Abstract
Introduction
Radiofrequency ablation (RFA) and microwave ablation (MWA) are widely accepted as the established treatment options for patients diagnosed with early-stage hepatocellular carcinoma (HCC) who are deemed unfit for surgical procedures. However, the effective implementation of these techniques is hindered by various challenges, primarily associated with the precise targeting of tumors within the liver. The utilization of thermal ablative methods is not recommended for hepatocellular carcinoma (HCC) that is located near intestinal loops, bile ducts, or in eccentric positions. The unmet need for non-thermal methods in the treatment of hepatocellular carcinoma (HCC) was addressed following the introduction of irreversible electroporation (IRE) as an innovative approach.
Aim of the work
To assess the efficacy, safety, and outcomes of IRE in the treatment of difficult-located HCC compared to transarterial chemoembolization (TACE).
Methods
This is a prospective study that included 24 patients with HCC who presented to the National Hepatology and Tropical Medicine Research Institute (NHTMRI) during the period from January 2017 to January 2020. Ten patients underwent IRE, while 14 patients underwent TACE.
Results
Sixteen patients (66.7%) were males; eight patients were females (33.3%). Their median age was 60.5 years (48–70 years). Seventeen patients (70.8%) were Child–Pugh class A, while seven patients (29.2%) were Child–Pugh class B. All the study population had a single focal lesion; the mean size of the focal lesions was 2.94 ± 0.59 cm. The most frequent difficult locations of HCC were segment V focal lesions adjacent to both the common bile duct and portal vein in eight patients (33.3%) followed by lesions adjacent to the inferior vena cava in five patients (20%) followed by the subcapsular lesions in three patients (12.5%) and lesions adjacent to the right kidney in two patients (8.3%). Complete response (CR) was higher in the IRE group (80%) compared to the TACE group (50%). Clinical decompensation occurred in six patients in the IRE group (60%) and eight patients in the TACE group (57.1%) (P value 1). Recurrence occurred in five patients (50%) treated with IRE and in seven patients (50%) treated with TACE (P value 1). Within the IRE group, two patients (20%) remained alive; on the other hand, within the TACE group six patients (42.9%) remained alive by the end of the study (P value 0.388).
Conclusion
Our data suggest that IRE is an effective procedure in the treatment of difficult-located HCC in terms of complete response, fewer sessions, and fewer side effects as compared to TACE.
Similar content being viewed by others
Introduction
With an anticipated incidence of more than one million cases by 2025, liver cancer continues to be a global health concern. Ninety percent of instances of liver cancer are attributed to hepatocellular carcinoma (HCC), the most prevalent kind of the disease [1]. The two primary curative interventions for HCC cases have been hepatic resection and liver transplantation. Improvements in patient selection have produced excellent 10-year post-liver transplantation survival rates and improved surgical resection results [2].
Although microwave thermal ablation (MWA) and radiofrequency ablation (RFA) were believed to be very successful minimally invasive treatment options for HCC, there are still several challenges associated with their use, most of which are connected to the location of the tumor. When tumors are located eccentrically or next to bile ducts or intestinal loops, it is not recommended to employ these thermal ablative techniques. The development of irreversible electroporation (IRE) addressed the unmet demand for non-thermal HCC therapy methods [3].
In the realm of interventional oncology, IRE has become popular. According to Rubinsky [4], this non-thermal method of tumor ablation has a lower rate of collateral damage and is not impacted by the heat sink effect. In particular, IRE uses extremely brief, high-voltage electrical pulses to cause pores to develop in cells’ lipid bilayers, which causes apoptosis. Because collagenous structures are preserved inside the ablation field, parenchymal architecture is maintained [5].
