Abstract
Liver serves as a hub for key metabolic pathways such as folate cycle that provides one-carbon units for a network of metabolic reactions. Methylenetetrahydrofolate reductase (MTHFR) is a rate limiting enzyme in folate metabolism and thus it is vital for DNA methylation, synthesis and repair [1]. The objective of this study was to evaluate an eventual association between MTHFR polymorphisms C677T (rs1801133) and A1298C (rs1801131) and the susceptibility to hepatocellular carcinoma (HCC) in Egyptian population.
Blood samples from patients and controls from Mansoura university hospital were used after signed consent and approval from Medical ethical committee. The two genetic loci were designed for amplification and genotyped by using PCR–RFLP.
Our results clarify that, the most important predictors for HCC are T/T genotype of variant C677T and C/C genotype of variant (A1298C) with odds ratio 3.28 and 2.99 respectively. Also, MTHFR variant C677T genotype C/C or T/T combined with MTHFR variant A1298C genotype C/C were associated with an increased risk of HCC, with the OR, 2.6 and 7 respectively. CT genotype of MTHFR variant C677T showed significant difference between HCC grades and C allele of variant C677T showed significant difference in BCLC stages of HCC.
Our data indicates that, the two variants (C677T and A1298C) constitute a risk factor for the development of HCC and this could be attributed to the low activities of the enzyme MTHFR that disturb one carbon metabolism and subsequently, DNA synthesis, repair and methylation, thus cellular redox state, growth, and proliferation.
Similar content being viewed by others
Introduction
Hepatocellular cellular carcinoma (HCC) is the sixth most common cancer in the world and the third leading cause of cancer deaths [2]. The etiology of liver cancer remains unclear with varied risk factors such as hepatitis, obesity, type 2 diabetes, nonalcoholic fatty liver disease, the lifestyle of the individuals (consumption of contaminated food with aflatoxin, heavy drinking of alcohol, ingestion of moldy foods, raw water drinking) and genetic predispositions [3].
The liver is the main site for the metabolic detoxification of carcinogens, and for storing vitamins which serve as cofactors for enzymes involved in different metabolic pathways such as one-carbon metabolism [4].
Folate metabolic reaction involves the conversion of homocysteine to methionine which is transformed along with ATP to produce S-adenosylmethionine (SAM). SAM is a key substrate for methyl transferases [5]. Disturbance of folate cycle hinder methionine cycle with intracellular accumulation of S-adenosyl-homocysteine (SAH). Hyper homo cysteinemia (Hcy) may accelerate the progression of liver fibrosis possibly leading to liver cancer. SAH is a potent inhibitor of (SAM) dependent methylation reactions [6]. Homo-cysteine is a vascular toxin which may cause endothelial injury at various organs; because it is involved in the pathogenesis of oxidative stress [7].
Genetic polymorphisms are risk factors which necessitate some other pathological conditions in order to trigger a chain of biological events that cause cancer [8]. Folate levels and metabolism are necessary for normal and malignant cells [9]. Damage to the liver caused by aflatoxin B1, smoke toxins, ethanol consumption, as well as inflammatory reactions of HBV/HCV infection, may lead to the alternation of folate metabolism [10].
Single nucleotide polymorphisms (SNPs) play an important role in normal human variation [11]. Methylenetetrahydrofolate reductase (MTHFR) is a rate limiting enzyme in folate metabolism. MTHFR has two common genetic SNPs, (C677T and A1298C), encoding two MTHFR variants with a reduced activity and heterogeneous frequency in different regions of the world, about 10% in Caucasians [12]. MTHFR enzyme is coded by the MTHFR gene that is located on the short arm of chromosome 1 (1p36.3) and there are two isoforms in humans [13]. The first isoform is about 77 kDa protein, and the second is 70 kDa [14].
