Abstract
Background
Iron deficiency anemia (IDA) constitutes a considerable nutritional problem in Egyptian preschool children. Moreover, IDA limits physical activity performance and interferes with children's development. Accordingly, we aim to investigate the correlation between IDA and hand dexterity and pinch grip strength in preschool children.
Results
This observational cross-sectional study encompassed the participation of 87 children, comprising both genders, with an age range of 5–6 years. The cohort was initially stratified into three distinct groups: Group A comprised 36 non-anemic children, group B included 25 children with mild iron-deficiency anemia (IDA), and group C consisted of 26 children with moderate IDA. After group delineation, comprehensive laboratory analyses were performed on all participants to assess for IDA, involving a thorough examination of their complete blood picture, hemoglobin (Hb) levels, serum iron levels, and serum ferritin levels. The evaluative metrics employed in this study encompassed the Bruininks-Oseretsky Test of Motor Proficiency-Second Edition (BOT-2) and the Baseline Mechanical Pinch Gauge. These instruments were utilized to assess manual dexterity and pinch strength, specifically tip-to-tip and tripod strength. This investigation revealed a positive correlation between Hb, serum iron, and serum ferritin levels with both manual dexterity and pinch strength across all three groups.
Conclusion
This study highlights that IDA negatively affects hand dexterity and pinch grip strength in preschool children. Managing IDA early is crucial for improving their physical performance and overall development.
Similar content being viewed by others
1 Background
Anemia refers to the reduced oxygen-carrying capacity of the blood because of an overall decrease in hemoglobin (Hb) concentration that, in turn, leads to tissue hypoxia [1]. Furthermore, anemia causes central nervous system dysfunction, including declined cognitive functions, delayed growth and motor development, and neurological symptoms. These symptoms include paresthesia, weakness, clumsiness, and an unsteady gait. Iron deficiency (ID) accounts for around 50% of all cases of anemia [2]. Iron is essential for Hb production in red blood cells, oxygen delivery to peripheral tissues, and the regulatory role of mitochondria in muscular energy metabolism [3]. The World Health Organization (WHO) has stated that iron deficiency anemia (IDA) represents a major dietary deficit in children [4] that affects 48.5% of Egyptian preschoolers [5]. The prevalence of IDA among children in the Nile Delta was estimated to be 17.19% [6]. Early-life ID disrupts brain energy metabolism, reduces myelin formation, and affects dopamine signaling, consequently causing neurodevelopmental deficits [7]. Notably, IDA influences the development of upper extremity skills such as reach and grasp [8]. Additionally, Ayala et al. [9] have shown that infants with DA have lower scores in fine motor skills and social–emotional areas.
Pinch strength is a prehension where two or three fingers collaborate with thumb movements to manipulate objects without using the palm [10]. Mainly, it is the predominant force generated by the synchronized contractions of the muscles in both the forearm and hand during hand grip [11]. Pinch strength includes three clinically measured categories: tip, key, and palmar pinch [12]. Accordingly, pinch strength is a good parameter in evaluating the hand as a predictor of hand function [13]. Additionally, Dougherty et al. [14] studied hand grip strength (HGS) in anemic children, concluding they have weaker grip strength than the control group.
Manual dexterity refers to the skill of manipulating objects by coordinating hand and finger movements and the capacity to synchronize minor muscle movements with the eye, hand, and finger [15]. Generally, it consists of muscle strength, force control, tactile sensation, and cognitive acuity [16]. Manual dexterity development is crucial for general development [17], rendering it the fundamental element to investigate while examining manipulative skills [18]. Strong handgrips and good hand dexterity are essential for school-age children, as many tasks throughout the school day require using their hands [19]. Efficient manipulation of objects requires sufficient fine motor control, enabling infants to develop perception awareness [20]. Although IDA results in permanent delays in gross and fine motor skills [21, 22], limited studies have investigated its effect on hand dexterity and pinch strength among preschool children. Accordingly, we aimed to examine the IDA association with hand dexterity and pinch strength in preschool children.
2 Methods
2.1 Study design and sample size
This observational cross-sectional study was conducted at the Outpatient Clinic of Pediatrics, Zagazig University Hospitals, from May 2022 to July 2023.
Herein, we utilized G*POWER statistical software (version 3.1.9.2; Franz Faul, Universitat Kiel, Germany) to calculate the sample size using the following parameters: α = 0.05, power = 80%, and moderate effect size = 0.3. This calculation was conducted depending on the findings of a pilot study that assessed the correlation between iron level and manual dexterity in 10 children. Eventually, we employed N = 85 as the required sample size for this study.
2.2 Subjects
This study enrolled 87 children of both sexes aged 5–6 years. First, children were subdivided into three groups: group A, which comprised 36 non-anemic children; group B, which included 25 children with mild iron deficiency anemia (IDA); and group C, which had 26 children with moderate IDA.
