drug, a dosage form needs to adhere to the intestinal wall for a longer time. Mucoadhesive strength was determined from the ex-vivo study for assurance of adherence. From the literature, it has been found that HPMC K4M has maximum mucoadhesive strength (due to more hydroxyl groups) followed by Carbopol [41]. In comparison with the second half of the DDS, the first part (T1F1) had less coating polymer applied to it (T2F3). Henceforth, coated T2F3 tablets displayed a greater mucoadhesive strength value as well as a longer mucoadhesive time. By using X-ray radiography, the path of coated matrix tablets has been mapped (Fig. 5). Two hours after giving the BaS04 integrated capsule, a radiogram revealed that the stomach region had matrix tablets, and 6 and 9 h later, the intestines contained the capsule. Stability studies proved the intactness of developed DDS for 6 months with a similarity factor between 87 and 90. A slight decrease in the drug content can be attributed to the degradation of the pure drug [30]. Statistical analysis of the drug release data from stability studies showed a p value greater than 0.05 confirming an insignificant difference between the optimized formulations [42].
To deal with early morning symptoms of asthma drug should reach the absorption site when symptoms are at their peak intensity. In this study, an in-vivo and radiographic study performed on rabbits shows the plasma concentration of MTS and time-dependent mobility of the previously developed dosage form as per the proposed hypothesis. An ex-vivo study has confirmed the required mucoadhesive strength and time [43,44,45,46].
Conclusion
The developed ChrDDS was efficiently characterized for mucoadhesive strength, pharmacokinetic parameters determination, time-dependent mobility, in-vitro in-vivo correlation, and stability studies. Results from HPLC method development were used in the determination of non-compartment pharmacokinetic parameters. The in-vitro dissolution data showed similarity with the in-vivo pharmacokinetic data and Level-A IVIVC was established. The in-vivo study and X-ray radiography proved the sustained and controlled release of MTS for chronotherapy of asthma with minimum risk of dose dumping.
In the future, pharmacodynamic studies need to be performed on animal models with a similar circadian cycle as humans. Additionally, a pilot study needs to be done to check the challenges of scale-up from laboratory to industry.
Availability of data and materials
All data and materials are available on request.
Abbreviations
- CHDDS:
-
Chronotherapeutic drug delivery system
- DDS:
-
Drug delivery system
- CCTs:
-
Compressed coated tablets
- DOE:
-
Design of experiment
- IVIVC:
-
In-vitro in-vivo correlation
- HPLC:
-
High-performance liquid chromatography
- HPMC:
-
Hydroxy propyl methyl cellulose
- RSD:
-
Relative standard deviation
- FDA:
-
Fraction of drug absorbed
- FDR:
-
Fraction of drug released
- MTS:
-
Montelukast sodium
- IS:
-
Internal standard
- C max :
-
Maximum concentration
- T max :
-
Time to reach maximum concentration
- V d :
-
Volume of distribution
- R t :
-
Retention time
- AUC:
-
Area under the curve
- CL:
-
Clearance
- MRT:
-
Minimum residence time
- T 1/2 :
-
Half-life
- LOD:
-
Limit of detection
- LOQ:
-
Limit of quantification
- SLS:
-
Sodium lauryl sulfate
References
Altman LC, Munk Z, Seltzer J, Noonan N, Shingo S, Zhang J, Reiss TF, Asthma M, Group S, Diego S (1998) A placebo-controlled, dose-ranging study of montelukast, a cysteinyl leukotriene—receptor antagonist. J Allergy Clin Immunol 102:50–56
Canadian Institutes of Health Research (2022) Montelukast drugbank.com. In: Drugbank. https://pubchem.ncbi.nlm.nih.gov/compound/23663996
National Center for Biotechnology Information (2023) Montelukast Pubchem. National Library of Medicine, National Institutes of Health, Department of Health and Human Services USA.gov. https://www.ptonline.com/articles/how-to-get-better-mfi-results
