Abstract
Background
Early prediction of non-invasive ventilation failure by using clinical parameters and scoring systems is a promising strategy for reducing mortality in acute exacerbation of chronic obstructive pulmonary disease patients. Our aim was to assess predictors of non-invasive ventilation failure in acute exacerbation of chronic obstructive pulmonary disease and the prognostic role of mid-regional proadrenomedullin.
Results
Forty-five patients were enrolled, comprising thirty-six males and nine females with mean age 63.4 ± 9.22 years. Mid-regional proadrenomedullin could not predict non-invasive ventilation outcome, while acute physiology and chronic health evaluation score, blood pH, arterial carbon dioxide and platelet count had predictive value.
Conclusion
Prediction of non-invasive ventilation outcome in acute exacerbation of chronic obstructive pulmonary disease patients is multifactorial and mid-regional proadrenomedullin alone could not predict this outcome.
Similar content being viewed by others
1 Background
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death worldwide. Acute exacerbation of COPD (AECOPD), especially when leading to hospitalization, plays a major role in increasing disease severity, mortality, and raising the economic burden of COPD [1]. Non-invasive ventilation (NIV), the gold standard treatment for AECOPD with acute hypercapnic respiratory failure, has been used in clinical practice since the end of the last century. It reduced the need for intubation, costs and length of hospital stay, and increased survival in these patients [2]. Precise identification of patients who will not benefit from NIV would avoid the unnecessary discomfort of NIV and the dangerous delay of intubation [3].
COPD is associated with systemic inflammation, and several circulating biomarkers are increased during exacerbation, reflecting the spillover of local airway inflammation into the circulation [4]. Adrenomedullin (ADM) is a 52-amino acids peptide that possess a variety of biological actions as immune-modulating, metabolic, vasodilatory and bactericidal actions [5]. The mid-regional fragment of this peptide “Proadrenomedullin” (MR-proADM), is more stable than the active molecule itself, allowing its indirect quantification [6].
Plasma ADM is elevated in various diseases as arterial hypertension, myocardial infarction, heart failure and septic shock [7]. In addition, tissue hypoxia was found to be a powerful physiological stimulus for ADM synthesis [6]. Several studies had explored the role of MR-proADM in COPD exacerbation as a diagnostic biomarker and its ability to predict mortality in patients requiring NIV with conflicting results [4,5,6]. The aim of this study was to evaluate predictors of NIV failure and to assess the ability of MR-proADM to predict NIV outcome in AECOPD patients.
2 Methods
2.1 Study design
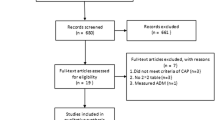
This prospective observational study was conducted in the period between December 2019 and August 2021. The study has been approved by the research ethics committee of our institute (No: MD-201-2019) and was conducted in accordance with the Helsinki Declaration. Written informed consent was obtained from all patients.
Inclusion criteria: COPD patients (previously diagnosed in our institute according to global initiative for chronic obstructive lung diseases “GOLD” criteria) with acute hypercapnic respiratory failure due to acute exacerbation. The following were excluded: patients with pneumonia, congestive heart failure and sepsis.
2.2 Sample size calculation
The calculated sample size is 45 AECOPD patients with acute hypercapnic respiratory failure. This sample size will be large enough to detect a 79% specificity of the MR-proADM for predicting the occurrence NIV failure in AECOPD patients with acute hypercapnic respiratory failure [4], at 95% level of confidence and 80% power of the study. Calculation was performed using the following sample size equation that has been described in Buderer [8], and is based on an estimated specificity of 79%, an estimated prevalence of NIV failure 24% [4], and a margin of error of 14%.
where n = calculated sample size, Zα/2 = the critical value of the Z distribution corresponding to the 95% level of confidence (= 1.96), p = estimated prevalence of NIV failure (24%), Sp = estimated specificity of MR-proADM for predicting the occurrence NIV failure in AECOPD patients “the primary end point” (0.79%), E = margin of error (as of 14%).
