Abstract
Background and Objective
Genetic and epigenetic changes characterize the multi-step process of breast carcinogenesis. It is believed that abnormal microRNA (miRNA) expression has a role in the onset and progression of breast cancer. This study aimed to examine the link between miRNA-127 and miRNA-138 and metastasis, tumor invasion, and apoptosis in Egyptian women with breast cancer, as well as their correlation with its molecular types.
Methodology
A total of 150 participants were included in this study, including 75 women with breast cancer and 75 supposedly healthy women who were age and gender-matched. Every patient underwent a thorough physical examination, a general clinical examination, a mammogram, and lab tests, such as the determination of the levels of miRNA-127 and miRNA-138 expression by real-time PCR and the measurement of blood carcinoembryonic antigen (CEA) and carcinoma antigen 15–3 (CA15-3) and CA15-3 and CEA levels.
Results
There was a significant low expression of miRNA-127 in favor of high TNM stage (Classification of Malignant Tumors), left-sided tumor, metastasis, high-grade disease, increased axillary nodal involvement, absence of estrogen and progesterone receptors, and low antigen Kiel 67 (Ki67) expression. Also, a significant expression of miRNA 127 in triple-negative breast cancer was found, followed by human epidermal growth factor receptor 2 (HER2/neu) overexpression, then luminal B, and the highest expression was with the Luminal A molecular subtype. A significant negative correlation existed between miRNA 127 and miRNA 138 with CEA and CA15.3 levels.
Conclusion
The miRNA-127 and miRNA-138 suppression may promote metastasis. Consequently, the restoration of miRNA-127 and miRNA-138 in breast cancer may have therapeutic potential; so, the miRNA-127 and miRNA-138 may play a role in breast cancer development.
Similar content being viewed by others
1 Background
Breast cancer (BC), known as the "pink killer", is the most common female malignant tumor [18]. BC is the main reason for female cancer mortality in 110 countries and is responsible for 15.5% of all cancer-related fatalities—approximately 7.7 million women survive five years following diagnosis with BC [17]. There were 22,700 new cases in Egypt and 9148 BC-related deaths in 2020 [1],. Human epidermal receptor 2 expressions (HER2/neu +), triple-negative BC (TNBC) (ER − , PR − , HER2/neu −), and estrogen receptor (ER +) or progesterone receptor (PR +) are the three distinct subtypes (hormone receptor expression) of BC, each with unique molecular traits and genetic profiles [6]. It will be helpful to clarify the molecular pathways involved in BC development by taking advantage of possible molecular, diagnostic, and prognostic indicators [19].
MicroRNAs (miRNAs) are a class of small endogenous noncoding RNAs that regulate the expression of protein-coding genes at the level of transcription and exert biological functions by degrading or inhibiting mRNA expression [8, 26]. It was recently found that miRNAs and human BCs are related. Recent clinical studies have started to assess miRNA expression profiling of tumors as a possible prognostic tool since it is believed that abnormal miRNA expression contributes to the onset and progression of breast cancer [2, 9].
It has been demonstrated that miRNA-127 functions as a tumor suppressor in a range of human malignancies, including BC [23]. According to Pronina et al. [13], hypermethylation of the miR-127 promoter region in BC tissues is a sign of tumor metastasis and is highly linked to metastasis. In BC tissues, miRNA-127 was significantly downregulated. Clinical stages, reduced overall survival (OS), and lymph node metastases are all linked to low expression levels of miRNA-127 and are independent predictors of the prognosis of breast cancer [16, 30].
Recently, miRNA-138 was found to regulate tumors; its involvement in promoting or inhibiting cancer has been shown in a range of tumor tissues [27]. In tissues and cells affected by breast cancer, miRNA-138-5p is not highly expressed. By upregulating the expression of E-cadherin and downregulating that of N-cadherin and vimentin, overexpression of miRNA-138-5p targets rhomboid domain-containing protein one and dramatically suppresses the invasion, migration, and epithelial-mesenchymal transition (EMT) of breast cancer cells [29]. MiRNA-138 functions as a new regulator in breast cancer cells, regulating tumor invasion and EMT by targeting histone methylation transferase and regulating proliferation and migration of breast cancer cells by targeting cycle-dependent kinase inhibitor-related protein [5]. Thus, the signal triggered by miRNA-138 may function as a new independent prognostic marker [12].
