Abstract
Background
Natural bioactive components derived from plant secondary metabolites have been pronounced as valuable alternatives for anticipating and subsiding hepatotoxic effects and its chronic complications based on experimental verification. The focus of this review is to elucidate the commonly used modern medicine for the treatment of liver disease and how major phytoconstituents have been tested for hepatoprotective activity, mechanism of action of some promising agents from natural sources, and clinical trial data for treating in patients with different liver diseases by the aid of natural phytoconstituents.
Main text
The review shows fifteen major isolated phytoconstituents, their biological sources, chemical structures, utilized plant parts, type of extracts used, hepatoprotective assay method, and their possible mechanism of action on the hepatoprotection. Nine promising hepatoprotective leads from natural sources with their chemistry and hepatoprotective mechanism are mentioned briefly. The review further includes the recent clinical trial studies of some hepatoprotective leads and their clinical outcome with different liver disease patients. Scientific studies revealed that antioxidant properties are the central mechanism for the phytoconstituents to subside different disease pathways by upsurging antioxidant defense system of cells, scavenging free radicals, down surging lipid peroxidation, improving anti-inflammatory potential, and further protecting the hepatic cell injury. In this review, we summarize recent development of natural product-based hepatoprotective leads and their curative potential for various sort of liver diseases. Furthermore, the usefulness of hit and lead molecules from natural sources for significant clinical benefit to discover new drug molecule and downsizing the problems of medication and chemical-induced hepatotoxic effects is extrapolated.
Conclusion
Further research are encouraged to elucidate the pharmacological principle of these natural-based chemical agents which will stimulate future pharmaceutical development of therapeutically beneficial hepatoprotective regimens.
Similar content being viewed by others
Introduction
The liver, largest organ in human body, contributes 2% of our body weight, weighing almost 1.5 kg in a fully grown adult [57]. The liver is the site for drug metabolism and biotransformation, thereby having defensive role in the body against toxic foreign chemical agents. Due to these, the liver is exposed to drugs, chemicals, and other xenobiotics in different concentrations which finally results in liver injury. There are over hundreds of etiology causing hepatic diseases. The most profound causes of hepatic disease consist of microbes (hepatitis virus A, B, C,Cytomegalovirus, Epstein-Barr virus, and yellow fever virus); disease related to metabolic syndrome (fatty liver disease caused by obesity, hemochromatosis, and Wilson’s disease); xenobiotics (alcohol, drugs, and chemicals); hereditary-related hepatic diseases; autoimmune diseases (biliary cirrhosis, hepatitis, and sclerosing cholangitis); and liver malignancies [75]. End result of hepatic diseases is disturbance and loss of workdays, compensation in quality of personal life, squeezing in expected life span, and financial burden to the individual as well as to the society, subsequently resulting in mortality and morbidity.
Around the globe, near to 2 million people are fading away each year because of hepatic complexities among which 1 million are due to complication of cirrhosis and another half are cognated to liver carcinoma and viral hepatitis [60, 107]. At present, the most prevalent cause of death is cirrhosis ranking 11 (1.16 million deaths) and liver cancer which ranks 16 (788,000 deaths) for death complication, and in combination, they account for 3.5% of all deaths worldwide [54, 107]. High intake of alcoholic product is the major factor for liver disease in global context [142]. A report published by the World Health Organization showed that among the total alcohol consumer worldwide which is predicted to be around 2 billion, slightly less than half, i.e., 75 million, are diagnosed with disorders related to the alcohol use specifically to several alcohol-associated liver disease [11, 181]. In 2015, more people died with viral hepatitis-related disease (1.34 million deaths) than by human immunodeficiency virus (HIV) (1.06 million deaths) or malaria (0.44 million deaths) and similar to the number caused by tuberculosis (1.37 million) [154, 178]. Among the morbidity cause by viral hepatitis, total of 96% is accounted for hepatitis B virus (66%) and hepatitis C virus (30%) which is mainly due to the cirrhosis complication and profusion of liver cancer [154].
Drug-induced liver injury (DILI) is one of the major problems associated with the treatment for several acute and chronic disease conditions. Research studies revealed that antitubercular drug (isoniazid), antipsychotic (chlorpromazine), penicillin antibiotic (amoxicillin), and histamine antagonist (cimetidine), analgesic and antipyretic (acetaminophen), and HMG-CoA reductase inhibitors (statins) are major drugs causing DILI [15, 143]. In West region of the globe, amoxicillin/clavulanic acid-induced liver injury occurs in 1 in 2350 [17], whereas combined antitubercular drug-induced liver injury is more profound in the east region [22, 198]. Among them, India and Nigeria have highest burden of DILI followed by China and South Korea having herbal and alternative medicine-induced liver injury [34, 156], WHO [179]. Globally, antimicrobial agents are considered as the major cause of idiosyncratic DILI [33, 170, 201]. The above latest figures depict that the worldwide liver disease burden has increased with growing time showing massive influence on the public life around the globe WHO [
Traditional medicine is prevalent all over the world which plays important role for preventive and curative purpose for people in developing countries [31]. According to the definition given by the WHO, “Traditional medicine is regarded as diverse health practices, approaches, knowledge and beliefs incorporating plant, animal, and/or mineral based medicine, spiritual therapies, manual techniques and exercises applied singularly or in combination to maintain well-being, as well as to treat, diagnose or prevent illness” [196].