Pajaron-Fernandez M, Garcia-Rubia S, Sanchez-Solis M, Garcia-Marcos L (2006) Montelukast administered in the morning or evening to prevent exercise-induced bronchoconstriction in children. Pediatr Pulmonol 41:222–227. https://doi.org/10.1002/ppul.20377
Trial D (2012) Montelukast, a once-daily leukotriene receptor antagonist, in the treatment of chronic asthma. Hispanic 158:1213–1220
Noonan MJ, Chervinsky P, Brandon M, Zhang J, Kundu S, McBurney J, Reiss TF (1998) Montelukast, a potent leukotriene receptor antagonist, causes dose-related improvements in chronic asthma. Eur Respir J 11:1232–1239. https://doi.org/10.1183/09031936.98.11061232
Marzouk MAEH, Darwish MK, Yassin GE, El-Fattah MAA (2022) Pulsatile chronotherapeutic drug delivery for controlling early morning surge in blood pressure; effect of coating on eplerenone in-vitro, in-vivo release and urinary Na/K ratio. Braz J Pharm Sci 58:1–16. https://doi.org/10.1590/s2175-97902022e19306
Dallaspezia S, van Jaarsveld A (2016) Antidepressant chronotherapeutics in a group of drug free outpatients. Psychiatry Res 241:118–121. https://doi.org/10.1016/j.psychres.2016.04.104
Smolensky MH, Lemmer B, Reinberg AE (2007) Chronobiology and chronotherapy of allergic rhinitis and bronchial asthma. Adv Drug Deliv Rev 59:852–882. https://doi.org/10.1016/j.addr.2007.08.016
Nainwal N (2012) Chronotherapeutics—a chronopharmaceutical approach to drug delivery in the treatment of asthma. J Control Release 163:353–360. https://doi.org/10.1016/j.jconrel.2012.09.012
JS, Scs, (2022) Exploration of Parteck® SRP 80 and hypromellose for chronomodulated release of LTD4 receptor antagonist and statistical optimization using central composite design. AAPS PharmSciTech. https://doi.org/10.1208/s12249-022-02415-5
US Department of Health and Human Services, FDA, CDER C (2014) Guidance for Industry ANDA submissions—content and format of Abbreviated New Drug Applications
Silva JB, Ferreira SBS, Reis AV, Cook MT, Bruschi ML (2018) Assessing mucoadhesion in polymer gels: the effect of method type and instrument variables. Polymers (Basel) 10:1–19. https://doi.org/10.3390/polym10030254
Sokar MS, Hanafy AS, El-Kamel AH, El-Gamal SS (2013) Pulsatile core-in-cup valsartan tablet formulations: in vitro evaluation. Asian J Pharm Sci 8:234–243. https://doi.org/10.1016/j.ajps.2013.09.006
Acharya PC, Shetty S, Fernandes C, Suares D, Maheshwari R, Tekade RK (2018) Preformulation in drug research and pharmaceutical product development. Elsevier Inc, Amsterdam
Bandopadhyay S, Bandyopadhyay N, Deb PK, Singh C, Tekade RK (2018) Preformulation studies of drug substances, protein, and peptides: role in drug discovery and pharmaceutical product development. Elsevier Inc, Amsterdam
Singh B, Saini G, Vyas M, Verma S, Thakur S (2019) Optimized chronomodulated dual release bilayer tablets of fexofenadine and montelukast: quality by design, development, and in vitro evaluation. Futur J Pharm Sci. https://doi.org/10.1186/s43094-019-0006-9
Lee HR, Park HJ, Park JS, Park DW, Ho MJ, Kim DY, Lee HC, Kim EJ, Song WH, Park JS, Choi YS, Kang MJ (2021) Montelukast microsuspension with hypromellose for improved stability and oral absorption. Int J Biol Macromol 183:1732–1742. https://doi.org/10.1016/j.ijbiomac.2021.05.151
Xie J, Wang Z (2021) Can remdesivir and its parent nucleoside GS-441524 be potential oral drugs? An in vitro and in vivo DMPK assessment. Acta Pharm Sin B 11:1607–1616. https://doi.org/10.1016/j.apsb.2021.03.028
Torpac Inc (1989) Torpac gelatin capsules. Torpac Inc, New Jersey
Elhabal SF, Ghaffar SA, Hager R, Elzohairy NA, Khalifa MM, Mohie PM, Gad RA, Omar NN, Elkomy MH, Khasawneh MA, Abdelaal N (2023) Development of thermosensitive hydrogel of Amphotericin-B and Lactoferrin combination-loaded PLGA-PEG-PEI nanoparticles for potential eradication of ocular fungal infections: in-vitro, ex-vivo and in-vivo studies. Int J Pharm X. https://doi.org/10.1016/j.ijpx.2023.100174