The inclusion criteria were as follows: (A) non-anemic children having a normal Hb level ≥ 11.5 g/L [23], serum iron > 60 mcg/dL [24], and serum ferritin level > 15 ng/mL in the absence of infection [25]; (B) anemic children having microcytic hypochromic anemia: Hb < 11.5 g/L (Hb of 11.0–11.4 and 8.0–10.9 refers to mild and moderate anemia, respectively) [4], serum iron < 60 mcg/dL [24], and serum ferritin < 15 ng/mL in the absence of infection [25]; (C) right-handed children; (D) children with a body mass index (BMI) of 15.2–15.5 kg/m2 [26].
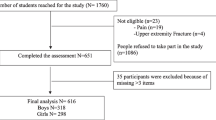
The exclusion criteria included the following: (A) deformity of the upper limb joints, either congenital or acquired; (B) unhealed upper limb bone fracture; (C) systemic diseases causing anemia such as hepatic dysfunction, renal impairment, or a previous bone disease; (D) transfusion blood within three months before evaluating the hematological parameters; (E) muscle fibers trauma in the previous one year, or using drugs that affects strength; (F) upper extremity neuromuscular disorders; (G) participation within a constant sports activity including the upper limbs; (H) visual, auditory, or vestibular defects; (I) history of hand injuries, operations, or other hand function limitations; (J) iron deficiency anemia secondary to non-nutritional causes (Fig. 1).
2.3 Laboratory investigations
Specific protocol and procedures were followed during the assessment of the laboratory investigations as follows: Blood samples were aseptically drawn from a peripheral vein and divided into multiple portions. A portion was placed in an EDTA tube for complete blood count (CBC) analysis. Another portion was left to clot in a plain tube and then centrifuged to separate the serum. The obtained serum was preserved at − 20 °C until testing [27]. The CBC was conducted using an automated blood cell counter (Sysmex-Xs 800i), serum iron levels were assessed with an AU 480-Chemistry auto-analyzer (Beckman Coulter Diagnostics-USA), and serum ferritin levels were determined through ELISA using DRG® Ferritin [EIA-1872].
To maintain data quality, standard operating procedures were followed throughout all laboratory processes. Analyses were conducted in line with the manufacturer's guidelines, and control reagents were employed with hematology and clinical chemistry analyzers to verify result reproducibility.
2.3.1 Assessment of Hb level
The Hb level was assessed utilizing a completely automated blood cell counter (Sysmex-Xs 800i), a fluorescent flow-cytometric hematology analyzer that precisely measures red and white blood cell count and platelets [28, 29]. The reliability of this analyzer is comparable to that of the standard manual approach, as indicated by r2 > 0.95 [30] and a correlation coefficient of 0.908 [31].
2.3.2 Assessment of serum iron
Serum iron was evaluated with the idealistic AU 480-Chemistry auto-analyzer (Beckman Coulter Diagnostics, USA) due to its high reliability, precision, accuracy, and acceptable variation coefficients for day-to-day impression [32, 33].
2.3.3 Assessment of serum ferritin
Herein, we analyzed serum ferritin levels employing a ferritin quantitative solid-phase enzyme-linked immunosorbent assay (ELISA) kit using DRG® Ferritin [EIA-1872], which had a specificity of 83% and sensitivity of 5.0 ng/mL, respectively. Also, it had an optical density of 0–2 (OD) or larger at the 450 nm wavelength. The intra- and inter-assay precision coefficient of variation (CV) was determined by replicate determinations of three different serum samples in one assay 3.6%, 5.7%, 3.5%, 4.2%, 5.1%, and 6.6%, respectively.
2.4 Outcome measures
2.4.1 Manual hand dexterity
The Bruininks-Oseretsky Test of Motor Proficiency, Second Edition (BOT-2) constitutes a widely recognized assessment tool utilized by occupational and physical therapists in clinical and school practice settings to measure manual hand dexterity. It is a norm-referenced and standardized measure that provides valuable insights into the motor skills of individuals [34]. The BOT-2 assesses the fine and gross motor skills of children aged 4–21 years by individual administration. In addition, BOT-2 demonstrated high psychometric quality, with good internal consistency (r ≥ 0.80), outstanding inter-rater reliability (r = 0.98), strong test–retest reliability (r ≥ 0.80), and content and concurrent validity [34,35,36].
Manual dexterity assessment involved directed activities: grasping, reaching, and bimanual coordination with small objects. These objects involve placing pegs on a pegboard, sorting cards, making dots in circles, stringing small blocks, picking plastic pennies, and placing them into the box. The child was instructed to perform the task with the utmost precision and promptness, prioritizing accuracy and timing. By incorporating speed, timed activities can accurately distinguish the dexterity level [36]. The scoring process involved determining the raw score for each test item using the Administration Easel. The raw results of each child were initially interpreted into point scores, thereby calculating the overall point scores by summing all the points. Eventually, the norm tables outlined in the handbook were utilized to convert the point scores of the subset into scale scores and obtain standard scores for statistical analysis [34].