Hepatic problems are one of the highly pronounced reason for mortality and morbidity in human [109, 114]. Liver damage is usually related to cell necrosis, diminution, and increase of liver biomarkers such as aspartate aminotransferase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), total bilirubin (TB), total protein (TP), an increase in tissue lipid per oxidation, and oxidative damage [36, 100]. Traditional medicine from the natural sources has significant effect in the management of the hepatic diseases. Many natural phytoconstituents have been demonstrated to be effective hepatoprotective agents, while many more are claimed to have hepatoprotective and hepatocurative activity. Natural product-based phytoconstituents are regarded as the best and most validated source for developing novel therapeutic agents, but poor absorption, distribution, metabolism, and elimination followed by few toxicological properties still restrain the wide utilization of them for therapeutic purpose. In the last couple of decades, researcher and scientist are more encouraged for finding out more promising hepatoprotective agents from plant source to develop novel modern medicine for different liver aliments [61, 161].
In view of these facts, this review is effort to evaluate the available proven scientific data on the following:
-
(i)
Recently developed modern medicines for liver disorder
-
(ii)
Major phytoconstituents from the natural sources with their hepatoprotective activity
-
(iii)
Promising hepatoprotective agents from the natural sources with its mechanism of action
-
(iv)
Clinical trial data of some promising hepatoprotective leads in patients with different liver diseases
-
(v)
Common mechanism of action of natural product-based leads for the protection against different liver diseases
Review method
The information about liver disease, clinical trial of recent hepatoprotective leads, promising hepatoprotective agents, and specific phytoconstituents was gathered by systematic literature survey with reference to the publications published mostly from 2000 to 2022. A comprehensive systematic literature survey was carried out in different scientific search engines such as Google Scholar, Wiley, PubMed, Taylor & Francis, ScienceDirect, and Springer to find required information. Major keywords used to search and to retrieve the related articles are "Liver disease," "Hepatoprotective," "Hepatoprotective AND Plant," "Hepatoprotective AND Herbal," "Hepatoprotective AND Natural Product," "Hepatotoxicity," "Hepatotoxicity AND Ethnopharmacology," and so forth.
Results
Some clinical significance of allopathic drugs for liver disorder
Due to the recent advancement, medication evaluation based on evidence, standard pharmacopeia, and randomized placebo control clinical trial to outline the clinical efficacy of modern medicine is more frequent. Therapies developed with synthetic hit and lead compounds relying in the principle of allopathic medicine have significant risk–benefit ratio, often expensive and less effective [117, 163]. Some liver-protective medicines and their adverse effects are depicted in Table 1 below.
Major bioactive phytochemicals with hepatoprotective activity
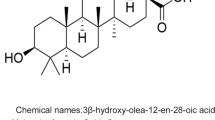
Active hepatoprotective phytoconstituents discovered in experimental laboratory mouse model during the experiment in mouse with different liver diseases are mentioned in Tables 1 and 2. Their chemical structures are illustrated in Fig. 1.
Some promising hepatoprotective agents from natural sources
Silymarin (family: Asteraceae)
Silymarin, an active compound of Silybum marianum (L.) Gaertn., commonly known as “milk thistle,” is one of the oldest plant which has been commonly utilized for the treatment of liver diseases [90, 102].
Dried seeds are major sources of active phytoconstituents, which contain four flavonolignans isomer, i.e., silybin, isosilybin, silydianin, and silychristin. The complex mixture of these four flavonolignans isomer is known as silymarin [47, 73].
Silymarin shows hepatoprotection via various underlying mechanisms of which most common are modulation of enzymatic and nonenzymatic liver biochemical markers [170, 173] and induction of nuclear factor-erythroid 2-related factor 2 (Nrf2) expression [70]. In addition, anti-inflammatory properties of silymarin have been proved in several models of liver damage. In rats, with alcoholic fatty liver model, silymarin acted by downregulating the expression of nuclear factor kappa B (NF-κB), interleukin-6 (IL-6), mission mode project-2 (MMP-2), mission mode project-13 (MMP-13), transforming growth factor beta-1 (TGF-β1), tumor-suppressor Krueppel-like factor, collagen α1 expression, and platelet-derived growth factor (PDGF) signaling when tested in hepatotoxic damage animal models [30, 194]. Likewise, silymarin could inhibit cells infected by HCV via TNF-α-induced activation of NF-κB and its nuclear translocation [104, 131]. Silymarin is well tolerated by patients with good safety profile [132]. Poor water solubility of silymarin is being overcame by silymarin-loaded solid nanoparticles which enhance its antioxidant and hepatoprotective activity in comparison with crude silymarin [20].
Glycyrrhizin (family: Leguminacae)
Glycyrrhizin, a triterpenoid glycoside isolated from the root of Glycyrrhiza glabra L. commonly known as liquorice root, has been used in traditional medicine system of Nepal, India, China, and other countries for the treatment of jaundice [121, 186]. It is a mixture of potassium and calcium salt of glycyrrhizinic acid, and other phytoconstituents involved are glycyrrhetinic acid, beta-sitosterol, hydroxycoumarins, and flavonoids [50, 147].