2.3 Data collection
Medical history was taken including comorbidities and the need for long term oxygen therapy (LTOT), vital signs were assessed on admission and after 1, 4 and 6 h of NIV application. Arterial blood gases (ABG) analysis was done before and 1 h after application of NIV. Laboratory investigations results including: complete blood count, C reactive protein (CRP), serum level of lactate dehydrogenase (LDH), lactate, urea, creatinine, albumin, sodium, and potassium were collected. Acute physiology and chronic health evaluation (APACHE) II score along with dyspnea, eosinopenia, consolidation, acidemia, atrial fibrillation (DECAF) score were calculated for every patient. Serum level of MR pro-ADM was measured using enzyme linked immunosorbent assay (human proadrenomedullin Elisa kit, Sino Geneclon Biotech Co., Ltd, China).
2.4 Statistical analysis
The data was statistically analyzed using Minitab program 17.1.0.0 for windows (Minitab Inc., 2013, Pennsylvania, USA). Continuous data were presented as mean and standard deviation (SD), and categorical data as number and percentage (%), the normality of data was examined using Shapiro–Wilk test. Comparison between the mean of two groups was performed by independent t-test, while Chi square test was used to compare between groups of categorical data. Logistic regression models with stepwise elimination were performed to determine the predictors of NIV failure in the studied cohort, as well factors associated with 30-days mortality. All tests were two-sided, p-value ˂ 0.05 was considered significant.
3 Results
The study included 45 patients, 36 males (80%) and 9 females (20%) with mean age of 63.4 ± 9.22 years. Patients were grouped into 2 groups; group A: NIV succeeded to correct the acute hypercapnic respiratory failure (34 patients, 75.6%) and group B: NIV failed to correct the acute hypercapnic respiratory failure (11 patients, 24.4%).
NIV failure was defined by any of the following: deterioration of the patient's condition, deterioration of conscious level, failure to alleviate symptoms, development of new symptoms or complications (e.g., pneumothorax, sputum retention, nasal bridge erosion), failure to improve or deterioration in ABG parameters, intolerance or failure of coordination with the ventilator [9]. NIV failure in our study was either due to failure to improve ABG parameters or failure to alleviate symptoms.
Mean values of serum MR-proADM levels in the study population were shown in Table 1.
Demographics of study population were summarized in Table 2.
Laboratory investigations and clinical scores of study population were shown in Table 3.
Comorbidities in our patients included diabetes mellitus and systemic hypertension.
NIV duration had a mean of 2.93 ± 1.98 days, and mean length of hospital stay was 8.77 ± 3.79 days with no significant difference between both groups. Nine patients (20%) died within 30 days.
Increasing APACHE-II score, increasing serum sodium, decreasing platelet count, lower pH on admission and after 1 h of NIV application, increasing PCO2 after 1 h of NIV application and presence of diabetes mellitus were found to be predictors of NIV failure (Table 4).
Increasing age, higher total leukocytic count and CRP and lower urea were found to be predictors of 30-day mortality (Table 5).
Serum level of MR-proADM was found to be related to higher BMI, higher platelet count (Table 6).
4 Discussion
During COPD exacerbations, MR-proADM levels increase, suggesting that it could be of special interest in that specific situation [4]. Increased circulating MR-proADM levels might contribute to the prevention of bacterial infection in AECOPD patients. It was also hypothesized that it could potentially promote bronchodilatation in AECOPD patients through inhibiting bronchoconstriction induced by histamine and acetylcholine. This suggests that plasma proADM levels during an exacerbation may reflect the ability or inability of patients to cope with the acute physiologic stress of exacerbation rather than mirroring the severity of the underlying lung disease [5]. So, we tried to assess the prognostic value of MR-proADM on NIV outcome and 30-day mortality in AECOPD patients.
Our results showed that mean values of serum MR-proADM levels (Table 1) did not vary significantly with NIV outcomes. As far as we know this was the first study to evaluate this role for MR-proADM.
In our study, MR-proADM levels correlated with 30-day survival (Table 1). The study [7] found that ADM levels did not differ significantly between survivors and non-survivors, while another study [4] reported that MR-proADM was significantly associated with the risk of poor outcome at 30 days in AECOPD patients.
In our study, age did not correlate with NIV outcome, which agrees with some studies [10, 11] leading to the conclusion that age should not be considered as a limiting factor for NIV treatment, while contradict with one study [12] who found that old age was associated with NIV failure which can be explained by poor mask-fitting, claustrophobia, excessive secretions, intolerance, agitation, and patient/ventilator asynchrony, most of which may be associated with poor respiratory muscle power [13].