2.4.2 Pinch strength
Herein, we deployed a Baseline Mechanical Pinch Gauge (0–60 lb) for measuring pinch strength (tip-to-tip and tripod) for all children. The intra-rater and inter-rater reliability for the pinch gauge (tip-to-tip grasp) was 0.986 and 0.995, respectively [37, 38]. The evaluation procedures were performed by instructing each child to sit in an armchair with stationary armrests and a backrest. They were then asked to position their upper extremity in the following manner: Shoulder adducted and neutrally rotated, elbow flexed at 90°, forearm in a neutral position, wrist in a neutral position between 0° and 30° extension, and ulnar deviation between 0 and 15°. In the tip-to-tip pinch strength assessment, the pinch gauge was positioned between the thumb and index fingertips.
In the tripod pinch strength assessment, the pinch gauge was positioned between the pads of the thumb, index, and middle fingers. Flexing the ulnar fingers and the interphalangeal joint of the thumb was important to achieve maximum pinch force during the pinch assessment [39,40,41]. Each child was then instructed to forcefully squeeze as long and tightly as possible to achieve optimal outcomes while avoiding abrupt movements until the needle came to a halt. The measurement was recorded when the needle stopped moving upward (the inner dial in-lb). Three trials were conducted using a 3-s contraction followed by a 10-s rest period between each trial to prevent fatigue. Eventually, the mean of the three trials was calculated and utilized for data analysis [40, 41].
2.5 Statistical analysis
The statistical analysis was conducted employing the SPSS software (version 25 for Windows). The characteristics of the subjects were compared between groups using the MANOVA test for numerical data and the Chi-squared test for categorical data. Moreover, the normality of the data was assessed through the Shapiro–Wilk test. Levene's test for homogeneity of variances was performed to assess the similarity between groups. A one-way MANOVA was used to compare Hb, serum iron, ferritin, manual dexterity, pinch tip-to-tip, and pinch tripod between different groups. Subsequent multiple comparisons were conducted using Tukey's test for post hoc analysis. The Pearson correlation coefficient was employed to examine the association between the variables. P < 0.05 indicated a statistical significance for all statistical tests.
3 Result
3.1 Subject characteristics
Table 1 demonstrates that the groups did not significantly differ in age, weight, height, BMI, and sex distribution (P > 0.05).
3.2 Comparison of Hb, serum iron, ferritin, manual dexterity, pinch tip-to-tip, and pinch tripod between all groups
The MANOVA test results indicated a significant group effect (F = 126.57, P = 0.001, η2 = 0.91). The findings demonstrated that Hb, serum iron, and ferritin levels were significantly reduced in groups B and C more than in group A (P < 0.001). Moreover, group C exhibited significantly decreased Hb, serum iron, and ferritin levels compared with group B (P < 0.001). The manual dexterity, pinch tip-to-tip, and pinch tripod of groups B and C significantly reduced compared with group A (P < 0.001). Additionally, these three parameters were significantly reduced in group C compared to group B (P < 0.01, Tables 2, 3).
3.3 Correlation between Hb, serum iron, ferritin and manual dexterity, pinch tip-to-tip, and pinch tripod
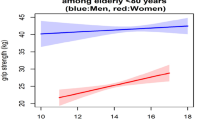
Regarding Hb levels in group A, the results revealed a strong positive correlation between Hb levels and manual dexterity, as well as a moderate positive significant correlation between Hb with pinch tip-to-tip and tripod (panel I).
Regarding Hb levels in group B, the results revealed a moderate positive correlation between Hb levels and manual dexterity, pinch tip-to-tip, and tripod (panel I).
Regarding Hb in group C, the results revealed a strong positive correlation between Hb levels and manual dexterity, pinch tip-to-tip, and tripod (panel I).
Regarding serum iron in three groups, results revealed a moderate positive significant correlation between serum iron with manual dexterity, pinch tip-to-tip, and pinch tripod in group A. In addition, the result revealed a strong positive significant correlation between serum iron and manual dexterity, while a moderate positive significant correlation was found between serum iron with pinch tip-to-tip and tripod in groups B and C (panel II).
Regarding serum ferritin in three groups, the results revealed a moderate positive significant correlation between ferritin and manual dexterity, pinch tip-to-tip, and tripod in group A. Additionally, there was a strong positive significant correlation between ferritin and manual dexterity, while there was a moderate positive significant correlation between ferritin with pinch tip-to-tip and tripod in groups B and C (panel III) (Fig. 2).