The single nucleotide polymorphism in MTHFR 677C-to-T results in a subsequent reduction in the enzyme activity and an increase in its thermolability [15]. The activity of the homozygous TT genotype is reduced by 70%, [16] and that the heterozygous CT genotype is reduced by 35% in comparison with the normal CC genotype [17]. MTHFR is pivotal for one-carbon metabolism that fuels the methionine cycle, de novo purine synthesis, transsulfuration pathway, serine, glycine, glutathione, thymidine production, and NADPH pools, and thereby regulates cellular redox state, growth, and proliferation. Dietary folic acid is the starting material for the folic acid cycle and folate deficiency may be due to genetic variation in (MTHFR) gene. Folate deficiency is associated with an increase in circulating homocysteine, hypo-methylation, and low level of 5-methyl tetra hydro folate (5-MTHF) leading to gene mutation or DNA strand breaks [18], [19]. Excess homocysteinemia in the presence of MTHFR variants C677T (rs1801133) and A1298C (rs1801131) increase pathology risks in general, and especially of, infertility, miscarriage and cancer susceptibility [20].
Excessive cigarette smoking and heavy alcohol consumption are associated with low plasma folate concentration, and hyperhomocysteinemia among patients with chronic hepatitis C infection, which may accelerate the progression of liver fibrosis in hepatic patients and possibly lead to liver cancer [21, 22]. MTHFR variant C667T has also been associated with an increased risk of invasive cervical cancer and premalignant lesions, which also indicate a possible role of MTHFR in viral infection-associated cancers [23]. The purpose of this case–control study is to assess the existence of associations between the MTHFR C677T and A1298C polymorphisms and the risk of HCC.
Material and method
The study is a case–control, including 50 patients with hepatocellular carcinoma on top of chronic HCV and 50 healthy subjects as a control group from Mansoura university hospital. The participants signed written approval consent. The study was approved by the Mansoura Faculty of Medicine ethical committee. Hepatocellular carcinoma was diagnosed by clinical, histopathological laboratory findings and radiological investigations including ultrasound and CT as indicated and reported according to Barcelona clinic liver cancer (BCLC). The patients with HCC had positive HCV antibodies and positive reverse transcriptase-polymerase chain for HCV genotype 4. Exclusion criteria included patients with hepatitis B virus, HIV, and patients with other cancers.
Fifteen-milliliter blood samples will be obtained from each participant and will be divided into three aliquots. One aliquot over EDTA for genomic DNA separation from the blood sample and the other aliquot will be used for sera separation. Sera will be subjected to the routine laboratory study of complete liver functions including alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin, and direct bilirubin by autoanalyzer (Dialab 450 system), determination of circulatory anti-HCV by Elecys system (Roche-diagnostic) and α fetoprotein (AFP) measurement by enzyme-linked immunosorbent assay (ELISA—DRG International Inc., USA.). The presence of HCV-RNA in patients’ sera was detected by real-time polymerase chain reaction. The third aliquot will be used for total blood counts by Sysmex and the determination of INR.
Molecular study of MTHFR C677T and A1298C polymorphisms
DNA Extraction
DNA was extracted from the blood samples with a Qiagen extraction kit from blood samples (Qiagen-Germany). The extracted DNA was kept frozen at -80 ºC till amplification.
Multiplex PCR for 677 and 1298 Loci of MTHFR Gene
Molecular study of methyl tetrahydrofolate reductase Polymorphism at 677 C /T and 1298 A / C polymorphisms was done by using PCR/RFLP. Odds ratios (OR) with 95% confidence intervals (CI) were used to assess the strength of association between both MTHFR C677T and A1298C polymorphisms and the risk of HCC.