This study's primary focus will be the significance of miRNA-138 and miRNA-127 as a non-invasive diagnosis for breast cancer. It provides a tool for early detection, which enhances patient outcomes and allows for an in-depth understanding of the molecular mechanisms causing breast cancer, treatment responsiveness, and its effect on survival.
2 Subjects and methods
2.1 Study design and population
The Clinical Oncology and Nuclear Medicine Department, Faculty of Medicine, Menoufia University, collaborated with the Medical Biochemistry and Molecular Biology Department to conduct this case–control study. One hundred and fifty participants were involved in the trial, including 75 breast cancer patients and 75 volunteers who appeared to be healthy. All patients provided written, voluntarily informed consent. All facets of this investigation were authorized by the ethics committee of Menuofia University's College of Medicine.
Patients who had received radiation or chemotherapy before surgery or who had a history of primary malignancies other than breast cancer were not eligible for the trial. All participants' personal histories, including the patient's age, menopausal state, and breast cancer in the family history, were collected. Clinicopathological information included tumor sidedness, histological type, tumor grade, TNM staging, tumor immunohistochemistry, including ER and PR status, HER2/neu expression, Ki67 expression, and various molecular subtypes (TNBC, HER2/neu overexpression, luminal A and luminal B). Measurements of blood tumor markers, carcinoembryonic antigen (CEA), and cancer antigen 15.3 (CA15.3) were performed in laboratories—findings from a molecular analysis to measure miRNA-127 and miRNA-138 levels.
Data on treatments included Metastatic status, the kind of surgery, the type of treatment chemotherapy or biological and hormone therapy received, the occurrence of treatment toxicity, and the severity of the toxicity. Progression and living status were recorded to calculate progression-free survival (PFS) and overall survival (OS).
3 Sampling and laboratory investigations
Each participant had two sterile vacationer tubes used to draw five milliliters of venous blood from them. Two milliliters were collected for RNA extraction in the first tube, which contained ethylene diamine-tetra acetic acid (EDTA), and the second tube, which lacked an anticoagulant. The samples were allowed to clot in the first tube before being centrifuged, and the serum was separated using the chemiluminescence method (ECLIA) to evaluate the levels of CA15.3 and CEA.
4 Extraction and reverse transcription (RT) of RNA
Following the manufacturer's instructions, total RNA, including miRNAs, was extracted using the RNeasy Mini Kit and Qiazol Reagent (Qiagen, USA). The NanoDrop 1000 (Thermo Scientific, USA) was utilized to evaluate the RNA's quality. Using the miScript II RT Kit (Qiagen, USA), single-stranded cDNA was created from the extracted materials as directed by the manufacturer. The cDNA product was kept at -20 °C until the real-time PCR stage.
5 Quantitative real-time PCR
Real-time PCR was performed on 100 nanograms of total RNA using the StepOne Real-Time PCR system (Applied Biosystems) and the miScript Primer Assay (forward primer) for miRNA16 (reference miRNA), miRNA-138, and miRNA-127, as well as the miScript SYBR Green PCR Kit, which contained the QuantiTect SYBR Green PCR Master Mix, following the manufacturer's instructions. The following real-time PCR protocol was used: 40 cycles of 94 °C for 15 s, 55 °C for 30 s, and 70 °C for 30 s were performed after 15 min at 95 °C. Inter-assay controls verified endogenous controls, and samples were all utilized. By using the 2−ΔΔCt method (ΔΔCt = {[Ct (miRNA of interest) – Ct (reference miRNA-16 of interest)] − [Ct (miRNA of control) – Ct (reference miRNA-16 of control)]}, the relative quantification (RQ) of miRNA gene expression was evaluated [20].