Simple linear regression analyses. Panel (I) hemoglobin level (g/dl) and manual dexterity, pinch tip-to-tip (lb), and pinch tripod (lb) in different 3 studied groups (r: Pearson correlation coefficient; *P < 0.05; **P < 0.01; ***P < 0.001). Panel (II) serum iron level (µg/dl) and manual dexterity, pinch tip-to-tip (lb), and pinch tripod (lb) in different 3 studied groups (r: Pearson correlation coefficient; *P < 0.05; **P < 0.01; ***P < 0.001). Panel (III) serum ferritin level (ng/ml) and manual dexterity, pinch tip-to-tip (lb), and pinch tripod (lb) in different 3 studied groups (r: Pearson correlation coefficient; *P < 0.05; **P < 0.01; ***P < 0.001)
4 Discussion
The present study delves into the intricate relationship between IDA, hand dexterity, and pinch grip strength in preschool children. With a robust observational cross-sectional design involving 87 children aged 5–6 years, the investigation systematically examined the impact of varying degrees of IDA on manual dexterity and pinch strength. Stratified into distinct groups based on their anemic status, our findings illuminate a noteworthy correlation between Hb, serum iron, and serum ferritin levels with the observed manual dexterity and pinch strength. As we navigate the discussion, we will delve into the implications of these correlations, shedding light on the potential repercussions of IDA on physical activity performance and developmental strategies in preschool children. Additionally, this discourse aims to underscore the significance of early intervention and effective management strategies to mitigate IDA's adverse effects and promote this vulnerable demographic's overall well-being.
This study revealed that manual dexterity significantly differed between anemic and non-anemic children in the three groups. The lower score in manual dexterity among anemic children may be attributed to an alteration of myelin formation, which affects motor skill development. This is consistent with Shafir et al. [8], who manifested that ID delays and alters corticospinal myelination, thereby delaying the typical development and mastery of motor skills. Furthermore, myelination throughout the early years of life accelerates the conduction velocity along this tract, gradually allowing for the development of both motor performance and skill to reach an adult-like level [42].
The results of Pollitt et al. [43] supported our result, which revealed that scores for both gross and fine motor skills significantly differed between anemic and non-anemic preschool children. Additionally, they indicated that anemic children exhibited lower motor scale scores than non-anemic children. Furthermore, Shafir et al. [8] have shown that children with severe chronic ID in infancy had persistently low motor scores that remained unimproved over time. Iron is crucial in synthesizing myelin; therefore, ID has been found to disrupt the myelination process [44,45,46]. Herein, pinch strength (tip-to-tip and tripod) exhibited a significant difference between anemic and non-anemic children in all groups. This lower pinch strength among anemic children may be due to decreased Hb levels that negatively affect oxygen delivery to musculoskeletal tissue, which agrees with Giulivi and Davies [47] and Grune [48]. Alley et al. [48] have consistently stated that anemic patients had significantly weaker HGS than non-anemic patients. Notably, Zhang and Enns [49] have explained the probable cause of neuronal abnormalities: Heme compounds contain approximately 70% of total body iron (e.g., Hb and myoglobin). Because iron is vital to cells' structural and functional integrity [44, 50], IDA patients complain of peripheral weakness and tingling sensation in their limbs [51].
Furthermore, anemia has been elucidated to be related to reduced muscle mass and strength [52]. In all groups, Hb, serum iron, and serum ferritin levels were significantly positively correlated with manual dexterity. This could be attributed to the reduced oxygen-carrying capability of Hb in the cerebral circulation as well as nerve growth factor downregulation. These findings are corroborated by Hübner et al. [53] and Bastian et al. [54], who have shown that ID impacts oligodendrocytes by disrupting the functions of iron-containing enzymes and several key enzymes. These key enzymes are involved in iron-dependent metabolism, neurotransmitter metabolism, respiratory chain, DNA, and lipid formation. Eventually, this malfunction leads to abnormal synaptic structure, hypomyelination, and nerve growth factor downregulation. The impact of anemia on children's neurobehavioral development may be ascribed to the diminished ability of Hb to transport oxygen to the cerebral blood flow, resulting in a subsequent decline in energy consumption [55]. Similarly, a study conducted in Chile on anemic infants elucidated that performance positively correlates with Hb concentration; the lower the Hb level, the lower the developmental scores [56].