The used primers for multiplex PCR are summarized in Table 1 [24]. The PCR reactions were conducted in 50 microns reaction mixture supplied by the Qiagen premix amplification kit. The mixture contains 10 mM Tris–HCl, pH 8.3, 50 mM KCl, 1.5 mM MgCl2, 0.2 mM of each dNTP, 50 pmol 677F, 50 pmol 677R, 100 pmol 1298F, and 100 pmol 1298R, 2.5 units of polymerase and 10 microns of the extracted DNA. The reaction mixture was incubated at 95 ºC for 8 min for initial activation of the Taq polymerase, followed by 40 cycles of 95 ºC for1 min, 63 ºC for 1 min, and 72 ºC for 1 min, with a final extension for 7 min at 72 ºC in the thermal cycler (Biosystem). Appropriate amplification of the predicted fragments was confirmed by digestion of the multiplex PCR products with HinfI or MboII and then electrophoresis on a 3% agarose gel for identification of the variants 677 C/T and 1298 A/C polymorphisms. Conditions for RFLP digestion are exactly as described by the manufacturer (Thermo Scientific-USA) [25].
Statistical analysis
Data are expressed as mean ± standard deviation or median for continuous data and number and % for discrete data. Non-normally distributed variables were analyzed by the Mann–Whitney test, while normally distributed variables were analyzed by t-test; categorical variables were compared using the Chi-square test. The effect of demographic parameters, clinical features, disease characteristics, genotypes, and alleles frequencies on HCC was investigated using univariate analysis in which all studied variables with p-value < 0.05 were considered as potential predictors and entered multivariable regression models. Deviation from Hardy–Weinberg equilibrium (HWE) expectations were determined using the chi-squared test. The statistical analysis was done by SPSS (statistical package for social sciences) version 25. Online SNP Stats software (http://www.snpstats.net/start.htm) analysis was applied to estimate the haplotypes and linkage.
Results
Table 2 shows the distribution of age, gender, and tumor characters among cases. More than two-thirds of the cases were male with a mean age of 55 years old. More than half of the cases were a class c Child–Pugh score (58%). The mean size of the mass was 4.8 cm. Two-thirds of the cases had one mass. Most of them were grade 3 and stage A Barcelona classification (42%). Two-thirds of them (60%) were right-sided tumors.
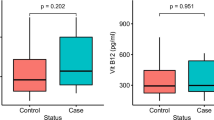
As in Table 3, platelets, albumin, ALT, AST and AFP were higher in cases than in control with a significant difference (P 0.01- 0.001). No significant difference was found regarding WBCs, Hb, and INR levels between the two groups.
Three genetic forms for each polymorphic locus were identified by RFLP. In cases, wild-type MTHFR 677CC was found in 30 (60%), the MTHFR 677CT heterozygous variant was present in 4 (8%), and the MTHFR 677 TT homozygous variant was found in 16 (32%). The MTHFR allele C was 64%, and T was 36%. While, in controls, wild-type MTHFR 677CC was found in 37 (74%), the MTHFR 677CT heterozygous variant was present in 10 (20%), and the MTHFR 677 TT homozygous variant was found in 3 (6%). The MTHFR allele C was 84% and T was 16%. For the allelic model C vs. T, the OR was 0.34 (95% CI: 0.17–0.66, p 0.001) (Table 4). In cases, wild-type MTHFR 1298AA was observed in 21 (42%) while MTHFR 1298AC heterozygous variant was noted in 15 (30%) and the MTHFR 1298CC homozygous variant was seen in 14 (28%) OR (0.23) (95% CI: 0.07–0.81, p 0.02). While, in controls, wild-type MTHFR 1298AA was observed in 26 (52%) while MTHFR 1298AC heterozygous variant was noted in 20 (40%) and the MTHFR 1298CC homozygous variant was seen in 4 (8%). For the allelic model A vs. C, the OR was 1.09 (95% CI: 0.62–1.9, p 0.67).