Glycyrrhizin shows hepatoprotective effect via various mechanisms such as increasing antioxidant defense in hepatic cell and as anti-inflammatory agent [121, 147]. High-mobility group protein box (HMGB1) are either diminished or interrupted for binding to glutathione S-transferase omega-1 (GSTO1) promoter region by glycyrrhizin to show anti-inflammatory effect [74, 93]. Not only glycyrrhizin, its metabolite, and glycyrrhetinic acid inhibited collagen αI(I) gene expression in liver fibrosis caused by CCl4 [110]. Glycyrrhetinic acid also helps in liver cell growth through the mechanism of epithelial growth factor receptor (EGFR) binding, stimulating DNA synthesis in liver cells by extracellular signal-regulated kinases (ERK2)-mediated pathway [25, 71], which helps in liver regeneration. During interferon alpha (IFN-α)-based therapy failure, glycyrrhizin administered through intravenous route dramatically lowered the serum alanine transaminase level after 12 weeks of therapy and improved liver fibrosis and necrosis caused by inflammation after 52-week treatment in patients with hepatic disease [97]. Moreover, it is also effective in prevention of HCV-related liver cirrhosis in older patients [62, 106]. In a study using in vitro cell model and in vivo animal models with hepatic injury, it was revealed that 18β-glycyrrhetinic acid reduces oxidative stress and expression of inflammatory markers which were predicted as a result of the downregulation of NF-κB and upregulation of Nrf2 target genes [59, 87].
Andrographolide and neoandrographolide (family: Acanthaceae)
Andrographolide and neoandrographolide are the active chemical constituents of herbaceous plant of Andrographis paniculata Nees. commonly known as “king of bitters” due to its extremely bitter taste and is well-known for liver diseases [134, 172].
The main active chemical constituent is diterpene lactone class which is obtained from the leaves, i.e., neoandrographolide, 14-deoxy-11-dehydroandrographolide, 14-deoxy-11-oxoandrographolide and deoxy-andrographolide, andrographolide, andrographine, panicoline, paniculide-A, paniculide-B, and paniculide-C [129, 136].
Andrographolide inhibits inflammation, angiogenesis, and fibrosis in chemically induced liver injury animal model via antioxidant and anti-inflammatory mechanisms [26, 77]. Oxidative stress-inducible gene such as hypoxia-inducible factor-1 alpha, superoxide dismutase (SOD-1), heme oxygenase-1 (HO-1), and glutathione S-transferase (GST1) which uprise nuclear Nrf2 content and its DNA-binding activity and other upregulated protein and gene are balanced by andrographolide [26, 187]. It also helps in upregulation of HO-1 via the p38 mitogen-activated protein kinase, MAPK/Nrf2 pathway shows anti-HCV activity [77]. Additionally, andrographolide helps in downregulation of hypoxia-inducible genes such as vascular endothelial growth factor (VEGF) and also diminishes TNF-α and cycloxygenase-2 (COX-2) expression and finally reduces liver hypoxia and attenuates hepatic apoptosis and fibrosis in rats [72, 79]. The compound decreases serum levels of TNF-α and interleukin-1 beta (IL-1β) and hepatic expression of TGF-β, cannabinoid receptor type 1 (CBR1), and Bax. The predicted mechanism for the decrement of serum levels of TNF-α and IL-1β is through the downregulation of JNK and ERK phosphorylation. A study in high-fat diet (HFD) fed mice administering andrographolide showed that cellular lipid accumulation is diminished [37, 79].
Picroside I and kutkoside (family: Scrophulariaceae)
Picroside and kutkoside are the active chemical constituents of roots and rhizomes of Picrorhiza kurroa Royle, commonly known as “Kutki” or “Kutaki,” and have been used to treat hepatic disorder since long [58, 140].
The major active constituents are kurkoside, apocynin, drosin, cucurbitacin glycoside, and the iridoid glycoside such as picroside 1, 2, and 3. Kutkin is formed when picroside I and kutkoside are mixed in the ratio of 1:2 [141, 152].
Picroside-I and kutkoside show hepatoprotective effect via membrane stabilizing, hypolipidemic and antioxidant properties, and finally liver regenerative effect in rats via stimulation of nucleic acid and protein synthesis [101, 139, 153]. Picroside-I and kutkoside are free radical scavengers (superoxide anion O2•) and inhibit lipid peroxidation in liver tissue [95]. It also showed restoration of bilirubin and activity of serum liver biomarkers level of AST, ALT, ALP, and LDH against acetaminophen-induced liver toxicity animal model by protecting injury hepatocyte proving its hepatoprotective effect [141]. Moreover, picroside also reduces the lipid peroxidation, normalizes glutathione metabolism, and inhibits hepatocarcinogenesis caused by N-nitrosodiethylamine in rats by increasing the life span of tumor bearing rats [24, 195]. It acts against less expression of LDL receptor on cell surface caused by paracetamol and uprises the conjugated dienes in liver cells as well as maintain of oxidation–reduction balance for healthy liver [108, 152].
Curcumin (family: Zingiberaceae)
Curcumin is the principle curcuminoid found in rhizome of Curcuma longa commonly known as “turmeric.” Traditional use of turmeric for the treatment of bilirubin-related liver disease such as jaundice and several other hepatic complication is being documented since long [81].
Structurally, similar phenolic compounds found in the rhizomes of turmeric are known as curcuminoids in their mixed form. Three major curcuminoids present in rhizomes of turmeric are curcumin, demethoxycurcumin, and bisdemethoxycurcumin. Chemically, curcumin is a diferuloylmethane which consists of diferulic acid moiety fused with methylene moiety or other carbon group and exists mainly in keto-enol form [83, 130].