Obesity causes reduction of lung and chest wall compliance, elevation of airway resistance, leading to increased risk of alveolar collapse, all of which could make obese patient more vulnerable to NIV failure [14]. Also, obese patients have worse quality of life, reduced 6-min walk distance, increased dyspnea and greater odds of severe AECOPD [15].
In our study there was no significant effect of BMI on NIV outcome. This was in line with some studies [12, 16] that found no relation between BMI and NIV outcome. And we disagree with other study [17] that found that BMI had the highest accuracy for predicting likelihood of NIV failure.
Diabetes mellitus worsens COPD outcomes as it increases length of hospital stay and risk of death during exacerbations, increasing modified medical research council (mMRC) dyspnea scores, and reducing six-minute walking distance [18]. In this study, diabetes mellitus was found to be a predictor of NIV failure (Table 4). Some studies [18, 19] reported similar results, while others [12] found that comorbidities had no predictive value on NIV outcome.
An important factor to be considered in predicting NIV outcome is the degree of acidosis. Furthermore, improvement in pH after few hours of the treatment, along with decrease in the respiratory rate is a predictor for positive outcome [10]. However; there is much debate about the correct cutoff value of pH to choose [18].
Our study (Table 4) showed that lower arterial pH at presentation was associated with increased risk of failure of NIV and the need for intubation. This is in concordance with other studies [10, 13, 18, 21, 22] that reported that pH on admission was highly related to NIV outcome. In addition to baseline, pH values after 1 h of NIV application was proved to be a powerful predictor of NIV outcome as well, in our study and also in some other studies [11, 23]. On the contrary, studies [3, 11, 24] did not identify any relation between pH and NIV failure.
Another variable that was found to be associated with NIV outcome in our study was PaCO2 after 1 h of NIV application. These results disagree with study [25] that recorded improvement in PaCO2 after 1 h in success and failure groups. Our results were in line with results of some studies [10, 11, 23] that reported lower values for the PaCO2 in the successful group after one hour of NIV treatment.
One of the beneficial effects of NIV is unloading of the respiratory muscles, decreasing the work of breathing and associated pulmonary hyperinflation so that dyspnea improves and the respiratory rate can fall [18]. In this study, patients in group B showed higher mean respiratory rate at presentation and after 1 h of NIV application than patients in group A (Table 3), however that was not statistically significant. These observations were in line with results of some studies [10, 23, 25].
APACHE II score could predict NIV outcomes (Table 4), as it was expected, as this index includes several factors each of them independently can predict the outcome. One study [22] reported that the lower APACHE II score contribute much to the lower NIV failure. Another study [25] found that patients with late failure of NIV had higher APACHE II score. Multiple studies [11, 20, 21] recorded similar observations.
Patients in group B had higher serum urea than patients in group A (Table 3), however that was not statistically significant. One study [26] stated that lower urea immediately prior to commencing NIV was significantly associated with a successful outcome and that the link between elevated urea and poor outcome is that it reflects a depleted intravascular volume and reduced vital organ perfusion.
Serum lactate was higher in group B than in group A but not of statistical significance (Table 3). One study [17] found higher serum lactate in the failure group but with no statistical significance which totally agree with our results. Another study [3] found that serum lactate had no predictive value for NIV failure.
Recently, elevated RDW was correlated with variety of diseases, including cardiovascular diseases, cerebrovascular diseases, pulmonary embolism, malignancy, diabetes mellitus and others. In addition, RDW is considered a powerful and independent risk factor for mortality. It is believed that an elevated RDW reflects a serious imbalance of homeostasis in the red blood cell caused by impaired erythropoiesis and abnormal erythrocyte survival, due to all kinds of metabolic disturbance [1]. Our study failed to demonstrate any difference between the 2 patient groups regarding RDW, this contradicts with the study [27] that stated that the presence of low RDW value was a predictor of NIV failure.
Other predictors of NIV failure included lower platelet count and higher serum sodium (Table 4), while hemoglobin, TLC, serum albumin, serum creatinine, CRP had no predictive value in NIV outcome. These totally agreed with Miller et al. [26] except for serum sodium.