MTHFR (C677T and MTHFR A1298C) polymorphisms and the risk of HCC
Using the C/C genotype as the reference for MTHFR C677T, ORs were 2.02 (95% CI: 0.58–7.11) and 0.15 (95% CI: 0.04–0.57 P < 0.005) for the C/T and T/T genotypes, respectively with significant difference. OR for the T allele was 0.34 (95% CI: 0.17–0.66 P 0.001) when compared with the C alleles. Using the A/A genotype as the reference group for MTHFR A1298C, ORs were 1.08 (95% CI: 0.45–2.6) for the A/C without significant difference and 0.23 (95% CI: 0.62–1.9 P 0.02) for the C/C genotypes, with significant difference. Applying Hardy Weinberg equation (HWE), revealed that MTHFR C677T and in MTHFR A1298C in control subjects was in HWE while cases of both genotypes weren't in HWE. We evaluated the combined effect of different exposures on the risk of HCC. MTHFR 677 CC or TT genotype combined with MTHFR 1298 CC genotype were associated with an increased risk of HCC, with the OR, 2.6 and 7 respectively.
CT genotype of MTHFR variant C677T showed significant difference in different grade of HCC. The C allele of variant C677T showed significant difference BCLC stages. No significant difference in genotypes and alleles distribution exists between classes of Child–Pugh score or according to No or site of tumor mass (Table 5).
Regarding Multivariate analysis for HCC risk predictors, the most important predictors for HCC are T/T genotype of variant (C677T) and C/C genotype of variant (A1298C) with odds ratio 3.28 and 2.99 respectively (Table 6).
Discussion
HCC is a complex disease that involves multistep with multiple genes and gene-environment interactions. MTHFR is a critical enzyme in both DNA synthesis and methylation, thereby affecting DNA stability and gene expression; thus playing an important role in tumor progression. The frequency of the variant genotype is heterogeneous in different regions of the world.
The association of MTHFR C677T (rs1801133) and A1298C (rs1801131) polymorphism with HCC was more conflicting. Molecular epidemiologic studies have revealed that MTHFR polymorphisms are associated with an increased risk of esophageal cancer, breast cancer [26], gastric cancer [27], hepatocellular carcinoma [28], cervical neoplasia [29], [30], bladder cancer [31], and indolent prostate cancer [32]. Conversely, MTHFR polymorphisms have also been associated with a reduced risk of colon cancer [33], leukemia and lymphoma [34] and highly aggressive prostate cancer [35]. In addition, no association has been found between the C677Tvariant and colon adenoma and lung cancer [36].
Our study was a case–control, including 50 patients with hepatocellular carcinoma on top of chronic HCV and 50 healthy subjects, we evaluated the association between MTHFR polymorphisms C677T (rs1801133) and A1298C (rs1801131) and the susceptibility to hepatocellular carcinoma (HCC) in tertiary medical Egyptian center. More than two-thirds of the cases were male with a mean age of 55 years old. This goes with literature according to the demographic distribution of HCC [37]. Platelets count, serum albumin, ALT, AST and AFP showed a significant difference in cases than control as more than half of the cases were a class C Child–Pugh score (58%).
Three genetic forms for each polymorphic locus were identified by RFLP. Our study revealed that both cases of HCC and controls have more mutant alleles (i.e., homozygous mutant at either the 677 or 1298 site or heterozygous mutant at both loci) but without significant difference. Most of cases and control were of wild type MTHFR. Wild-type MTHFR 677CC was found in 30 (60%) of cases and in 37 (74%) of control. While wild-type MTHFR 1298AA was observed in 21 (42%) of cases and in 26 (52%) of controls. For the allelic model C vs. T, the OR was 0.34 (95% CI: 0.17–0.66, p 0.001) while for the allelic model A vs. C, the OR was 1.09 (95% CI: 0.62–1.9, p0.67).
Using the C/C genotype as the reference for MTHFR C677T, ORs were 2.02 (95% CI: 0.58–7.11) and 0.15 (95% CI: 0.04–0.57 P < 0.005) for the C/T and T/T genotypes, respectively with significant difference. Saffroy et al. [38] found that the wild MTHFR CC genotype was associated with the risk for HCC especially in patients with high alcohol consumption, whereas the TT genotype was related to a reduced risk for HCC (protective). MTHFR CC genotype was significantly higher in patients who had developed HCC on alcoholic cirrhosis rather than on viral cirrhosis ( P = 0.002) or on non-cirrhotic livers ( P = 0.02). The relative risk was 2.03. Further, Mu et al. [39] found that the MTHFR 677 C/T genotype was associated with an increased risk of primary liver cancer in a Chinese population.