Hepatoprotection mechanism of the curcumin may be due to its antioxidant activity and activation of the phase 2 detoxifying/antioxidant enzymes such as HO-1 and NADPH quinone oxidoreductase-1 (NQO1) and Nrf2/Kelch-like ECH-associated protein 1 (Keap1)/antioxidant-responsive element (ARE) pathway [43, 48]. In addition, its administration in diet reduces oxidative stress, decreases Cytochrome P450 2E1 (CYP2E1) and paired-related homeobox 1 (Prx1) expression, while upregulates paired-related homeobox 6 (Prx6) expression [78]. Oxidative stress caused by hepatotoxins is closely associated with activation of some inflammatory mediators such as MAPKs, NF-κB, and signal transducer and activator of transcription-3 (STAT3) via different pathways [5]. Research reported that curcumin can inhibit the expression of toll-like receptor-2 (TLR2), toll-like receptor-4 (TLR4), and HMGB1 in rat suffered with fibrogenesis expression of ligand molecules. Concanavalin A-induced hepatitis in mice via T-cell-mediated pathway become less severe when administered with curcumin which is mainly due to the inhibition of liver inflammation [167, 168]. Likewise, curcumin could diminish liver toxicity cause by lipopolysaccharide (LPS)/D-galactosamine (D-GalN) through inhibition of hepatic mRNA levels of Sirtuin (silent mating type information regulation 2 homolog)-1 (SIRT1) [190]. It also suppresses expression of gene for receptors which are involved in final product of advanced glycation in hepatic stellate cells (HSCs) by uprising the peroxisome proliferator-activated receptor-gamma (PPARγ) activity and subsiding oxidative stress [86]. Moreover, curcumin could protect against paracetamol-induced hepatocyte apoptosis by reducing the availability of proapoptotic genes Bax and caspase-3 while improving antiapoptotic genes [80]. However, curcumin is able to downregulate Bcl-2 mRNA expression and upregulates p53 protein expression in thioacetamide-induced cytotoxicity, facilitating apoptosis in damaged cells which reduces hepatic inflammatory gene and fibrogenesis [174]. Additionally, antioxidant and anti-inflammatory effect of curcumin could protect mice against human cytomegalovirus infection [92].
Phyllanthin and hypophyllanthin (family: Euphorbiaceae)
Phyllanthin is a potent hepatoprotective lignans found in Phyllanthus niruri Linn., commonly known as “gale of the wind,” is a long established herbal remedy for jaundice and other hepatic diseases [50].
The main active chemical constituents include alkaloids, astragalin, brevifolin, ellagitannins, amariin, repandusinic acid, phyllanthusiin D gallocatechins, geraniin, hypophylanthis, lignans, nirutin, phyllanthin, and phyllanthenol. Chemically, phyllanthin and hypophyllanthin are lignans isolated from the hexane extract and have been established as the hepatoprotective agents [58, 83].
Phyllanthus niruri is effective against infective hepatitis and other liver disease [65, 76]. Ethanolic extract of this plant possesses potent hepatoprotective activity both in vitro and in vivo. In India, it was used to treat jaundice in children because of its liver-protective and detoxifying action [38, 52]. A study in the UK revealed that Phyllanthus extract could be effective for treatment of both acute and chronic hepatitis in children [38, 76]. Phyllanthin and hypophyllanthin both can protect rat liver from toxicity induced by carbon tetrachloride and cytotoxicity induced by galactosamine [7, 158].
These lignans also protect against liver damage induced by alcohol and normalize a “fatty liver” condition. The hepatoprotective effects of phyllanthus lignin are achieved with the mechanism of inhibition of superoxide and hydroxyl radicals and lipid peroxidation [16, 67].
Berberine (family: Berberidaceae)
Berberine is an isoquinoline alkaloid which could be isolated from roots, rhizomes, and stem bark of Berberis aristata DC, commonly known as “barberry” and has been used as tonic remedy for liver since long ago [98].
The major active chemical constituents present in Berberis aristata are berberine, oxyberberine, berbamine, aromoline, karachine, and oxycanthine. Berberine is experimentally proved hepatoprotective phytoconstituent [63, 96].
Berberine shows antioxidant activity which could suppress oxidative stress and attenuates apoptosis through the increment of ratio of Bcl-2/Bax in ischemia-/reperfusion-injured rat liver inhibiting caspase-3 cleavage in the liver [123]. Its mechanism of action is upregulation of Akt and inhibition of mTOR expression [146]. Furthermore, hepatocyte nuclear factor-4 alpha and PPARα/peroxisome proliferator-activated receptor-gamma coactivator 1-alpha (PGC-1α) could be restored with berberine showing hepatoprotective effect in liver ischemia. Experiment in mice with steatosis induced by ethanol showed that berberine protects the liver from ethanol-induced oxidative stress [193]. Berberine even reduces the expression of hepatic proprotein convertase subtilisin/kexin type 9 (PCSK9), a cholesterol homeostasis regulator, and decreases IFN-γ, TNF-α, IL-1α and 8-isoprostane levels in LPS-induced hepatoxicity mouse model [180]. Carbon tetrachloride-induced liver injury is attenuated by berberine via suppression of TNF-α, COX-2, and iNOS expression and oxidative stress [39]. Berberine could diminish liver fibrosis through the activation of AMPK and decreasing the expression of NOX4 and phosphorylated Akt [82].