Preservation of vital structures within the IRE-ablated zone is another unique characteristic of IRE ablation. In all IRE-ablated liver tumors, critical structures, such as the hepatic arteries, hepatic veins, portal veins, and intrahepatic bile ducts, were all preserved [6]. In other types of tumor ablation, these structures are completely obliterated due to the extreme temperature changes causing the denaturation of proteins [6]. IRE is a relatively new technique for tumor ablation. It has shown promising results in difficult cases where surgery is not recommended and delicate anatomic structures are present near or within the tumor. Currently, liver cancer is one of the most common targets for IRE treatment [7].
This study aimed to assess the efficacy and safety of IRE in the treatment of difficult-located HCC in comparison to TACE and to compare the long-term follow-up results of the two techniques.
Patients and methods
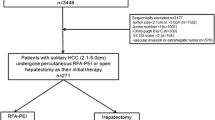
The National Hepatology and Tropical Medicine Research Institute’s HCC unit conducted this prospective study (NHTMRI). Twenty-four patients with challenging localization HCC who visited NHTMRI between January 2017 and January 2020 were included in the current study. These 24 patients were chosen from 270 HCC patients who visited the NHTMRI HCC unit over the study’s duration. Ten patients received IRE, while 14 had TACE (transarterial chemoembolization). All patients signed a written informed consent before inclusion in the study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This study was carried out following the 1975 Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments and its later amendments. The protocol of this study was approved by the ethics committee of the Faculty of Medicine, Cairo University (Number: N-46–2017).
The inclusion criteria for both IRE and TACE groups were as follows: patients diagnosed with a single HCC by dynamic imaging (triphasic CT and/or dynamic MRI) with or without elevated serum alpha-fetoprotein with a maximum tumor diameter of 4 cm. Difficult-located tumors included HCC adjacent to bowel loops, gall bladder, major vessels (inferior vena cava, hepatic veins, and portal vein), bile duct, vital organs (right kidney), and caudate lobe HCC. Subcapsular (does not intend the liver capsule) and partially exophytic (less than 50% of the tumor size bulging outside the capsule) tumors were included.
Suitable laboratory parameters for performing the intervention are hemoglobin more than 10 g/dl, platelets count more than 60,000/cmm and INR not more than 1.6, Child-Turcotte-Pugh class A and early B up to score 8, and compensated cardiac condition.
We excluded patients with ascites, patients with extrahepatic or vascular spread of HCC, patients with cardiac arrhythmias, or those with artificial pacemakers. The decision to allocate the patient to one of the two treatment modalities (IRE versus TACE) was based on random selection (United States Office of Research Integrity, 1992).
All patients were subjected to full history taking, laboratory investigations, complete blood count, liver profile as serum albumin, total bilirubin, INR, AST, ALT, and radiological investigations such as abdominal ultrasound, triphasic CT abdomen, and/or dynamic MRI.
Irreversible electroporation (IRE) (Nanoknife system)
IRE is a local application of a series of brief (ultra short) but intense (strong) electrical pulses, causing innumerable permanent lethal nanopores in the cell membrane, thus disrupting the cellular homeostasis and leading to permanent cell death from apoptosis, not necrosis as in all other thermal or radiation-based ablation techniques [8].
IRE was performed by an expert in interventional ultrasound locoregional therapy using the Nanoknife system, Angiodynamics, Inc®. Queensbury, NY, USA.
The IRE system consists of a computer-controlled pulse generator that delivers 3000-V pulses to the IRE probes. Typically, a minimum of 90 pulses are delivered, which last from 20 to 100 µs each. The number of probes inserted inside the tumor is determined according to the tumor dimensions, which also specify the spacing of probes needed to create the desired ablation zone based on the input data to the central processing unit [9].
The needles were multiple monopolar 19-gauge radio-opaque probes, spaced 15 to 22 mm apart, and were used depending on the electroporation zone to be achieved. The insertion, adjustment, and follow-up till withdrawal of the needles were done under ultrasonographic guidance.