CT genotype of MTHFR variant C677T showed significant difference in different grade of HCC. The C allele of variant C677T showed significant difference in BCLC stages. This may highlight the genetic susceptibility and role of gene polymorphism in HCC. Regarding Multivariate analysis for HCC risk predictors, the most important predictors for HCC are T/T genotype of variant (C677T) and C/C genotype of variant (A1298C) with odds ratio 3.282, 2.01 and 2.99 respectively.
Small sample size which represents a single center study may be a limiting factor. Also, serum folic acid was not measured among patients enrolled in this study despite that most of them have malnutrition status and mostly had low folate intake which is an independent factor affecting methylation of DNA.
Our results conclude that MTHFR polymorphism is a risk factor for the development of HCC but additional studies to further define their influence in the different stages of hepatocarcinogenesis are required.
Availability of data and materials
Data were collected from the registered medical records following the institutional ethics committee and agreement with the Helsinki Declaration of 1975, revised in 2008.
References
Xia B, Yang W, Liang H, Liu S, Wang D, Huang J (2022) Cancer Prevention Effects of Foods, Food Groups, Nutrients, and Their Underlying Mechanisms. ACS Food Sci Technol 2(3):437–454
Yeermaike A, Gu P, Liu D, Nadire T (2022) “LncRNA NEAT1 sponges miR-214 to promoted tumor growth in hepatocellular carcinoma,” Mamm Genome 33(3):525-533
Amer ME, Amer MA, Othman AI, Elsayed DA, El-Missiry MA, Ammar OA (2022) “Silymarin inhibits the progression of Ehrlich solid tumor via targeting molecular pathways of cell death, proliferation, angiogenesis, and metastasis in female mice,” Mol Biol Rep 49(6):4659-4671
Roberti A, Fernández AF, Fraga MF (2021) Nicotinamide N-methyltransferase: At the crossroads between cellular metabolism and epigenetic regulation. Mol Metab 45:101165
Alam J et al (2021) “Expression and analysis of the SAM-dependent RNA methyltransferase Rsm22 from Saccharomyces cerevisiae,” Acta Crystallogr Sect D Struct Biol 77(Pt 6):840-853
Maclean KN, Jiang H, Phinney WN, Mclagan BM, Roede JR, Stabler SP (2021) Derangement of hepatic polyamine, folate, and methionine cycle metabolism in cystathionine beta-synthase-deficient homocystinuria in the presence and absence of treatment: Possible implications for pathogenesis. Mol Genet Metab 132(2):128–138
H. is a vascular Toxin, Haque MF, Farzana T, Jahan I (2014) “Hyperhomocysteinemia: An Emergent Risk Factor of Atherosclerotic Vascular Disease”
Öksüz E et al (2022) Relationship between MTHFR Gene Polymorphisms and Gastrointestinal Tumors Development: Perspective from Eastern Part of Turkey. J Investig Surg 35(1):83–91
Zarou MM, Vazquez A, Vignir Helgason G (2021) “Folate metabolism: a re-emerging therapeutic target in haematological cancers,.” Leukemia 35(6):1539–1551
Rome FI, Hughey CC (2022) Disrupted liver oxidative metabolism in glycine N-methyltransferase-deficient mice is mitigated by dietary methionine restriction. Mol Metab 58:101452
Graf J, Hodgson R, Van Daal A (2005) Single nucleotide polymorphisms in the MATP gene are associated with normal human pigmentation variation. Hum Mutat 25(3):278–284