6 Statistical analysis
The computer-supplied data were analyzed using the IBM SPSS software program, version 20.0. (IBM Corp., New York's Armonk). To describe quantitative data, percentages, and numbers were used. The Kolmogorov–SmiRNAnov test was used to determine if the distribution was normally distributed. Quantitative data were represented using the interquartile range (IQR), mean, standard deviation, and range (minimum and maximum). The statistical significance of the data was calculated at the 5% level. The Kaplan–Meier curve, Fisher's Exact or Monte Carlo correction, Student's t-test, Mann–Whitney test, and Chi-square test were used for the survival research.
7 Results
7.1 Demographic and clinicopathological characteristics of study subjects
With 150 participants overall, the median age was 51, and the mean age ± SD was 49.16 ± 10.17. Participants' ages ranged from 27 to 73 years. Two groups of cases (≤ 51 and > 51) were created based on the median age of the cases. At the time of diagnosis, 31 (41.3%) and 44 (58.7%) patients, respectively, were postmenopausal and premenopausal, respectively. Only five (6.7%) of the total cases under investigation had a positive family history of breast cancer. The tested groups' ages, menstrual status, and family history showed no discernible differences.
The breast cancer group's clinical characteristics are shown in Table 1. Patients with positive hormone receptor status showed positive ER levels of 58.7% and positive PR values of 56%. HER2/neu levels were high (60%) in some patients, low (21%) in others, and absent (18.7%) in others. Compared to Luminal A (17.3% of patients), the molecular subtypes showed that Luminal B biological type was discovered more frequently (41.3%). Before the trial's conclusion, 10.3% of the cases passed away, and 25 cases (33.3%) reported disease progression.
8 Tumor markers, miRNA-138 and miRNA-127
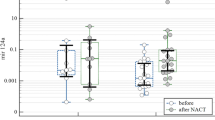
Tumor marker results for CEA were statistically different between the case (12.69 ± 27.52) and control (2.20 ± 1.04) groups (P = < 0.001). As well as CA15.3 which was statistically different between the case (45.33 ± 59.56) and control (15.95 ± 5.74) groups (P = 0.002). Additionally, the case group had significantly lower expression of miRNA-138 and miRNA-127 (11.18 ± 5.75, 11.04 ± 6.67, respectively) than the control group (14.85 ± 2.72, 14.59 ± 2.77, respectively) (P = 0.001) (Fig. 1).
miRNA-138 was significantly lower in triple-negative BC (10.11 ± 7.36) and other types of luminal classifications (11.71 ± 4.76) compared to the control group (14.85 ± 2.72). The P value for comparing TNBC and control was (p2 = 0.002) and the P value for comparing between other types and control was (p3 < 0.001), but the difference between TNBC cases and other types of cases was not statistically significant (p1 = 0.626). miRNA-127 was significantly lower in TNBC (8.19 ± 6.51) and other luminal categories (12.46 ± 6.34) compared to the control group (14.59 ± 2.77). The P value for comparing triple-negative cases and other types of cases was (p1 = 0.015), the P value comparing triple-negative and control was (p2 < 0.001), and the P value for comparing between other and control was (p3 = 0.020) (Fig. 2).
Comparing the two cases groups and control regarding the level of A: miRNA-138 (p1 = 0.626), (p2 = 0.002), ( p3 < 0.001); B: miRNA-127 (p1 = 0.015), (p2 < 0.001), (p3 = 0.020). p: p-value for comparison between the studied categories *: Statistically significant at p ≤ 0.05 p1: p-value for comparing between TNBC and other cases p2: p-value for comparing between TNBC and control p3: p-value for comparing between other cases and control
According to the analysis of the relationships between these biomarkers, miRNA-127 had a statistically significant positive correlation with miRNA-138 (r = 0.251, P = 0.030). CEA value had a moderately significant negative correlation with miRNA-138 (r = − 0.304, P = 0.008) and miRNA-127 (r = − 0.348, P = 0.002). CA15.3.value had a mild significant negative correlation with miRNA-138 (r = − 0.240, P = 0.038) and miRNA-127 (r = − 0.283, P = 0.014) and a moderately significant positive correlation with CEA value (r = 0.369, P = 0.001).