Likewise, Guo et al. [57] have indicated that serum ferritin levels had a linear association with gross motor, fine motor, and language scores. Our findings represented that pinch strength had significant positive correlations with Hb, serum iron, and serum ferritin levels in all groups. These correlations may be due to reduced muscle oxygen supply, functional and structural changes in muscle fibers, and anemia-caused fatigue. Consistently, Deveci et al. [58] have explained that reduced Hb levels are correlated with structural and functional alterations in the capillaries and muscle fiber [59], fatigue [60], physical performance [61], and muscle strength impairment [61]. Similarly, a decreased Hb level has been shown to directly correlate with decreased HGS in elderly Australians [62, 63], which is attributed to tissue hypoxia reducing oxygen supply to the muscles, directly affecting muscle strength, regardless of anemia [61]. Additionally, Gi et al. [64] have demonstrated that anemia is significantly related to HGS, particularly in Korean adults over 19 years old.
4.1 Limitations and recommendations
While our study sheds light on the correlation between IDA, hand dexterity, and pinch grip strength in preschool children, certain limitations merit acknowledgment. A cross-sectional study design can only establish correlations and associations but cannot determine causality. The excessive cost of laboratory analysis investigates serum iron and ferritin. Finally, the enrolment of the control group, which consisted of children born healthy and without any growth problems, took a long duration.
Future longitudinal research is crucial for establishing temporal relationships between IDA with pinch grip strength and hand dexterity. Diversifying the sample to include various demographics enhances external validity. Recognizing the need for replication studies in diverse populations is indeed valuable. Replication studies conducted in various geographic locations and cultural contexts help to determine the consistency and robustness of findings across different populations. Future studies for early identification and management of IDA would provide practical implications for healthcare professionals and parents. Future studies should meticulously address confounding variables, providing a more nuanced understanding of the observed associations. Additionally, investigating the impact of targeted IDA interventions on motor skills and development could inform preventive strategies. Despite these limitations, our findings underscore the need for ongoing research to guide evidence-based interventions and public health initiatives to ameliorate IDA's developmental effects in preschool children.
5 Conclusion
This study reveals a clear association between IDA and impaired manual dexterity and diminished pinch grip strength in preschool children. The positive correlation observed between hemoglobin, serum iron, and serum ferritin levels with both manual dexterity and pinch strength underscores the impact of IDA on fine motor abilities in this age group. These findings collectively emphasize the detrimental effects of IDA on developing crucial fine motor skills in preschool children.
Availability of data and materials
Data of the present study can be made applicable upon reasonable request to the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- BOT-2:
-
Bruininks-Oseretsky Test of Motor Proficiency, Second Edition
- CV:
-
Coefficient of variation
- OD:
-
Optical density
- ELISA:
-
Enzyme-linked immunosorbent assay
- Hb:
-
Hemoglobin
- HGS:
-
Hand grip strength
- ID:
-
Iron deficiency
- IDA:
-
Iron deficiency anemia
- r:
-
Pearson correlation coefficient
- P-value:
-
Probability value
- WHO:
-
World Health Organization
References
Deshpande NS, Yadav BM, Deshmukh S (2022) Clinical profile of anaemia with special reference to neurological changes at tertiary hospital. MedPulse Int J Med 21(2):57–60. https://doi.org/10.26611/10212125
Al-Mekhlafi MH, Surin J, Atiya AS, Ariffin WA, Mahdy AK, Abdullah HC (2008) Anaemia and iron deficiency anaemia among aboriginal schoolchildren in rural Peninsular Malaysia: an update on a continuing problem. Trans R Soc Trop Med Hyg 102(10):1046–1052. https://doi.org/10.1016/j.trstmh.2008.05.012
Kang C, Li Ji L (2012) Role of PGC-1α signaling in skeletal muscle health and disease. Ann N Y Acad Sci 1271(1):110–117. https://doi.org/10.1111/j.1749-6632.2012.06738.x
WHO (2023) Anaemia. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/anaemia.