General anesthesia with deep neuromuscular blockade was used in all cases to achieve paralysis to zero twitches. This level of paralysis is needed to prevent patient movement when the high-voltage pulses are delivered. General anesthesia was achieved by propofol (0.5–1 mg/kg), fentanyl (1 mg/kg), and atracurium (0.5 mg/kg) followed by maintained inhalation on isoflurane (1.5 to 3% in oxygen) with controlled ventilation.
Treatment planning was based on preoperative imaging with CT scanning in which the tumor dimensions and morphology were measured and uploaded into the pulse generator software. The number and spacing of probes needed to create the desired ablation zone were calculated by the generator software, based on the computer algorithm. The probes are placed in a manner as to bracket the tumor, rather than violate the tumor itself.
The tumor must be completely encased by the needle probes. The ablation time for four electrodes was 9 min. Ablation technical success was defined as the ability to successfully deliver all the planned pulses (at least 90) following the size and dimension of the lesion plus the absence of tumoral enhancement on follow-up dynamic CT after 1 month from the session of ablation [10].
Post ablation the patients were transferred from the interventional ultrasound unit to the ward department. Vital signs (blood pressure, pulse, and temperature) were monitored every 4 h for the next 24 h and patients were discharged after follow-up abdominal ultrasound to exclude any abdominal collection or development of ascites.
Transarterial chemoembolization (TACE)
TACE was performed by an expert in interventional radiology. The procedure involves gaining percutaneous transarterial access by the Seldinger technique to the hepatic artery with an arterial sheath, by puncturing the common femoral artery in the right groin and passing a catheter guided by a wire through the abdominal aorta, through the celiac trunk and common hepatic artery, and finally into the branch of the proper hepatic artery supplying the tumor.
The interventional radiologist then performed a selective angiogram of the celiac trunk and possibly the superior mesenteric artery to identify the branches of the hepatic artery supplying the tumor(s) and threaded smaller, more selective catheters into these branches. This was done to maximize the amount of the chemotherapeutic dose that was directed to the tumor and minimize the amount of the chemotherapeutic agent that could damage the normal liver tissue. When a blood vessel supplying the tumor has been selected, alternating aliquots of the chemotherapy (adriamycin/cisplatin) dose mixed with lipidol and embolic particles were injected through the catheter as follows:
-
Ten milliliters of 50 mg doxorubicin hydrochloride powder mixed in isotonic saline 0.9% or 10 ml of 50 mg cisplatin liquid mixed with lipidol adjusted according to the volume of the tumor
-
Embolic material: gel foam or variable-sized poly vinyl alcohol (PVA) or Embosphere Microspheres variable according to the type and size of arterio-portal (AP) shunts
The total chemotherapeutic dose was either given in one vessel’s distribution or was divided among several vessels supplying the tumor.
Follow-up
Follow-up was performed for all patients using triphasic CT abdomen, INR, CBC, albumin, bilirubin, and alpha-fetoprotein, after 1 month then triphasic CT abdomen every 3 months in the first year then every 6 months till the end of the study. The mean follow-up period was 24 months.
All patients were assessed for the absence of tumor hyper-enhancement on follow-up imaging and according to the modified Response Evaluation Criteria in Solid Tumors (mRECIST) [11].
-
1.
Complete response: Disappearance of any intra-tumoral arterial enhancement in all target lesions
-
2.
Partial response: At least a 30% decrease in the sum of diameters of viable (enhancement in the arterial phase) target lesions, taking as reference the baseline sum of the diameters of target lesions
-
3.
Stable disease: Any cases that do not qualify for either partial response or progressive disease
-
4.
Progressive disease: An increase of at least 20% in the sum of the diameters of viable (enhancing) target lesions, taking as reference the smallest sum of the diameters of viable (enhancing) target lesions recorded since treatment started [11]
Statistical methodology
Analysis of data was done using SPSS (statistical program for social science version 12) as follows: description of quantitative variables was performed using mean, SD, and range. A description of qualitative variables was performed using numbers and percentages. The chi-square test was used to compare qualitative variables between the groups. P value is considered insignificant if > 0.05 while considered significant if < 0.05 and is highly significant if < 0.01 [12].