Embelin (family: Myrsinaceae)
Embelin, chemically known as “2,5-dihydroxy-3-undecyl-1,4-benzoquinone,” is an active chemical constituent of leaves of Embelia ribes Burm.f. commonly known as “false black pepper” and is known for free radical scavenging and liver protective function [66]. The active constituents are embelin, christembine, quercitol, and resin. Embelin shows its hepatoprotective effect mainly through its free radical scavenging and lipid peroxidation pathway. Embelin can control the liver biomarkers: AST, ALT, ALP, LDH, bilirubin γ-glutamyl transpeptidase, and total protein levels in carbon tetrachloride-treated rats [150]. Study in mitochondria of rat liver showed that embelin could inhibit lipid peroxidation, and impaired superoxide dismutase level was restored with embelin administration. Furthermore, to extraplot mechanism and rate of reactions of embelin with hydroxyl, way of oxidizing single electron and radical called “organo-haloperoxyl” with the technique known as nanosecond pulse radiolysis was studied. Its redox potential was also evaluated, and the study depicted that embelin is a potent-free radical scavenger in physiological conditions [35, 66].
Resveratrol
Resveratrol chemically known as “trans-3,5,4′-trihydroxystilbene” is a naturally occurring polyphenol compound present in Vitis labrusca commonly known as “grapes,” Vaccinium myrtillus L. commonly known as “blueberries” and Rubus idaeus L. commonly known as “raspberries” with potent antioxidant properties. Resveratrol, a phytoalexin, is generated in plants when bacteria and fungi attacked it [32].
Resveratrol shows liver protection via reduction of oxidative stress during hepatocyte injury by modifying the expression of nuclear transcription factors Nrf2 and NF-κB and downregulating HO-1 and iONS gene expression [1, 144]. This enhances the free radical scavenging properties as well as phase 2 enzymes [21]. Furthermore, it even inhibits proinflammatory cytokines such as IL-2, IL-6, and TNF-α in concanavalin A-induced autoimmune hepatitis [199]. In liver injury cause by high cholesterol, resveratrol shows protective effect which is mediated by the enhancement of autophagy and downregulation of proapoptotic proteins such as Bax and caspase-3 and caspase-8 [23]. Followingly, hepatotoxicity caused by isoniazid and rifampicin is ameliorated by resveratrol by modulating the expression of SIRT1 mRNA hepatic cells of mice, which finally minimize hepatic oxidative stress in the liver, production of cytokine, and expression of gene called PPARγ [119]. Moreover, resveratrol also prevents hepatotoxicity resulted from higher consumption of acetaminophen by upregulating expression of SIRT1 and downregulating p53 signaling, enhancing the expression of cell nuclear antigen, promoting hepatic cell proliferation, enhancing liver regeneration and inducing uprising the level of cyclin D1 and Cdk4 [53, 176].
Clinical trials of some hepatoprotective leads
During the drug development phase of the clinical trials, potent hepatoprotective phytoconstituents are studied in different human liver disease condition with specified period to curing the liver disease. The summary of the reported clinical trials of major hepatoprotective leads is documented in Table 3.
Possible best mechanism of herbal remedy for the protection of liver against variety of toxins and injury
The study revealed that the most profound hepatoprotective mechanisms of the herbal plants are through the free radical scavenging effect and anti-inflammatory pathway. The hepatic injury perpetually involves per oxidation of fatty acid present in hepatocyte membrane leading to the distortion of the cells and their organelles. Recent studies suggested that oxidative stress has a vital role in the commencement and development of hepatic damage. Role of oxidative stress in viral hepatitis and in liver diseases caused by autoimmune syndrome has been studied and reported significantly [42]. Furthermore, xenobiotics and toxic chemicals damage hepatic cells mainly by the generation of reactive free radicals which form covalent bonding interaction with the amino acid residue of the hepatic cell membranes (Fig. 2). Due to widespread contact to harmful chemicals, sometimes the produced free radicals override the defensive system available naturally causing hepatic injury. Natural phytoconstituents such a vitamin E and silymarin are known for their protective role against liver injury caused by hepatotoxic agent [197]. Inflammation which is the major clinical symptom in hepatotoxin-induced liver damage is cause by toxin or through oxidative stress which leads towards the noteworthy increment of proinflammatory cytokines including TNF-α (tumor necrosis factor-α) and IL-6 (interlukin-6) and hepatocyte inflammation [2]. In brief, minimizing the oxidative stress and inflammatory cytokines is the major mechanism by which herbal remedies act as hepatoprotectant.
The mechanism by which herbal remedies protect against liver injury from different toxins and injurious stimuli [3]
Discussion
Global use of herb-based regimen is increasing day by day, and at least one-quarter of patients with liver diseases use natural phytoconstituents for disease therapy. Current research strategies are focused on scientific investigation of herbal-based medicine for their safety and efficacy through huge preclinical studies followed by clinical trials to find the mysteries hidden in medicinal plants [51]. Such approaches ultimately help to find the real potent therapeutic lead and valuable pharmacotherapeutic candidate from the natural sources specially plant origin and standardize the dosage regimen on scientific-based finding [135]. Recently, most of the herbal products are marketed for the purpose of disease prevention, support health, relieve symptoms, and curing of different disease and aliments. Still most of these products lack scientific and pharmacological validation. Most of the experimental model study related to hepatotoxicity using cell culture and animals showed that various plant extracts exert hepatoprotective and curative effects which further assist in clinical testing for discovery of hepatoprotective leads. Due to lack of scientific‑based pharmacological data, most of the herbal-based formulations cannot be recommended for the treatment of liver diseases [155].