Baker RD, Greer FR (2010) Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics 126(5):1040–1050. https://doi.org/10.1542/peds.2010-2576
El-Shanshory MR, Sherief LM, Hassab HM, Ragab SM, Yahia S, Mansour AK et al (2021) Prevalence of iron deficiency anemia and beta thalassemia carriers among relatives of beta thalassemia patients in Nile Delta region, Egypt: a multicenter study. J Egypt Public Health Assoc 96(1):27. https://doi.org/10.1186/s42506-021-00088-9
Bastian TW, Rao R, Tran PV, Georgieff MK (2020) The effects of early-life iron deficiency on brain energy metabolism. Neurosci Insights 15:2633105520935104. https://doi.org/10.1177/2633105520935104
Shafir T, Angulo-Barroso R, Su J, Jacobson SW, Lozoff B (2009) Iron deficiency anemia in infancy and reach and grasp development. Infant Behav Dev 32(4):366–375. https://doi.org/10.1016/j.infbeh.2009.06.002
Ayala R, Otero GA, Porcayo Mercado R, Pliego-Rivero FB (2008) Delayed CNS maturation in iron-deficient anaemic infants. Nutr Neurosci 11(2):61–68. https://doi.org/10.1179/147683008x301342
Duruöz MT (2014) Assessment of hand functions. In: Duruöz MT (ed) Hand function: a practical guide to assessment. Springer, New York, pp 41–51. https://doi.org/10.1007/978-1-4614-9449-2_3
McQuiddy VA, Scheerer CR, Lavalley R, McGrath T, Lin L (2015) Normative values for grip and pinch strength for 6- to 19-year-olds. Arch Phys Med Rehabil 96(9):1627–1633. https://doi.org/10.1016/j.apmr.2015.03.018
Mathiowetz V, Weber K, Volland G, Kashman N (1984) Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am 9(2):222–226. https://doi.org/10.1016/s0363-5023(84)80146-x
Secker DJ, Jeejeebhoy KN (2007) Subjective global nutritional assessment for children. Am J Clin Nutr 85(4):1083–1089. https://doi.org/10.1093/ajcn/85.4.1083
Dougherty KA, Bertolaso C, Schall JI, Smith-Whitley K, Stallings VA (2018) Muscle strength, power, and torque deficits in children with type SS sickle cell disease. J Pediatr Hematol Oncol 40(5):348–354. https://doi.org/10.1097/mph.0000000000001143
Gonzalez V, Rowson J, Yoxall A (2015) Development of the variable dexterity test: construction, reliability and validity. Int J Ther Rehabil 22:174–180. https://doi.org/10.12968/ijtr.2015.22.4.174
Wang YC, Magasi SR, Bohannon RW, Reuben DB, McCreath HE, Bubela DJ et al (2011) Assessing dexterity function: a comparison of two alternatives for the NIH toolbox. J Hand Ther 24(4):313–320. https://doi.org/10.1016/j.jht.2011.05.001
Edwards SJ, Buckland DJ, McCoy-Powlen JD (2002) Developmental and functional hand grasps. Slack, Thorofare
Priosti PA, Blascovi-Assis SM, Cymrot R, Vianna DL, Caromano FA (2013) Força de preensão e destreza manual na criança com Síndrome de Down. Fisioter Pesqui 20:278–285
Roshan P, Chandrashekar N, Likhitha J (2021) Influence of low BMI on handgrip strength, handgrip endurance and hand dexterity in school going children-a pilot study. Int J Sci Healthc Res 6(3):70–78
Pollitt E (2000) A developmental view of the undernourished child: background and purpose of the study in Pangalengan, Indonesia. Eur J Clin Nutr 54(Suppl 2):S2-10. https://doi.org/10.1038/sj.ejcn.1600999
Stoltzfus RJ (2001) Iron-deficiency anemia: reexamining the nature and magnitude of the public health problem. Summary: implications for research and programs. J Nutr 131(2s–2):697S-700S. https://doi.org/10.1093/jn/131.2.697S
Suryana MS, Sukandar D, Fitri Y, Ahmad A (2020) Assessment of anemia status on physical development skills of children under two years old in Aceh, Indonesia. J Nutr Sci Vitaminol (Tokyo) 66(Supplement):S463-s467. https://doi.org/10.3177/jnsv.66.S463
WHO (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization. https://www.who.int/publications/i/item/WHO-NMH-NHD-MNM-11.1
Soldin OP, Bierbower LH, Choi JJ, Choi JJ, Thompson-Hoffman S, Soldin SJ (2004) Serum iron, ferritin, transferrin, total iron binding capacity, hs-CRP, LDL cholesterol and magnesium in children; new reference intervals using the Dade Dimension Clinical Chemistry System. Clin Chim Acta 342(1–2):211–217. https://doi.org/10.1016/j.cccn.2004.01.002
WHO (2020) Serum ferritin concentrations for the assessment of iron status in individuals and populations: technical brief. World Health Organization. https://www.who.int/publications/i/item/9789240008526
WHO Growth reference data for 5–19 year. World Health Organization. https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators
Elkafafy M, Sakr MMA, Elsamanoudy MI, Abd Al-Samee HS (2021) Correlation between iron status and simple febrile seizures in children. Int J Med Arts 3(3):1714–1718. https://doi.org/10.21608/ijma.2021.79064.1320