Results
When we compared the two studied groups, there were no differences among the patients regarding their age, gender distribution, presence of diabetes mellitus, and Child–Pugh score. Sixteen patients (66.7%) were males; eight patients were females (33.3%). The median age of the 24 patients was 60.5 years (range, 48–70 years). The mean age of the IRE group was 59.2 years, while the mean age of the TACE was 60.6 years (P value = 0.546). Eight patients (57.1%) of the TACE group had previous HCC ablation, while only two patients (20%) of the IRE group underwent previous HCC ablation (Table 1).
As regards the virology status of the studied patients, 22 patients (91.7%) were HCV Ab positive. Eleven patients (45.8%) had positive HCV RNA before ablation. All 24 patients (100%) were HBV negative. Two of our patients were virology-negative patients (8.3%), one male patient had a history of bilharziasis, and the other female patient had a history of diabetes.
When we compared the two groups regarding the virological background and laboratory parameters, apart from the significantly higher AST level in the TACE group, there was no statistically significant difference between both groups in the rest of the parameters (Table 2). Regarding the radiological features of the studied groups, we found no statistical difference among the studied groups regarding their tumor features. All the study population had a single focal lesion (Table 3). The mean focal lesion size for the TACE group was 3.11 cm (range from 2.5 to 3.8 cm), and the mean focal lesion size for the IRE group was 2.69 cm (1.7 to 3.5 cm) (P value 0.212). All patients in the IRE group had the focal lesion in the right lobe (100%), whereas, in the TACE group, eight patients (57.1%) had the focal lesion in the right lobe, four patients (28.6%) had focal lesions on the left, and two patients (14.3%) had focal lesions in the caudate lobe.
The most encountered specific sites for HCC in the IRE group were segments IV and V (8 out of 10 patients) while HCC in segments I, II, and III were only present in the TACE group (5 out of 14 patients). All the 24 patients in the two groups IRE and TACE had a patent portal vein and all patients had no lymph node metastasis. According to BCLC, eight patients in the IRE group (80%) were stage A and two patients in the IRE group (20%) were stage B, in contrast to all the 14 patients in the TACE group were BCLC class A (P value 0.163) (Table 3).
This study did not reveal statistical significance among the two groups regarding their treatment response, post-treatment hepatic decompensation, recurrence, or mortality (Table 4). The two most common causes of decompensation in patients in the IRE group were ascites (33.3%) and portal vein thrombosis (33.3%) respectively over 2 years of follow-up while the most common cause of decompensation in the TACE patients was the development of ascites (50%) over 2 years of follow-up. Within the IRE group, five patients (62.5%) developed recurrence away from the primary ablated HCC site over 2 years of follow-up and two patients (20%) remained alive. On the other hand, within the TACE group, seven patients (53.8%) developed new lesions (five patients recurrence in the same primary HCC site that needed further sessions and two patients away from the primary site) and six patients (42.9%) remained alive (Table 4).
The cause of death in 12 of the studied patients was due to long-term complications of recurrent metastatic HCC and liver cell failure. Refractory ascites, hepatic encephalopathy, and hemodynamic instability (shock) were their last presentation. One patient with portal vein thrombosis died from hypovolemic shock due to massive hematemesis and melena even after performing endoscopic variceal ligation bedside in the intensive care unit. One patient died from complications of COVID-19 pneumonia. One patient died from complications of malignant obstructive jaundice and a very high bilirubin level not eligible for biliary drainage and renal failure. One patient died from massive pleural effusion and lung infection followed by respiratory failure.
Seven patients in the IRE group had Child–Pugh class A. Using the modified RECIST criteria, two patients had a partial response and five patients had a complete response. Six patients died after 2 years of follow-up, three patients experienced a recurrence of HCC following total ablation, and five patients with Child–Pugh class A displayed hepatic decompensation.