In this study, 30-day mortality (Table 5) was 20% with increasing age, higher TLC, elevated CRP and lower serum urea as predictors of mortality. Advanced age, low pH, high paCO2, receiving home oxygen therapy and creatinine levels were associated with 30-day mortality in AECOPD patients in one study [28]. While another study [11] found that low BMI < 20 was associated with higher mortality rates in AEOCPD patients admitted in the intensive care unit.
We acknowledge that our study has some limitations, as the relatively small number of patients and being a single-center study that could limit the generalizability of results. Additionally predictive value of MR pro-ADM on NIV failure needs to be further evaluated for more verification of results.
5 Conclusion
One of the most important factors before application of NIV is to assess the probability of its failure, which can worsen the outcome of patients and increase the risk of mortality. Our results identified APACHE II score, platelet count, serum sodium, arterial pH initially and after 1 h of NIV, PaCO2 after 1 h of NIV and presence of diabetes mellitus as predictors of NIV failure. This may help appropriate patient selection for NIV and close monitoring, if the probability of failure is seen to be high.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABG:
-
Arterial blood gases
- ADM:
-
Adrenomedullin
- AECOPD:
-
Acute exacerbation of COPD
- APACHE II:
-
Acute physiology and chronic health evaluation II
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C- reactive protein
- DECAF:
-
Dyspnea, eosinopenia, consolidation, acidemia, and atrial fibrillation
- LDH:
-
Lactate dehydrogenase
- LTOT:
-
Long term oxygen therapy
- mMRC:
-
Modified medical research council
- MR-proADM:
-
Mid-regional proadrenomedullin
- NIV:
-
Non-invasive ventilation
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- RDW:
-
Red cell distribution width
- TLC:
-
Total leucocytic count
References
Zhu M, Peng H, Wan L, Zhang S, Zeng Y (2021) The role of elevated red blood cell distribution width in the prognosis of AECOPD patient. Medicine 100:10(e25010)
Supervía A, Pallàs O, Canas M, del Baño F, Cirera I, Iglesias M, Pedro-Botet J (2017) Non-invasive ventilation in hypercapnic COPD exacerbation: predictors of mortality. Lung Breath J 1(3):1–3
Bastiansen A (2014) Predicting failure of non-invasive ventilation in a mixed population. J Anesth Clin Res 5:1
Dres M, Hausfater P, Foissac F, Bernard M, Joly L, Sebbane M et al (2017) Mid-regional pro-adrenomedullin and copeptin to predict short-term prognosis of COPD exacerbations: a multicenter prospective blinded study. Int J COPD 12:1047–1056
Stolz D, Christ-Crain M, Morgenthaler N, Miedinger D, Leuppi J, Miiller C et al (2008) Plasma pro-adrenomedullin but not plasma pro-endothelin predicts survival in exacerbations of COPD. Chest 134(2):263–272
Zapata M, Villanueva M, Plaza F, Gomez C, Maldonado A, Moreno M (2017) Mid-Regional Proadrenomedullin as a prognosis biomarker of mortality in patients treated with non-invasive ventilation in the emergency room. Int J Crit Care Emerg Med 3(1):024
Meng D, Li X, Song X, Xin J, Yang W (2014) Diagnostic and prognostic value of plasma adrenomedullin in COPD exacerbation. Respir Care 59(10):1542–1549
Buderer NM (1996) Statistical methodology: Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med 3(9):895–900
BTS guidelines, (2002) Non-invasive ventilation in acute respiratory failure. Thorax 57:192–211
Pejkovska S, Jovkovska Kaeva B, Goseva Z, Arsovski Z, Jovanovska Janeva J, Zeynel S (2015) Predictive factors for the effect of treatment by noninvasive ventilation in patients with respiratory failure as a result of acute exacerbation of the chronic obstructive pulmonary disease. OA Maced J Med Sci 3(4):655–660
Steriade A, Johari S, Sargarovschi N, Necula D, Tudose C, Ionita D et al (2019) Predictors of outcome of noninvasive ventilation in severe COPD exacerbation. BMC Pulm Med 19:131–137
Ferreira C, Dias C, Mendes M, Moita J (2013) Predictors of failure of noninvasive ventilation (NIV) in acute respiratory failure due to chronic obstructive pulmonary disease. Eur Respir J 42:2492