8.1 Correlation between the miRNA-138 and miRNA-127 expression with clinicopathological data and treatment
There was a significant step-wise decrease in the expression miRNA-138 with increasing the TNM stage (P = 0.001). Also, a high expression of miRNA-138 favored non-metastatic, low-grade (GI & GII) diseases (P = 0.006 & P = 0.019, respectively). A significantly higher expression of the miRNA-138 was found in still-alive cases than in dead cases (P = 0.002). On the other hand, there was a significant step-wise increase in the expression of miRNA-127 in left-side tumor cases compared to the right side (P = 0.009) and a significant decrease in metastasis cases (P = 0.018). miRNA-127 was decrease significantly in grade 2 toxicity (P = 0.012), in progressed cases (P = 0.002) and was increase significantly in hormonal treatment (P = < 0.001*) and alive cases (P = 0.004*) in cases group (Table 2).
9 Survival data of the cases
At the end of the study, the progression-free survival rate for the patients under study was 66.4%. The mean progression-free survival time was 25.392 months. The overall survival time of the studied cases at the end of the study was 86.6%. The mean survival time was 30.117 months. The overall survival was significantly longer in patients with high miRNA-138 (≥ 12.18) expression (mean = 26.987 months, overall survival time = 78.9%) compared to patients with low expression (< 12.18) (mean = 31.703, overall survival time = 94.6%) (P = 0.049), with no significant correlation with PFS (Fig. 3).
Kaplan–Meier survival curve for overall Survival with miR-138 and miR-127. a A total of 75 Breast cancer patients were segregated into two groups (above median: n = 45, below median: n = 30) based on the expression status of miR-138. The overall survival time at the end of the study was significantly longer in patients with below median (< 12.18) miRNA 138 levels (mean = 26.987, 78.9%) compared to patients with above median (> 12.18) miRNA 138 levels (mean = 31.703, 94.6%) (P = 0.049). b) A total of 75 Breast cancer patients were segregated into two groups (above median: n = 46, below median: n = 29) based on the expression status of miR-127. The overall survival time at the end of the study was significantly longer in patients with below median (< 11.31) miRNA 127 levels (mean = 23.832, 78.9%) compared to patients with above median (> 11.31) miRNA 127 levels (mean = 31.703, 94.6%) (P = 0.049)
Regarding survival correlation with miRNA-127 expression, PFS and OS were significantly shorter in patients with low miRNA 127 expression (< 11.31) (mean = 18.855 months, progression-free survival time = 51.9%) and (mean = 23.832 months, overall survival time = 78.9%) respectively, compared to patients with high miRNA 127 (≥ 11.31) expression (mean = 28.865 months, progression-free survival time = 81.1%) (mean = 31.703 months, overall survival time = 94.6%) (P = 0.007, P = 0.049 respectively) (Fig. 4).
Kaplan–Meier survival curve for progression-free survival with miR-138 and miR-127. a A total of 75 Breast cancer patients were segregated into two groups (above median: n = 45, below median: n = 30) based on the expression status of miR-138. The progression-free survival time at the end of the study was insignificantly different between patients with below median (< 12.18) miRNA 138 levels (mean = 23.271, 62.9%) and patients with above median (> 12.18) miRNA 138 levels (mean = 26.284, 70.2%) (P = 0.504). b A total of 75 Breast cancer patients were segregated into two groups (above median: n = 46, below median: n = 29) based on the expression status of miR-127. The progression-free survival time at the end of the study was significantly shorter in patients with below median (< 11.31) miRNA 127 levels (mean = 18.855, 51.9%) compared to patients with above median (> 11.31) miRNA 127 levels (mean = 28.865, 81.1%) (P = 0.007)
9.1 The relationship between breast cancer patients' clinicopathological traits and mortality
In univariate COX regression analysis, metastasis status, CA15.3.value, chemo toxicity, miRNA- 138, and miRNA-127 were significantly associated for mortality as dependent variables with each other but in multivariate COX regression analysis, they were not predictors as individual independent variables. Table 3.