Furthermore, three individuals in the IRE group had a Child–Pugh class B-7. They all had a complete response. After 2 years of follow-up, one patient developed hepatic decompensation, two patients experienced HCC recurrences, and one patient was still alive.
There were ten patients with Child–Pugh class A in the TACE group. Five patients had a complete response, while five achieved a partial one. Hepatic decompensation occurred in six of the Child–Pugh class A patients, and six patients had HCC recurrence. Six Child–Pugh class A patients died away by the time the study was finished.
Furthermore, two patients in the TACE group demonstrated a partial response, and two patients with a Child–Pugh class B-7 attained a complete response. Two patients displayed decompensation and after achieving complete response, one patient experienced an HCC recurrence. By the time the trial was over, two Child–Pugh class B patients died (Figs. 1, 2, 3, 4, 5, and 6).
Discussion
The results of our study revealed that there was no significant difference in the treatment outcome, post-treatment decompensation, recurrence, and mortality among comparable patients with difficult location HCC treated with IRE versus TACE.
Our study also revealed that IRE can be used in patients with Child–Pugh class B (7/8) with adequate results. Few studies have assessed the tolerability and efficacy of IRE in the treatment of Child–Pugh B (7/8) patients with hepatocellular carcinoma (HCC). A previous single-center study included 23 patients (median age 65.2 years, range 38.8–84.0) with 33 HCCs who were treated via IRE. The majority of patients had well-compensated Child–Pugh A cirrhosis due to either alcohol and/or hepatitis C. Eight patients received IRE for more than one lesion either concurrently or on separate occasions. Their median tumor size was 2.0 cm (range 1.0–5.0 cm) [13]. The complete response (CR) rate was 92.9% for lesions smaller than 2 cm, 90.0% for lesions 2–3 cm, and 77.8% for lesions larger than 3 cm. The three lesions that required two procedures were all larger than 3 cm and were all complicated by local recurrence during follow-up. Of the four lesions that had residual disease, three were large lesions (5.0, 3.9, and 2.9 cm) [13]. These data agree with our study, as our patients in the IRE group had an 80% complete response according to mRECIST criteria.
Freeman and colleagues reported that 12 (52.2%) out of 23 patients were still alive by the end of their study. All 11 deaths were liver-related (HCC or end-stage liver failure) [13]. On the other hand, in our study, two patients remained alive (20%). Death was mainly due to the natural course of illness related to long-term complications of cirrhosis and liver cell failure.
Another study by Sutter and colleagues, who recruited 58 patients with 75 HCCs considered contraindicated to ordinary thermo-ablative techniques and treated them with IRE, reported 92% complete ablation [14]. Previous studies used IRE as its main therapeutic effect apoptosis, rather than necrosis and distortion of cells and/or connective structures, like with pure thermal ablative techniques. Thus, IRE is an effective and safe modality to treat tumors located close to critical structures, such as hilar biliary ducts for central locations or diaphragm and digestive tract for peripheral subcapsular locations [14].
Another study [15] included 300 patients (mean age: 51 to 66.6 years,male: 182; female: 118) from 9 studies of hepatic malignant tumors. The meta-analysis showed that compared with the initial values, the longest diameter of the tumors was significantly decreased at the last follow-up months after IRE. Furthermore, the ALP, AST, and total bilirubin levels were increased 1 day after IRE while returning to baseline at the last follow-up month. The pooled data indicated that IRE could be a minimally invasive and effective approach for patients who had preoperative poor liver function or those whose masses were in refractory locations where surgical resection was unsuitable.
The outcome of TACE appears to depend on careful patient selection. In an RCT that recruited patients with compensated cirrhosis (70% in Child–Pugh A), absence of cancer-related symptoms (81% with ECOG performance status of 0), and large or multinodular HCC with neither vascular invasion nor extrahepatic spread, 2-year survival after conventional TACE reached 63%, compared with 27% of the untreated control arm (P = 0.009) [16].