This review gives the clear idea that herbal-based therapy could play a significant role against various liver disorder and disease condition occurring in human. Several herbs from natural sources and plant extracts have measurable hepatoprotective effect in several experimental animal models. Secondary metabolites such as alkaloid, flavonoids, phenolic, tannins, lignins, and resin-based compound are the major active phytocontituents for hepatoprotective effect [9]. The significant portion of the study depicts that extracts of different parts of medicinal plants have potentials to subside hepatic disorder Baral et al. [14]. In addition, this study highlighted scientific evidence and mechanism of hepatoprotection by crude extracts of medicinal plants. The most probable mechanism of action of several plant extracts is through the scavenging effect of harmful free radical generated during infirmities. Several experiments in vivo study showed that phenolic and flavonoid constituents of plant extracts help to upsurge the decrease proportion of blood glutathione, to enhance protein secretion, to minimize lipid peroxidation and to enhance free radical scavenging properties. Furthermore, phytoconstituents lower the hepatic enzymes such as AST, ALT, ALP and arginase and enhance the level of total bilirubin in blood plasma,upsurge antioxidative enzymes such as SOD, GPx, CAT and GST,and lower MDA level [41]. In a nutshell, it could be highlighted that herbal drug possesses significant hepatoprotective properties which could be proved by various preclinical and clinical studies.
Conclusion and future perspective
To recapitulate, numerous research in last few decades have clearly established that herbal lead compounds have significant hepatic injury; the major mechanism for protection of liver cells is eradication of free radicals, reducing oxidative stress and decreasing the proinflammatory cytokine mediators in the body. This ample review will be helpful to begin a new way and to explore additional clinical application of bioactive constituents as liver-protective agents. Significant natural availability and economic and minimum side effect as compared to allopathic medicine have encouraged utilization of bioactive compounds for the treatment of liver disease. Followingly, subsequent preclinical investigations have been directed, and such studies have already proved several remedies as hepatoprotective agents, and further clinical trials are on demand for authentication. Several in silico studies and compounds from molecular networking have also suggested active phytoconstituents from natural sources as possible hepatoprotective agents. In addition, it is a proper time to uncover the possibility of hepatoprotection potential of new bioactive compounds for human health either through in silico methods such as molecular docking, machine learning, and deep learning or through biophysical and biochemical experimental techniques. Finally, in this review, an attempt has been made to compile the reported hepatoprotective plants and their active phytoconstituents around the globe. These phytoconstituents are claimed to have proved benefit for health professionals, scientists, and scholars working in the field of pharmacology, therapeutics, and pharmacognosy to develop evidence-based alternative medicines to cure different kinds of liver diseases for mankind. This study paved a marvelous path for further scientific validation, research, and investigation to understand the therapeutic potential of these natural lead constituents to discover novel hepatoprotective therapeutics from natural source.
The point is not that natural products will solve all problems. It is that a lot of problems are not being solved because natural products are not being examined.
S. J. Gould, Chem. Eng. News 13 October 2003, p 103
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- Akt:
-
Enzyme type of serine/threonine protein kinase
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine transaminase
- AMPK:
-
AMP-activated protein kinase
- ARE:
-
Antioxidant-responsive element
- AST:
-
Aspartate aminotransferase
- Bcl-xL:
-
B-cell lymphoma-extra large
- CAT:
-
Catalase
- Cdk4:
-
Cyclin-dependent kinase 4
- COX-2:
-
Cycloxygenase-2
- CYP2E1:
-
Cytochrome P450 2E1
- ERK2:
-
Extracellular signal-regulated kinase
- EGFR:
-
Epithelial growth factor receptor
- GGT:
-
Gamma-glutamyl transferase
- GPx:
-
Glutathione peroxidase
- GR:
-
Glutathione reductase
- GSH:
-
Glutathione
- GST-1:
-
Glutathione S-transferase
- GSTO1:
-
Glutathione transferase omega 1
- HAT:
-
Histone acetyltransferase
- HDAC2:
-
Histone deacetylase-2
- HCV:
-
Hepatitis C virus
- HFD:
-
High-fat diet
- HMBG1:
-
High mobility group box 1
- HO-1:
-
Heme oxygenase-1
- HSCs:
-
Hepatic stellate cells (HSCs)
- IFN:
-
Interferon
- IL-6:
-
Interleukin-6
- IL-1β:
-
Interleukin-1β
- JNK:
-
Jun N-terminal kinase
- LDH:
-
Lactate dehydrogenase
- LPO:
-
Lipid peroxidation
- LPS/D-GalN:
-
Lipopolysaccharide/D-galactosamine
- MAPK:
-
Mitogen-activated protein kinase
- MDA:
-
Malonaldehyde
- MMP:
-
Mission mode project