Ranjan OP, Nayak UY, Reddy MS, Dengale SJ, Musmade PB, Udupa N (2013) Development and validation of RP-HPLC method with ultraviolet detection for estimation of montelukast in rabbit plasma: application to preclinical pharmacokinetics. J Young Pharm 5:133–138. https://doi.org/10.1016/j.jyp.2013.10.006
Emami J (2006) In vitro-in vivo correlation: from theory to applications. J Pharm Pharm Sci 9:31–51
Navamanisubramanian R, Nerella R, Duraipandian C, Seetharaman S (2018) Quality by design approach for optimization of repaglinide buccal tablets using Box–-Behnken design. Futur J Pharm Sci 4:265–272. https://doi.org/10.1016/j.fjps.2018.10.002
Alagili MF, AlQuadeib BT, Ashri LY, Ibrahim MA (2023) Optimization and evaluation of Lisinopril mucoadhesive sustained release matrix pellets: In-vitro and ex-vivo studies. Saudi Pharm J. https://doi.org/10.1016/j.jsps.2023.06.023
Georgy KR, Farid RM, Latif R, Bendas ER (2019) A new design for a chronological release profile of etodolac from coated bilayer tablets: in-vitro and in-vivo assessment. J Adv Res 15:37–47. https://doi.org/10.1016/j.jare.2018.08.003
SJ & SCS (2023) Exploration of Polymethacrylate and hypromellose for the development of a non-sulfhydryl ACE inhibitor mucoadhesive system using Box–Behnken design: in-vitro and ex-vivo evaluation. Drug Dev Ind Pharm. https://doi.org/10.1080/03639045.2023.2184636
Ranjan OP, Nayak UY, Reddy MS, Dengale SJ, Musmade PB, Udupa N (2014) Osmotically controlled pulsatile release capsule of montelukast sodium for chronotherapy: statistical optimization, in vitro and in vivo evaluation. Drug Deliv 21:509–518. https://doi.org/10.3109/10717544.2013.853209
Lee R (1989) Radiation protection in veterinary radiology. Vet Rec 103:97–100
Tiwari SK, Singh DK, Ladumor MK, Chakraborti AK, Singh S (2018) Study of degradation behaviour of montelukast sodium and its marketed formulation in oxidative and accelerated test conditions and prediction of physicochemical and ADMET properties of its degradation products using ADMET Predictor™. J Pharm Biomed Anal 158:106–118. https://doi.org/10.1016/j.jpba.2018.05.040
Ferlenghi F, Giorgio C, Incerti M, Guidetti L, Chiodelli P, Rusnati M, Tognolini M, Vacondio F, LA Mor M (2021) Metabolic soft spot and pharmacokinetics: functionalization of C-3 position of an Eph–ephrin antagonist featuring a bile acid core as an effective strategy to obtain oral bioavailability in mice. Pharmaceuticals (Basel) 15(1):41
Royce A, Li S, Weaver M, Shah U (2004) In vivo and in vitro evaluation of three controlled release principles of 6-N-cyclohexyl-2′-O-methyladenosine. J Control Release 97:79–90. https://doi.org/10.1016/j.jconrel.2004.02.016
Long CM (2014) Biopharmaceutical considerations and in vitro-in vivo correlations (ivivcs) for orally administered amorphous formulations. U620097:1
Gyarmati B, Stankovits G, Szilágyi BÁ, Galata DL, Gordon P, Szilágyi A (2022) A robust mucin-containing poly(vinyl alcohol) hydrogel model for the in vitro characterization of mucoadhesion of solid dosage forms. Colloids Surf B Biointerfaces 213:1–9. https://doi.org/10.1016/j.colsurfb.2022.112406
Hoffmann A, Daniels R (2018) A novel test system for the evaluation of oral mucoadhesion of fast disintegrating tablets. Int J Pharm 551:141–147. https://doi.org/10.1016/j.ijpharm.2018.09.001
ICH (2003) International conference on harmonization (ICH). Guidance for industry: Q1A(R2) stability testing of new drug substances and products. Ich Harmon Tripart Guidel 4:24
ICH. Q2B validation of analytical procedures: methodology. In: Proceedings of the international conference on harmonization expert working group. Geneva, Switz
Sabir AM, Moloy M, Bhasin PS (2016) Hplc method development and validation: a review. Int Res J Pharm 4:39–46. https://doi.org/10.7897/2230-8407.04407