Hong Y, Duan J, Bai L, Han X, Huang S, Guo S (2018) Noninvasive ventilation failure in pneumonia patients ≥ 65years old: the role of cough strength. J Crit Care 44:149–153
Chen Q, Liu M, Liu B, Li W, Gao D, Xie L et al (2020) Predictive factors for failure of noninvasive ventilation in adult intensive care unit: a retrospective clinical study. Can Respir J 2020:1324348
Donoghue O, Fergal J, Howard M (2014) Obesity, COPD, NIV and reverse epidemiology. Respirology 19(6):777–779
Wang J, Shang H, Yang X, Guo S, Cui Z (2019) Procalcitonin, C-reactive protein, PaCO2, and noninvasive mechanical ventilation failure in chronic obstructive pulmonary disease exacerbation. Medicine 98:17(e15171)
Ghazala L, Hatipoğlu U, Devnani T, Covert E, Hanks J (2021) Duration of noninvasive ventilation is not a predictor of clinical outcomes in patients with acute exacerbation of COPD and respiratory failure. Can J Respir Ther 57:113–118
Shaheen M, Daabisa R, Elsoucy H (2018) Outcomes and predictors of success of noninvasive ventilation in acute exacerbation of chronic obstructive pulmonary disease. Egypt J Bronchol 12:329–339
Chakrabarti B, Angus R, Agarwal S, Lane S, Calverley P (2009) Hyperglycaemia as a predictor of outcome during non-invasive ventilation in decompensated COPD. Thorax 64:857–862
Conti V, Paones G, Mollica C, Sebastiani A, Mannocci A, La Torre G et al (2015) Predictors of outcome for patients with severe respiratory failure requiring non-invasive mechanical ventilation. Eur Rev Med Pharmacol Sci 19:3855–3860
Çiftci F, Çileda A, Erol S, Kaya A (2017) Non-invasive ventilation for acute hypercapnic respiratory failure in older patients. Wien Klin Wochenschr 129:680–686
Duan J, Wang S, Liu P, Han X, Tian Y, Gao F et al (2019) Early prediction of noninvasive ventilation failure in COPD patients: derivation, internal validation, and external validation of a simple risk score. Ann Intensive Care 9:108–118
Ko B, Ahn S, Lim K, Kim W, Lee Y, Lee J (2015) Early failure of noninvasive ventilation in chronic obstructive pulmonary disease with acute hypercapnic respiratory failure. Intern Emerg Med 10:855–860
Sevic B, Obradovic D, Stefanovic S (2013) Severe respiratory acidosis in COPD not a predictor of noninvasive ventilation failure in high dependency unit? Poster Present Resuscitation 84:85
Chen T, Bai L, Hu W, Han X, Duan J (2020) Risk factors associated with late failure of noninvasive ventilation in patients with chronic obstructive pulmonary disease. Can Respir J 2020: article ID 8885464
Miller D, Fraser K, Murray I, Thain G, Currie G (2012) Predicting survival following non-invasive ventilation for hypercapnic exacerbations of chronic obstructive pulmonary disease. Int J Clin Pract 66:434–437
Yavsan M, Göktepe M, Tosun M, Karatas E, Teke T, Uzun K (2014) Red cell distribution width and mean platelet volume as a non-invasive ventilation success marker in COPD with acute hypercapnic respiratory failure. Eur Respir J 44:2091
İlhan B, Berikol G and Doğan H (2022) The predictive value of modified risk scores in patients with acute exacerbation of COPD: a retrospective cohort study. Intern Emerg Med 1–9
Acknowledgements
Not applicable.
Funding
Self-funded.
Author information
Authors and Affiliations
Contributions
M. A., H. H.: conception of the work and substantively revised the manuscript. R. H., M. M.: acquisition, analysis, of data and drafted the work. G. S.: design of the work, interpretation of data. All authors have approved the submitted version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the research ethics committee of faculty of medicine, Cairo university (No: MD-201-2019) and was conducted in accordance with the Helsinki Declaration. Written informed consent was obtained from all patients.
Consent for publication
Not applicable.
Competing interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elnady, M.A.E.H., Assal, H.H., Kandeel, R.H. et al. Mid-regional proadrenomedullin as a potential prognostic factor of NIV outcome in AECOPD. Beni-Suef Univ J Basic Appl Sci 12, 45 (2023). https://doi.org/10.1186/s43088-023-00383-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-023-00383-8