Mpoulimari I, Zintzaras E (2022) “Synthesis of genetic association studies on autism spectrum disorders using a genetic model-free approach,” Psychiatr Genet 32(3):91-104. YPG-0000000000000316
Koch MC, Stegmann K, Ziegler A, Schröter B, Ermert A (1998) Evaluation of the MTHFR C677T allele and the MTHFR gene locus in a German spina bifida population. Eur J Pediatr 157(6):487–492
Yang F, Qiu R, Abudoubari S, Tao N, An H (2022) Effect of interaction between occupational stress and polymorphisms of MTHFR gene and SELE gene on hypertension. PeerJ 10:e12914
Liu X-M, Liu F-H, Tang Y, Li Q (2012) MTHFR C677T polymorphism and pancreatic cancer risk: a meta-analysis. Asian Pacific J cancer Prev 13(8):3763–3766
Yang M, Vousden KH (2016) “Serine and one-carbon metabolism in cancer,.” Nature Reviews Cancer 16(10):650–662. https://doi.org/10.1038/nrc.2016.81 (Nature Publishing Group)
Li J, Li Z, Zhang J (2018) “Polymorphisms of methylenetetrahydrofolate reductase gene among women of childbearing age from Shiyan area”, Zhonghua yi xue yi Chuan xue za zhi= Zhonghua Yixue Yichuanxue Zazhi= Chinese. J Med Genet 35(4):572–576
Malaguarnera G et al (2022) Serum Folate deficiency in HCV related Hepatocellular Carcinoma. Sci Rep 12(1):1–10
Harlan De Crescenzo A et al (2021) Deficient or excess folic acid supply during pregnancy alter cortical neurodevelopment in mouse offspring. Cereb Cortex 31(1):635–649
Petrone I, Bernardo PS, Dos Santos EC, Abdelhay E (2021) MTHFR C677T and A1298C polymorphisms in breast cancer, gliomas and gastric cancer: a review. Genes (Basel) 12(4):587
Haber PS, Kortt NC (2021) Alcohol use disorder and the gut. Addiction 116(3):658–667
Neamatallah M et al (2022) “Association of Vitamin D Gene Polymorphisms With HCV Infection Outcome,” Br J Biomed Sci 79:10237.
Abdel Allah HMM, W. E. Zahran, S. A. El-Masry, M. El-Bendary, A. F. Soliman, (2021) “Association of MTHFR and TYMS gene polymorphisms with the susceptibility to HCC in Egyptian HCV cirrhotic patients,” Clin Exp Med 22(2):257-267 pp. 1–11
P. Frosst et al (1995) “• A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase,” Available: http://www.nature.com/naturegenetics
P. Yi, I. P. Pogribny, and S. J. James “Multiplex PCR for simultaneous detection of 677 C ! T and 1298 A ! C polymorphisms in methylenetetrahydrofolate reductase gene for population studies of cancer risk.” Available: www.elsevier.com/locate/canlet
Omran MH, Fotouh BE, Shosha WG, Ismail A, Ibrahim NE, Ramadan SS (2021) Strong Correlation of MTHFR Gene Polymorphisms with Breast Cancer and its Prognostic Clinical Factors among Egyptian Females. Asian Pacific J cancer Prev APJCP 22(2):617
L. Xu et al (2017) “Methylenetetrahydrofolate reductase C677T polymorphism and colorectal cancer susceptibility: A meta-analysis,” Biosci Rep vol. 37, no. 6. https://doi.org/10.1042/BSR20170917
Wang B, Ma M, Guo X, Yan Y, Li L (2021) “Associations between methylenetetrahydrofolate reductase polymorphisms and hepatocellular carcinoma risk: An update meta-analysis and trial sequential analysis,.” Medicine (Baltimore) 100(41):e27527. https://doi.org/10.1097/MD.0000000000027527
Waker CA, Kaufman MR, Brown TL (2021) “Current state of preeclampsia mouse models: approaches, relevance, and standardization,” Front Physiol 12:681632.