Aashli, Reddy SG, Siva Kumar B, Prashanthi K, Murthy HCA (2023) Fabricating transdermal film formulations of montelukast sodium with improved chemical stability and extended drug release. Heliyon. https://doi.org/10.1016/j.heliyon.2023.e14469
Mašková E, Kubová K, Raimi-Abraham BT, Vllasaliu D, Vohlídalová E, Turánek J, Mašek J (2020) Hypromellose—a traditional pharmaceutical excipient with modern applications in oral and oromucosal drug delivery. J Control Release 324:695–727. https://doi.org/10.1016/j.jconrel.2020.05.045
Bala Ramesha Chary R, Vani G, Madhusudan Rao Y (1999) In vitro and in vivo adhesion testing of mucoadhesive drug delivery systems. Drug Dev Ind Pharm 25:685–690. https://doi.org/10.1081/DDC-100102226
Biswas N, Sahoo RK, Guha A, Kuotsu K (2014) Chronotherapeutic delivery of hydroxypropylmethylcellulose based mini-tablets: an in vitro-in vivo correlation. Int J Biol Macromol 66:179–185. https://doi.org/10.1016/j.ijbiomac.2014.02.036
Gazioglu I, Evrim Kepekci Tekkeli S, Tartaglia A, Aslan C, Locatelli M, Kabir A (2022) Simultaneous determination of febuxostat and montelukast in human plasma using fabric phase sorptive extraction and high performance liquid chromatography-fluorimetric detection. J Chromatogr B Anal Technol Biomed Life Sci 1188:123070. https://doi.org/10.1016/j.jchromb.2021.123070
Tintinger GR, Feldman C, Theron AJ, Anderson R (2010) Montelukast: More than a cysteinyl leukotriene receptor antagonist? Sci World J 10:2403–2413. https://doi.org/10.1100/tsw.2010.229
Shakya A, Arafat T, Hakooz N, Abuawwad A, Al-Hroub H, Melhim M (2014) High-performance liquid chromatographic determination of montelukast sodium in human plasma: application to bioequivalence study. Acta Chromatogr 26:457–472. https://doi.org/10.1556/AChrom.26.2014.3.5
Okumu A, DiMaso M, Löbenberg R (2008) Dynamic dissolution testing to establish in vitro/in vivo correlations for montelukast sodium, a poorly soluble drug. Pharm Res 25:2778–2785. https://doi.org/10.1007/s11095-008-9642-z
Acknowledgements
The management of PES University in Bengaluru, India is to be thanked by the authors for granting Mrs. Saniya Jawed a scholarship and all the facilities and assistance she needs to carry out this research. Pacto Pharmaceuticals Pvt Ltd. of Mumbai, India, is thanked by the authors for providing size 5 gelatin capsules. The authors express deep gratitude towards Certara University USA for providing a free Phoenix WinNonlin software trial license.
Funding
This work has not received any grant from public, commercial, or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
SJ carried out formulation and evaluation and wrote the original draft. CSS contributed to reviewing, editing, and supervision.
Corresponding author
Ethics declarations
Animal rights
White New Zealand rabbits (2–2.5 kg) were maintained as per the standard protocols in the Animal House of PES College of Pharmacy, PES University, Bengaluru, Karnataka, India. X-ray radiography and pharmacokinetic studies were performed as per approved guidelines of CPSCEA, Government of India, and were granted by IEAC of PES College of Pharmacy with ethical clearance number (PESCP/IAEC/128/2021-2022). All animals were kept in the Animal House of PES College of Pharmacy, PES University, Bengaluru, Karnataka, India, per the CPSCEA guidelines, Government of India.
Consent for publication
Authors declare no conflict of interest.
Competing interests
The authors declared no competing interests regarding the publication of current research work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jawed, S., Satish, C.S. IVIVC assessment, pharmacokinetic evaluation, and X-ray radiography mapping of Novel Parteck® SRP 80 and hypromellose-loaded LTD4 receptor antagonist chronosystem. Futur J Pharm Sci 9, 105 (2023). https://doi.org/10.1186/s43094-023-00552-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-023-00552-7