Nagai T, Tanaka C (2006) Summary of the automated hematology analyzer XS-1000i. Sysmex J Int
Gunawardena D, Jayaweera S, Madhubhashini G, Lokumarakkala DD, Senanayake SJ (2017) Reliability of parameters of complete blood count with different storage conditions. J Clin Lab Anal. https://doi.org/10.1002/jcla.22042
Mokhtari M, Najafi S (2016) Evaluation of the correlation of automated and manual results of complete blood count in oncologic patients. Comp Clin Path. https://doi.org/10.1007/s00580-016-2319-9
Kim AH, Lee W, Kim M, Kim Y, Han K (2014) White blood cell differential counts in severely leukopenic samples: a comparative analysis of different solutions available in modern laboratory hematology. Blood Res 49(2):120–126. https://doi.org/10.5045/br.2014.49.2.120
Gasljevic V (2010) Method validation and measurement uncertainty. Biochem Med 20:57–63. https://doi.org/10.11613/BM.2010.007
Goswami K, Mookherjee S, Mazumdar I (2018) Calibration verification for Olympus Au 480 and Meril Autoquant Aq 400i automatic biochemistry auto analyser using seven analytes
Bruininks RH, Bruininks BD (2005) Bruininks-Oseretsky test of motor proficiency | Second Edition BOT-2
Cools W, Martelaer KD, Samaey C, Andries C (2009) Movement skill assessment of typically developing preschool children: a review of seven movement skill assessment tools. J Sports Sci Med 8(2):154–168
Deitz JC, Kartin D, Kopp K (2007) Review of the Bruininks-Oseretsky test of motor proficiency, Second Edition (BOT-2). Phys Occup Ther Pediatr 27(4):87–102
Mathiowetz V, Vizenor L, Melander D (2000) Comparison of Baseline Instruments to the Jamar Dynamometer and the B&L Engineering Pinch Gauge. Occup Ther J Res 20(3):147–162. https://doi.org/10.1177/153944920002000301
Mandanka N, Diwan S (2020) Intra rater and inter rater reliability of hand dynamometer and pinch gauge in children with spastic cerebral palsy. Indian J Physiother Occup Ther Int J 14(2):97–99. https://doi.org/10.37506/ijpot.v14i2.2619
McCoy W, Dekerlegand J (2011) Effect of the position of ulnar three digits on thumb to index tip to tip pinch strength. J Hand Ther 24(4):379. https://doi.org/10.1016/j.jht.2011.07.008
Alahmari KA, Kakaraparthi VN, Reddy RS, Silvian PS, Ahmad I, Rengaramanujam K (2019) Percentage difference of hand dimensions and their correlation with hand grip and pinch strength among schoolchildren in Saudi Arabia. Niger J Clin Pract 22(10):1356–1364. https://doi.org/10.4103/njcp.njcp_121_19
Mahmoud AG, Elhadidy EI, Hamza MS, Mohamed NE (2020) Determining correlations between hand grip strength and anthropometric measurements in preschool children. J Taibah Univ Med Sci 15(1):75–81. https://doi.org/10.1016/j.jtumed.2020.01.002
Lemon R, Armand J, Olivier E, Edgley S (1997) Skilled action and the development of the corticospinal tract in primates. In: Neurophysiology and neuropsychology of motor development. Mac Keith Press United Kingdom, London, pp 162-176
Pollitt E, Saco-Pollitt C, Leibel RL, Viteri FE (1986) Iron deficiency and behavioral development in infants and preschool children. Am J Clin Nutr 43(4):555–565. https://doi.org/10.1093/ajcn/43.4.555
Beard JL, Wiesinger JA, Connor JR (2003) Pre- and postweaning iron deficiency alters myelination in Sprague-Dawley rats. Dev Neurosci 25(5):308–315. https://doi.org/10.1159/000073507
Connor JR, Menzies SL (1996) Relationship of iron to oligodendrocytes and myelination. Glia 17(2):83–93. https://doi.org/10.1002/(sici)1098-1136(199606)17:2%3c83::Aid-glia1%3e3.0.Co;2-7
Ortiz E, Pasquini JM, Thompson K, Felt B, Butkus G, Beard J et al (2004) Effect of manipulation of iron storage, transport, or availability on myelin composition and brain iron content in three different animal models. J Neurosci Res 77(5):681–689. https://doi.org/10.1002/jnr.20207
Giulivi C, Davies KJ (1990) A novel antioxidant role for haemoglobin. The comproportionation of ferrylhemoglobin with oxyhemoglobin. J Biol Chem 265(32):19453–19460
Grune T (2000) Oxidative stress, aging and the proteasomal system. Biogerontology 1(1):31–40. https://doi.org/10.1023/a:1010037908060
Zhang AS, Enns CA (2009) Molecular mechanisms of normal iron homeostasis. Hematol Am Soc Hematol Educ Program. https://doi.org/10.1182/asheducation-2009.1.207
Carley A (2003) Anemia: when is it not iron deficiency? Pediatr Nurs 29(3):205–211
Ghosal S, Chattaraj W, Pramanik D, Mukherjee S, Banerjee U (2018) Assessment of peripheral neuronal activity with nerve conduction studies in iron deficiency anaemia patients from rural areas of Bankura District of West Bengal. JMSCR 6(9):1051–1054. https://doi.org/10.18535/jmscr/v6i9.182