- NF-κB:
-
Nuclear factor kappa B
- Nrf2:
-
Nuclear factor erythroid 2-related factor 2
- NQO1:
-
NADPH quinone oxidoreductase-1
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- PGC-1α:
-
Peroxisome proliferator-activated receptor-gamma coactivator 1-alpha
- PDGF:
-
Platelet-derived growth factor
- Prx:
-
Paired-related homeobox
- SIRT1:
-
Sirtuin 1
- SOD:
-
Superoxide dismutase
- STAT3:
-
Signal transducer and activator of transcription 3
- TB:
-
Total bilirubin
- TGF-β1:
-
Transforming growth factor beta
- TLR:
-
Toll-like receptor
- VEGF:
-
Vascular endothelial growth factor
References
Ahmad A, Ahmad R (2014) Resveratrol mitigate structural changes and hepatic stellate cell activation in N’-nitrosodimethylamine-induced liver fibrosis via restraining oxidative damage. Chem Biol Interact 221:1–12
Al-Amarat W, Abukhalil MH, Alruhaimi RS, Alqhtani HA, Aldawood N, Alfwuaires MA, Althunibat OY, Aladaileh SH, Algefare AI, Alanezi AA (2022) Upregulation of Nrf2/HO-1 signaling and attenuation of oxidative stress, inflammation, and cell death mediate the protective effect of apigenin against cyclophosphamide hepatotoxicity. Metabolites 12:648
Al-Asmari AK, Al-Elaiwi AM, Athar MT, Tariq M, Al Eid A, Al-Asmary SM (2014) A review of hepatoprotective plants used in Saudi traditional medicine. Ev-Based Complement Altern Med 2014:1-22
Al-Snai A, Mousa H, Majid WJ (2019) Medicinal plants possessed hepatoprotective activity. IOSR J Pharmacy 9:26–56
Ambade A, Mandrekar P (2012) Oxidative stress and inflammation: essential partners in alcoholic liver disease. Int J Hepatol 853175:1
Antarkar D (1980) A double-blind clinical trial of Arogya-wardhani-an Ayurvedic drug-in acute viral hepatitis. Indian J Med Res 72:588–593
Antunes C, Arbo MD, Konrath EL (2022) Hepatoprotective native plants documented in Brazilian traditional medicine literature: current knowledge and prospects. Chem Biodivers 19:e202100933
Arteel G, Marsano L, Mendez C, Bentley F, Mcclain CJ (2003) Advances in alcoholic liver disease. Best Pract Res Clin Gastroenterol 17:625–647
Arya AK, Durgapal M, Bachheti A, Joshi KK, Gonfa YH, Bachheti RK, Husen A (2022) Ethnomedicinal use, phytochemistry, and other potential application of aquatic and semiaquatic medicinal plants. Evid-Based Complement Altern Med Rev 2022:1-19
Asgarshirazi M, Shariat M, Sheikh M (2017) Comparison of efficacy of folic acid and silymarin in the management of antiepileptic drug induced liver injury: a randomized clinical trial. Hepatobiliary Pancreat Dis Int 16:296–302
Asharani P, Karuvetil MZ, Brian TYW, Satghare P, Roystonn K, Peizhi W, Cetty L, Zainuldin NA, Subramaniam M (2022) Prevalence and correlates of physical comorbidities in alcohol use disorder (AUD): a pilot study in treatment-seeking population. Int J Ment Health Addict 1–18.
Baghbahadorani FK, Miraj S (2016) The impact of silymarin on improvement of platelet abnormalities in patients with severe preeclampsia. Electron Physician 8:2436
Bandopadhyay S, Mandal S, Ghorai M, Jha NK, Kumar M, Ghosh A, Proćków J, Pérez De La Lastra JM, Dey A (2023) Therapeutic properties and pharmacological activities of asiaticoside and madecassoside: a review. J Cell Mol Med 27:593-608
Baral R, Karki A, Karki S, Neupane B, Koirala P, Baral S, Panta S (2021) Phytochemical screening, free radical scavenging, and in-vitro anti-bacterial activity study of chloroform, acetone and methanol extracts of selected medicinal plants of Nepal. Curr Perspect Med Aromatic Plants 4:22–35
Benić MS, Nežić L, Vujić-Aleksić V, Mititelu-Tartau L (2022) Novel therapies for the treatment of drug-induced liver injury: a systematic review. Front Pharmacol 12:785790
Bhattacharjee R, Sil PC (2007) Protein isolate from the herb, Phyllanthus niruri L. (Euphorbiaceae), plays hepatoprotective role against carbon tetrachloride induced liver damage via its antioxidant properties. Food Chem Toxicol 45:817–826
Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S (2013) Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 144:1419–1425. e1413
Bunout D, Hirsch S, Petermann M, De La Maza M, Silva G, Kelly M, Ugarte G, Iturriaga H (1992) Controlled study of the effect of silymarin on alcoholic liver disease. Rev Med Chil 120:1370–1375
Cai L, Wu Y, Zhan J (2012) Comparison of the efficacy of two glycyrrhizin preparations in the treatment of chronic hepatitis B. J Pharmaceut Epidemiol 21:160–161
Cengiz M, Kutlu HM, Burukoglu DD, Ayhancı A (2015) A comparative study on the therapeutic effects of silymarin and silymarin-loaded solid lipid nanoparticles on D-GaIN/TNF-α-induced liver damage in Balb/c mice. Food Chem Toxicol 77:93–100
Cerný D, Canová NK, Martínek J, Horínek A, Kmonícková E, Zídek Z, Farghali H (2009) Effects of resveratrol pretreatment on tert-butylhydroperoxide induced hepatocyte toxicity in immobilized perifused hepatocytes: involvement of inducible nitric oxide synthase and hemoxygenase-1. Nitric Oxide 20:1–8
Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, Watkins PB, Navarro V, Barnhart H (2015) Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology 148:1340–1352. e1347.