10 The relationship between clinicopathological characteristics and relapse
In univariate COX regression analysis, metastasis status, PT status (≥ 3), PN status (≥ 3), CEA value, CA15.3.value, miRNA-138 and miRNA-127 were significantly associated with relapse as dependent variable. In multivariate COX regression analysis, CEA value and CA15.3.value significantly acted as independent predictor variables Table 4.
11 Discussion
In the last few years, microRNAs (miRNAs) have attracted considerable attention in breast cancer research, due to their conflicting functions either as potential oncogenes or tumor suppressor genes, this is in addition to their prognostic role. The objective of the present study was to evaluate the potential of miRNA-127 and miRNA-138 expression levels as a biomarker that might be combined with additional tools for diagnosis and prognosis [23].
In the present study, there was a significantly low expression of miRNA-127 in primary tumors in breast cancer compared to the control group. Similar to our result, those reported by [11] and [24], found that seven miRNAs including miRNA-127 were downregulated more than twofold in BC tissues than in adjacent normal tissues. Also, our findings were analogous to those of Umeh-Garcia et al. [21], who examined miRNA-seq data from the BRCA dataset and found that miRNA-127 expression was lower in breast tumors than in healthy tissue. Furthermore, Chan et al., 2013, identified miRNA-127 as a regulator of cellular senescence that directly targeted the proto-oncogene BCL6. They showed that miRNA-127 downregulation in breast cancer tissue was associated with up-regulation of BCL6 so over-expression of miRNA-127 or depletion of BCL6 inhibited breast cancer cell proliferation [4].
In this study, miRNA-127 was considerably lower in high-grade tumors (GIII), patients with more than 3 lymph node metastases (N2, N3), patients with metastatic disease, patients that progressed, and patients that died. This was in agreement with [13] and [21], who reported that poorly differentiated and advanced-stage tumors were more likely to have hypermethylated miRNA-127 promoters than other cancer patients. Furthermore, it was attributed to the depletion of miRNA-127 that could reduce its tumor suppressor effect and enhance the capacity of migration and invasion in BC cells as reported by [23]
In addition, we found significantly high miRNA-127 expression in tumors with ER and PR expression. This confirmed the observation by Alizadeh et al. [3], who found that hormone therapy might significantly upregulate tumor suppressor miRNAs including miRNA-127 in women with breast cancer. This study also observed a statistically significant higher level of miRNA-127 after hormonal treatment. Significant high miRNA-127 level in tumors with low expression of the proliferation marker Ki 67, which was explained by [7] who reported that ectopic expression of miRNA-127 in gastric cancer cell lines inhibited cell proliferation and suppressed the cell cycle. Also, we found significantly low expression of miR-127 in the most aggressive pathological subtypes of BC, TNBC, and HER2/neu overexpression similar to [21].
In correlation with miRNA-127 expression, median PFS and OS were significantly higher in patients with high miRNA-127 expression. This is in line with our findings by Wang et al. [23] who showed that patients with low miRNA127 had OS that was considerably lower than individuals with high miRNA-127, which explained that upregulation of miRNA-127 could inhibit growth and reduce the capacity of colony formation and cellular migration and invasion in BC cells by enhancing caspase-3-dependent apoptosis that might decrease the incidence of local recurrence and distant metastasis, and so improved patient survival.