The above data is consistent with the results gained from our study for the control group using TACE, whereas, the 2-year survival rate was 43%, with a similar response to mRECIST treatment (50%), suggesting similar outcomes for the HCC patients enrolled in this study with regard to TACE.
As regards TACE technique in another trial, between November 2005 and August 2016, Lee et al. retrospectively reviewed 74 patients with a single HCC ≤ 5 cm or up to three HCCs ≤ 3 cm without vascular invasion or extrahepatic metastasis who were treated with RFA (n = 43) or TACE (n = 31). The overall survival (OS) and local progression rates were compared after propensity score analysis [17]. The mean follow-up period was 2.8 ± 1.9 years. The 1-, 2-, and 3-year survival rates were 97.1, 94.0, and 80.7% for the RFA group and 89.0, 80.8, and 62.0% for the TACE group, respectively. The clinical variables of the RFA and the TACE groups were well balanced by propensity score adjustment, and the RFA group showed better OS (P = 0.039) and local progression rates (P = 0.004) than the TACE group [17].
Our current study has several limitations. First, as a single-institution study, it suffers from bias in the use of ablation as an adjunct to surgical resection. Additionally, both groups in our study consisted of relatively few patients (14 and 10, respectively).
IRE appears to be a safe treatment for hepatic tumors in proximity to vital structures. Further prospective evaluation is needed to determine the optimal effectiveness of IRE concerning size and technique for IRE of the liver [18].
In conclusion, irreversible electroporation represents a safe, effective ablative modality for the treatment of hepatocellular carcinoma in the setting of Child–Pugh A and early B liver dysfunction in difficult locations. Its safety and efficacy compare favorably with TACE.
Given the benefits of its non-thermal nature, IRE may broaden local ablative options for HCC, in particular, when standard local curative treatments are difficult to perform. Further studies are warranted to compare IRE to other standard HCC therapies.
Conclusion
This study revealed that IRE is comparable to TACE in the treatment of compensated patients with difficult location HCC as regards treatment outcome, post-treatment decompensation, recurrence, and mortality.
Availability of data and materials
All relevant data are included in the manuscript and its supporting information files. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Llovet JM, Kelley RK, Villanueva A et al (2021) Hepatocellular carcinoma. Nat Rev Dis Primers 7(1):6. https://doi.org/10.1038/s41572-020-00240-3
Tabrizian P, Jibara G, Shrager B et al (2019) (2019): “Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis.” Ann Surg 261(5):947–955
Guo Tian, Qiyu Zhao, Fen Chen, Tian’an Jiang, Weilin Wang (2016) Ablation of hepatic malignant tumors with irreversible electroporation: a systemic review and meta-analysis of outcomes. Oncotarget 20(4):5853–5860
Rubinsky B (2007) Irreversible electroporation in medicine. Technol Cancer Res Treat 6(4):255–259
Lee EW, Totonchy M, Kee ST et al (2020) Radiology key: Irreversible Electroporation ablation: mechanism of action and devices. https://doi.org/10.1055/b-0034-81502
Asha Z (2017) Grand David and Kevin P charpentier (2017): Irreversible electroporation of hepatocellular carcinoma: patient selection and prospective. J Hepatocell carcinoma 4:49–58
Figini M, Wang X, Lyu T, Su Z, Procissi D, Yaghmai V et al (2017) Preclinical and clinical evaluation of the liver tumor irreversible electroporation by magnetic resonance imaging. Am J Transl Res 9:580–590
Tian G, Zhao Q, Chen F, Jiang T, Wang W et al (2017) Ablation Of Hepatic Malignant Tumors With Irreversible Electroporation: A Systematic Review And Meta-Analysis Of Outcomes. Oncotarget 8(4):5853–5860. https://doi.org/10.18632/oncotarget.14030
Wang G, Zhu S, Li X (2019) Comparison of values of CT and MRI imaging in the diagnosis of hepatocellular carcinoma and analysis of prognostic factors. Oncol Lett 17:1184–1188. https://doi.org/10.3892/ol.2018.9690