Vulser H, Wiernik E, Hoertel N, Thomas F, Pannier B, Czernichow S et al (2016) Association between depression and anemia in otherwise healthy adults. Acta Psychiatr Scand 134(2):150–160. https://doi.org/10.1111/acps.12595
Hübner NS, Mechling AE, Lee HL, Reisert M, Bienert T, Hennig J et al (2017) The connectomics of brain demyelination: functional and structural patterns in the cuprizone mouse model. Neuroimage 146:1–18. https://doi.org/10.1016/j.neuroimage.2016.11.008
Bastian TW, Santarriaga S, Nguyen TA, Prohaska JR, Georgieff MK, Anderson GW (2015) Fetal and neonatal iron deficiency but not copper deficiency increases vascular complexity in the developing rat brain. Nutr Neurosci 18(8):365–375. https://doi.org/10.1179/1476830515y.0000000037
Yang W, Liu B, Gao R, Snetselaar LG, Strathearn L, Bao W (2021) Association of anemia with neurodevelopmental disorders in a nationally representative sample of US children. J Pediatr 228:183-189.e182. https://doi.org/10.1016/j.jpeds.2020.09.039
Walter T, De Andraca I, Chadud P, Perales CG (1989) Iron deficiency anemia: adverse effects on infant psychomotor development. Pediatrics 84(1):7–17
Guo Y, Yu L, Wu ZY, Deng YH, Wu JL (2023) Gender-specific association between serum ferritin and neurodevelopment in infants aged 6 to 12 months. Sci Rep 13(1):2490. https://doi.org/10.1038/s41598-023-29690-x
Deveci D, Marshall JM, Egginton S (2001) Relationship between capillary angiogenesis, fiber type, and fiber size in chronic systemic hypoxia. Am J Physiol Heart Circ Physiol 281(1):H241-252. https://doi.org/10.1152/ajpheart.2001.281.1.H241
Hepple RT (2000) Skeletal muscle: microcirculatory adaptation to metabolic demand. Med Sci Sports Exerc 32(1):117–123. https://doi.org/10.1097/00005768-200001000-00018
Smith DL (2000) Anemia in the elderly. Am Fam Physician 62(7):1565–1572
Penninx BW, Pahor M, Cesari M, Corsi AM, Woodman RC, Bandinelli S et al (2004) Anemia is associated with disability and decreased physical performance and muscle strength in the elderly. J Am Geriatr Soc 52(5):719–724. https://doi.org/10.1111/j.1532-5415.2004.52208.x
Alley DE, Shardell MD, Peters KW, McLean RR, Dam TT, Kenny AM et al (2014) Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol A Biol Sci Med Sci 69(5):559–566. https://doi.org/10.1093/gerona/glu011
Hirani V, Naganathan V, Blyth F, Le Couteur DG, Seibel MJ, Waite LM et al (2016) Low hemoglobin concentrations are associated with Sarcopenia, physical performance, and disability in older Australian men in cross-sectional and longitudinal analysis: the concord health and ageing in men project. J Gerontol Ser A 71(12):1667–1675. https://doi.org/10.1093/gerona/glw055
Gi YM, Jung B, Kim KW, Cho JH, Ha IH (2020) Low handgrip strength is closely associated with anemia among adults: a cross-sectional study using Korea National Health and Nutrition Examination Survey (KNHANES). PLoS ONE 15(3):e0218058. https://doi.org/10.1371/journal.pone.0218058
Acknowledgements
The authors want to convey their profound appreciation to the children and their parents for participating.
Funding
This research did not receive any specific grant from the public, commercial, or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
Fatma Essam Amer, Khaled Ahmed Mamdoh, Tamer Hasan Moustafa Hassan Walaa A. Abd-El-Nabie, and Hoda Eltalawy designed the research; Fatma Essam Amer, Khaled Ahmed Mamdoh, Tamer Hasan Moustafa Hassan Walaa A. Abd-El-Nabie, and Hoda Eltalawy performed all experiments; Fatma Essam Amer, Khaled Ahmed Mamdoh, Walaa A. Abd-El-Nabie, and Hoda Eltalawy analyzed the data; Fatma Essam Amer, Khaled Ahmed Mamdoh, Tamer Hasan Moustafa Hassan Walaa A. Abd-El-Nabie, and Hoda Eltalawy wrote and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethical Committee of the Faculty of Physical Therapy at Cairo University approved the study protocol (No: P.T.REC/012/003712). In addition, participation in the current study was authorized by asking the children's parents to sign a consent form before data collection.
Consent of publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amer, F.E., Mamdouh, K.A., Hassan, T.H.M. et al. Iron deficiency anemia in relation to pinch strength and hand dexterity in preschool children: a cross-sectional study. Beni-Suef Univ J Basic Appl Sci 13, 59 (2024). https://doi.org/10.1186/s43088-024-00518-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-024-00518-5