In this study, the level of miRNA-138 with low expression (13.48) was significantly associated with breast cancer patients, which was explained by [10] who reported that high expression of miRNA-138-5p might reduce breast cancer cell proliferation via targeting LIM domain kinase 1 (LIMK1). Additionally, lower miRNA-138 expression levels were found in triple-negative cases and other pathological subtypes. This finding follows Wang et al. [22] and Yao et al. [25], who noticed the downregulation of miRNA-138 in the aggressive pathological subtype, TNBC patients. Contrary to our results, those reported by [12], and [14] found that miRNA-138 was an oncogenic driver in TNBC, however the difference in our results was statistically non-significant. In this study, miRNA-138 was significantly decreased in metastatic cases (P = 0.006) and significantly increased in early-stage patients compared to late cases (P = 0.019). The same finding was observed by Zhang et al. [28], who found that low levels of miRNA-138 were linked to lymph node metastases and invasion and this could be due to the role of miRNA-138 in enhancing the cell motility, and arrest in the G0/G1 phase [10].
In this study, miRNA-138 and miRNA-127 revealed a moderately significant negative correlation with the elevated level of the predictive biomarkers of breast cancer, CEA, and CA15.3 values which was the role of both miRNA-138 and miRNA-127 in inhibiting cell proliferation, invasion, metastasis and inducing apoptosis [15] & [23].
In the present study, the OS was significantly longer in patients with high miRNA-138 expression. Many studies indicated that miRNA-138 may be a tumor suppressor in many types of cancers [27], Chemn et al., 2022).
12 Conclusion
The results of the current study supported the use of miRNA-138 and miRNA-127 as essential and distinctive biomarkers for the diagnosis of breast cancer, as well as their potential use in prognosis and treatment. However, more thorough functional analyses and prospective population-based research with large sample sizes and a range of ethnic groups are required to support these findings.
Availability of data and materials
Not Applicable.
Abbreviations
- BC:
-
Breast cancer
- HER2/neu + :
-
Human epidermal receptor 2 expressions
- TNBC:
-
Triple-negative BC (ER − , PR − , HER2/neu −)
- ER + :
-
Estrogen receptor
- PR + :
-
Progesterone receptor
- miRNAs:
-
MicroRNAs
- OS:
-
Overall survival
- EMT:
-
Epithelial-mesenchymal transition
- CEA:
-
Carcinoembryonic antigen
- CA15.3:
-
Cancer antigen 15.3
- PFS:
-
Progression-free survival
- EDTA:
-
Ethylene diamine-tetra acetic acid
- RQ:
-
Relative quantification
- IQR:
-
Interquartile range
- GI & GII:
-
Low-grade
- GIII:
-
High-grade tumors
- LIMK1:
-
LIM domain, kinase 1
References
Abdel-Fadeel N, Zanaty M, Kamal A, Hassan M, Taha M (2022) Childhood psychological trauma and psychiatric comorbidity in patients with breast cancer. Egypt J Hosp Med 88(1):2788–2794. https://doi.org/10.21608/ejhm.2022.241954
Almohaywi M, Sugita BM, Centa A, Fonseca AS, Antunes VC, Fadda P, Mannion CM, Abijo T, Goldberg SL, Campbell MC, Copeland RL, Kanaan Y, Cavalli LR (2023) Deregulated miRNA expression in triple-negative breast cancer of ancestral genomic-characterized latina patients. Int J Mol Sci 24(17):13046. https://doi.org/10.3390/ijms241713046