Thomson KR, Kavnoudias H, Neal RE (2015) Introduction to irreversible electroporation-principles and techniques. Tech Vasc Interv Radiol 18(3):128–134 ([PMID: 26365541])
Llovet JM, Riccardo Lencioni (2020) Journal of Hepatology 72(2):288–306. https://doi.org/10.1016/j.jhep.2019.09.026
Miller MC, Knapp RG (1992) Clinical epidemiology and biostatistics. Harwal Publishing company, Malverin, The national medical series for independent study, pp 275–292
Freeman E, Cheung W, Ferdousi S, Kavnoudias H, Majeed A, Kemp W, Roberts SK (2021) Irreversible electroporation versus radiofrequency ablation for hepatocellular carcinoma: a single center propensity-matched comparison. Scand J Gastroenterol. 56(8):942–947
Sutter O, Niessen C, Igi J, Pregler B et al (2017) Factors associated with short-term local recurrence of liver cancer after percutaneous ablation using irreversible electroporation: a prospective single-center study. J Vasc Interv Radiol 26(5):694–702
Guo Tian, Qiyu Zhao, Fen Chen, Tian’an Jiang, Weilin Wang (2017) Ablation of hepatic malignant tumors with irreversible electroporation: a systemic review and meta-analysis of outcomes. Oncotarget 8(4):5853–5860
Montaña X et al (2002) Barcelona Liver Cancer Group. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 359(9319):1734–1739
Lee, Bo-Ching, Liu Kao-Lang, Wu, Chih-Horng, Huang, Kai-Wen et al (2018) Comparison of radiofrequency ablation and transarterial chemoembolization for HCC. Cardiovasc Intervent Radiol 41(11):1699–1707. https://doi.org/10.1007/s00270-018-1978-0
Cannon R, Ellis S, Hayes D, Narayanan G, Martin RCG (2013) Safety and early efficacy of irreversible electroporation for hepatic tumors in proximity to vital structures. J Surg Oncol. 107(5):544–9
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly to finishing this work; all authors agree with the content of the manuscript. Design of the study: Magdy El-Serafy, Mohamed Hassany. Performance of management: Mohamed Hassany, Wessam Mostafa, Hossam Debian. Acquisition of data: Ahmed Mostafa Mahboub. Analysis of data: Ahmed Mostafa Mahboub, Wessam Mostafa, Hossam Debian. Interpretation of data and drafting of the article: Ahmed Mostafa Mahboub, Hend Ibrahim Shousha. Article revision: Mohamed Hassany, Ahmed Mostafa Mahboub, Wessam Mostafa, Hossam Debian, Hend Ibrahim Shousha, Magdy El-Serafy. Final approval of the version: Magdy El-Serafy. Article submission: Hend Ibrahim Shousha.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients signed a written informed consent before inclusion in the study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This study was carried out following the 1975 Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments and its later amendments. The protocol of this study was approved by the ethics committee of the Faculty of Medicine, Cairo University (Number: N-46–2017).
Consent for publication
N/A.
Competing interests
The authors do not have a commercial or any association that might pose a conflict of interest (e.g., pharmaceutical stock ownership, consultancy, advisory board membership, relevant patents, or research funding).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Submission declaration
This work has not been published previously, is not under consideration for publication elsewhere, its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out and, if accepted, will not be published elsewhere including electronically in the same form, in English or any other language, without the written consent of the copyright holder.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hassany, M., Mahboub, A.M., Mostafa, W. et al. Assessment of efficacy and safety of irreversible electroporation versus TACE for treatment of difficult location hepatocellular carcinoma. Egypt Liver Journal 14, 33 (2024). https://doi.org/10.1186/s43066-024-00338-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-024-00338-3