Parsaeian SF et al (2021) A Meta-Analysis for Association of XRCC3 rs861539, MTHFR rs1801133, IL-6 rs1800795, IL-12B rs3212227, TNF-α rs1800629, and TLR9 rs352140 Polymorphisms with Susceptibility to Cervical Carcinoma. Asian Pacific J Cancer Prev 22(11):3419–3431
Qian S, Tan J, Zhou Q, Yin J, Li H, He Y (2021) The Relationship Between GSTT1, GSTM1, GSTO1, GSTP1 and MTHFR Gene Polymorphisms and DNA Damage of BRCA1 and BRCA2 Genes in Arsenic-Exposed Workers. J Occup Environ Med 63(4):e177–e183
Ganini C et al (2021) Serine and one-carbon metabolisms bring new therapeutic venues in prostate cancer. Discov Oncol 12(1):1–13
Lak R, Kazemi E, Aavani P, Alaei F, Pashizeh F (2021) Association analysis of C677T and A1298C polymorphisms in MTHFR gene in patients with colorectal cancer susceptibility. Cent Asian J Med Pharm Sci Innov 1(2):74–80
S. Hou et al (2014)“Genome-wide association analysis of Vogt-Koyanagi-Harada syndrome identifies two new susceptibility loci at 1p31.2 and 10q21.3,” Nat Genet vol. 46, no. 9. https://doi.org/10.1038/ng.3061
Yadav U, Kumar P, Dwivedi S, Singh BP, Rai V (2021) “Folate (MTHFR C677T and MTRR A66G) genepolymorphisms and risk of prostate cancer: a case-control study with an updated meta-analysis,” medRxiv.doi: https://doi.org/10.1101/2021.01.06.21249185
Walia HK, Singh N, Sharma S (2021) “MTHFR polymorphism as a predictive biomarker for gastrointestinal and hematological toxicity in North Indian adenocarcinoma patients,” J Chemother 34(5):326-340
Serraino D, Fratino L, Piselli P (2023) Epidemiological Aspects of Hepatocellular Carcinoma. In: Ettorre GM (ed) Hepatocellular Carcinoma. Updates in Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-09371-5_1
Saffroy R, Pham P, Chiappini F, Goupil M, Castera L et al (2004) The MTHFR 677C > T polymorphism is associated with an increased risk of hepatocellular carcinoma in patients with alcoholic cirrhosis. Carcinogenesis Vol 25(Issue 8):pp 1443-1448
Mu LN, Cao W, Zhang ZF, Cai L, Jiang QW, You NC, Goldstein BY, Wei GR, Chen CW, Lu QY, Zhou XF, Ding BG, Chang J, Yu SZ (2007) Methylenetetrahydrofolate reductase (MTHFR) C677T and A1298C polymorphisms and the risk of primary hepatocellular carcinoma (HCC) in a Chinese population. Cancer Causes Control 18(6):665–675
Acknowledgements
Not applicable.
Conflicts of interests
Nothing to declare by the authors.
Confirmation
*All authors have confirmed the manuscript for submission in this journal.
*The content of this manuscript has not been published, or submitted for publication elsewhere.
Funding
Nothing to declare.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Fatma Abozeid,Dina Elhammady, Ahmed yassen.Material preparation by Amany Ragab, Aya fathy, Mohamed Serria, Omar Ammar. The manuscript was written by Maysaa Zaki, Fatma Abozeid. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethical Committee of the Faculty of Medicine of Mansoura University approved the study and the patients to participate.
The participants signed written approval consent.
Consent for publication
All authors have confirmed the manuscript for submission and publication in this journal.
Competing interests
Nothing to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abozeid, F., Zaki, M., Nagah, W. et al. Associations of methylene tetrahydrofolate reductase (MTHFR) polymorphism with hepatocellular carcinoma in Egyptian population. Egypt Liver Journal 14, 34 (2024). https://doi.org/10.1186/s43066-024-00342-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-024-00342-7