Alizadeh S, Isanejad A, Sadighi S, Khalighfard S, Alizadeh AM (2019) Effect of a high-intensity interval training on serum microRNA levels in women with breast cancer undergoing hormone therapy A single-blind randomized trial. Annals Phys Rehabilit Med 62(5):329–335. https://doi.org/10.1016/j.rehab.2019.07.001
Chen J, Wang M, Guo M, Xie Y, Cong YS (2013) miR-127 regulates cell proliferation and senescence by targeting BCL6. PLoS ONE 8(11):e80266
Cheng H, Chen L, Fang Z, Wan Q, Du Z, Ma N, Guo G, Lu W (2022) The effect of miRNA-138 on the proliferation and apoptosis of breast cancer cells through the NF-κB/VEGF signaling pathway. Cellular Mole Biol Noisy-le-Grand, France 68(2):132–137. https://doi.org/10.14715/cmb/2022.68.2.19
El Hejjioui B, Lamrabet S, Amrani Joutei S, Senhaji N, Bouhafa T, Malhouf MA, Bennis S, Bouguenouch L (2023) New biomarkers and treatment advances in triple-negative breast cancer. Diagnostics (Basel, Switzerland) 13(11):1949. https://doi.org/10.3390/diagnostics13111949
Guo LH, Li H, Wang F, Yu J, He JS (2013) The tumor suppressor roles of miR-433 and miR-127 in gastric cancer. Int J Mol Sci 14(7):14171–14184
Han J, Mendell JT (2023) MicroRNA turnover: a tale of tailing, trimming, and targets. Trends Biochem Sci 48(1):26–39. https://doi.org/10.1016/j.tibs.2022.06.005
Khadka VS, Nasu M, Deng Y, Jijiwa M (2023) Circulating microRNA biomarkers for detecting breast cancer in high-risk benign breast tumors. Int J Mol Sci 24(8):7553. https://doi.org/10.3390/ijms24087553
Li D, Song H, Wu T et al (2017) MiRNA-138-5p targeting LIMK1 suppresses breast cancer cell proliferation and motility. Rsc Adv 7(82):52030–52038
Lu M, Ju S, Shen X, Wang X, Jing R, Yang C, Chu H, Cong H (2017) Combined detection of plasma miRNA-127-3p and HE4 improves the diagnostic efficacy of breast cancer. Cancer Biomark 18(2):143–148. https://doi.org/10.3233/CBM-160024
Nama S, Muhuri M, Di Pascale F, Quah S, Aswad L, Fullwood M, Sampath P (2019) MicroRNA-138 is a prognostic biomarker for triple-negative breast cancer and promotes tumorigenesis via TUSC2 repression. Sci Rep 9(1):12718. https://doi.org/10.1038/s41598-019-49155-4
Pronina IV, Loginov VI, Burdennyy AM, Fridman MV, Senchenko VN, Kazubskaya TP, Kushlinskii NE, Dmitriev AA, Braga EA (2017) DNA methylation contributes to the deregulation of 12 cancer-associated microRNAs and breast cancer progression. Gene 604:1–8. https://doi.org/10.1016/j.gene.2016.12.018
Qattan A (2020) Novel miRNA targets and therapies in the triple-negative breast cancer microenvironment: an emerging hope for a challenging disease. Int J Mol Sci 21(23):8905. https://doi.org/10.3390/ijms21238905
Sha HH, Wang DD, Chen D, Liu SW, Wang Z, Yan DL, Feng JF (2017) MiR-138: A promising therapeutic target for cancer. Tumor Biol 39(4):1010428317697575
Shang C, Chen Q, Zu F, Ren W (2022) Integrated analysis identified prognostic microRNAs in breast cancer. BMC Cancer 22(1):1170. https://doi.org/10.1186/s12885-022-10242-x
Shinde SS, Ahmed S, Malik JA, Hani U, Khanam A, Ashraf Bhat F, Ahmad MiRNA S, Ghazwani M, Wahab S, Haider N, Almehizia AA (2023) Therapeutic delivery of tumor suppressor miRNAs for breast cancer treatment. Biology 12(3):467. https://doi.org/10.3390/biology12030467
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics. CA: A Cancer J Clin 71(1):7–33. https://doi.org/10.3322/caac.21654
Teh BT, Fearon ER (2020) Genetic and epigenetic alterations in cancer. Abeloff’s Clin Oncol 209–224:e2. https://doi.org/10.1016/b978-0-323-47674-4.00014-1
Thu HN, Vy HT, Thanh TN, Giang DT, Nhan TN, Hoang NP, Hue TN (2021) miRNA-16 as an internal control in breast cancer studies: a systematic review and meta-analysis. Mol Biol 55(6):1045–1056. https://doi.org/10.31857/S0026898421060136
Umeh-Garcia M, Simion C, Ho PY, Batra N, Berg AL, Carraway KL, Yu A, Sweeney C (2020) A Novel Bioengineered miRNA-127 Prodrug Suppresses the Growth and Metastatic Potential of Triple-Negative Breast Cancer Cells. Can Res 80(3):418–429. https://doi.org/10.1158/0008-5472.CAN-19-0656
Wang G, Dong Y, Liu H, Ji N, Cao J, Liu A, Tang X, Ren Y (2022) Long noncoding RNA (lncRNA) metallothionein 1 J, pseudogene (MT1JP) is downregulated in triple-negative breast cancer and upregulates microRNA-138 (miRNA-138) to downregulate hypoxia-inducible factor-1α (HIF-1α). Bioengineered 13(5):13718–13727. https://doi.org/10.1080/21655979.2022.2077906
Wang S, Li H, Wang J, Wang D, Yao A, Li Q (2014) Prognostic and biological significance of microRNA-127 expression in human breast cancer. Dis Markers 2014:401986. https://doi.org/10.1155/2014/401986
Yan LX, Huang XF, Shao Q, Huang MY, Deng L, Wu QL, Shao JY (2008) MicroRNA miR-21 overexpression in human breast cancer is associated with advanced clinical stage, lymph node metastasis, and patient poor prognosis. RNA 14(11):2348–2360
Yao L, Chen L, Zhou H, Duan F, Wang L, Zhang Y (2022) Long noncoding RNA NEAT1 promotes the progression of breast cancer by regulating miRNA-138-5p/ZFX axis. Cancer Biother Radiopharm 37(8):636–649. https://doi.org/10.1089/cbr.2019.3515
Yedigaryan L, Sampaolesi M (2021) Therapeutic implications of miRNAs for muscle-wasting conditions. Cells 10(11):3035. https://doi.org/10.3390/cells10113035
Yeh M, Oh CS, Yoo JY, Kaur B, Lee TJ (2019) Pivotal role of microRNA-138 in human cancers. Am J Cancer Res 9(6):1118–1126
Zhang J, Liu D, Feng Z, Mao J, Zhang C, Lu Y, Li J, Zhang Q, Li Q, Li L (2016) MicroRNA-138 modulates metastasis and EMT in breast cancer cells by targeting vimentin. Biomed Pharmacother Biomed Pharmacother 77:135–141. https://doi.org/10.1016/j.biopha.2015.12.018
Zhao C, Ling X, Li X, Hou X, Da Z (2019) MicroRNA-138-5p inhibits cell migration, invasion, and EMT in breast cancer by directly targeting RHBDD1. Breast Cancer 26(6):817–825. https://doi.org/10.1007/s12282-019-00989-w
Zhao X, Duan Z, Liu X, Wang B, Wang X, He J, Yao Z, Yang J (2013) MicroRNA-127 is downregulated by Tudor-SN protein and contributes to metastasis and proliferation in breast cancer cell line MDA-MB-231. Anat Rec (Hoboken) 296(12):1842–1849
Acknowledgements
Not Applicable
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
GMN, MFE, and EAG got the study concept and design, EAE and RAA do the clinical examination and diagnosis, AAA and HSA made data analysis and interpretation, and GMN, EAG, and AAA wrote and revised the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval and consent to participate
Research Involving Human Participants. The study was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent, and the Ethics Committee of Faculty of Medicine, Menoufia University approved the study protocol.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no conflict of interest that affects this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nasr, G.M., Elshal, M.F., Gobran, E.AG. et al. Clinical and biological significance of microRNA-127 and microRNA-138 expression in women with breast cancer: response to treatment and survival impact. Beni-Suef Univ J Basic Appl Sci 13, 24 (2024). https://doi.org/10.1186/s43088-024-00476-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-024-00476-y