Chan CC, Lee KC, Huang YH, Chou CK, Lin HC, Lee FY (2014) Regulation by resveratrol of the cellular factors mediating liver damage and regeneration after acute toxic liver injury. J Gastroenterol Hepatol 29:603–613
Chander R, Kapoor NK, Dhawan BN (1992) Effect of picroliv on glutathione metabolism in liver and brain of Mastomys natalensis infected with Plasmodium berghei. Indian J Exp Biol 30:711–714
Chen G, Bei B, Feng Y, Li X, Jiang Z, Si J-Y, Qing D-G, Zhang J, Li N (2019) Glycyrrhetinic acid maintains intestinal homeostasis via HuR. Front Pharmacol 10:535
Chen H-W, Huang C-S, Li C-C, Lin A-H, Huang Y-J, Wang T-S, Yao H-T, Lii C-K (2014) Bioavailability of andrographolide and protection against carbon tetrachloride-induced oxidative damage in rats. Toxicol Appl Pharmacol 280:1–9
Chen Q-Y, Huang X-B, Zhao Y-J, Wang H-G, Wang J-B, Liu L-C, Wang L-Q, Zhong Q, Xie J-W, Lin J-X (2022) The peroxisome proliferator-activated receptor agonist rosiglitazone specifically represses tumour metastatic potential in chromatin inaccessibility-mediated FABP4-deficient gastric cancer. Theranostics 12:1904
Chen X, Li R, Liang T, Zhang K, Gao Y, Xu L (2013) Puerarin improves metabolic function leading to hepatoprotective effects in chronic alcohol-induced liver injury in rats. Phytomedicine 20:849–852
Chigurupati H, Auddy B, Biyani M, Stohs SJ (2016) Hepatoprotective effects of a proprietary glycyrrhizin product during alcohol consumption: a randomized, double-blind, placebo-controlled, crossover study. Phytother Res 30:1943–1953
Clichici S, Olteanu D, Nagy A-L, Oros A, Filip A, Mircea PA (2015) Silymarin inhibits the progression of fibrosis in the early stages of liver injury in CCl4-treated rats. J Med Food 18:290–298
Cunningham AB, Shanley P, Laird S (2008) Health, habitats and medicinal plant use. Human health and forests: a global overview of issues, practice and policy. pp 35–62
Das A (2011) Heat stress-induced hepatotoxicity and its prevention by resveratrol in rats. Toxicol Mech Methods 21:393–399
Devarbhavi H (2017) Acute liver failure induced by anti-infectious drugs: causes and management. Current Hepatology Reports 16:276–285
Devarbhavi H, Dierkhising R, Kremers WK, Sandeep M, Karanth D, Adarsh C (2010) Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol 105:2396–2404
Devi Daimary U, Girisa S, Parama D, Verma E, Kumar A, Kunnumakkara AB (2022) Embelin: a novel XIAP inhibitor for the prevention and treatment of chronic diseases. J Biochem Mol Toxicol 36:e22950
Dianzani M, Muzio G, Biocca M, Canuto R (1991) Lipid peroxidation in fatty liver induced by caffeine in rats. Int J Tissue React 13:79
Ding L, Li J, Song B, Xiao X, Huang W, Zhang B, Tang X, Qi M, Yang Q, Yang Q (2014) Andrographolide prevents high-fat diet–induced obesity in C57BL/6 mice by suppressing the sterol regulatory element-binding protein pathway. J Pharmacol Exp Ther 351:474–483
Dixit S, Achar M (1983) Bhumyamalaki (Phyllanthus niruri Linn.) and jaundice in children. J Natl Integr Med Assoc 25:8501–133
Domitrović R, Jakovac H, Blagojević G (2011) Hepatoprotective activity of berberine is mediated by inhibition of TNF-α, COX-2, and iNOS expression in CCl(4)-intoxicated mice. Toxicology 280:33–43
Eldesoky AH, Abdel-Rahman RF, Ahmed OK, Soliman GA, Saeedan AS, Elzorba HY, Elansary AA, Hattori M (2018) Antioxidant and hepatoprotective potential of Plantago major growing in Egypt and its major phenylethanoid glycoside, acteoside. J Food Biochem 42:e12567
Eugenio-Pérez D, Montes De Oca-Solano HA, Pedraza-Chaverri J (2016) Role of food-derived antioxidant agents against acetaminophen-induced hepatotoxicity. Pharm Biol 54:2340–2352
Ezhilarasan D (2018) Oxidative stress is bane in chronic liver diseases: clinical and experimental perspective. Arab J Gastroenterol 19:56–64
Farombi EO, Shrotriya S, Na HK, Kim SH, Surh YJ (2008) Curcumin attenuates dimethylnitrosamine-induced liver injury in rats through Nrf2-mediated induction of heme oxygenase-1. Food Chem Toxicol 46:1279–1287
Federico A, Trappoliere M, Loguercio C (2006) Treatment of patients with non-alcoholic fatty liver disease: current views and perspectives. Dig Liver Dis 38:789–801
Feher J, Deák G, Müzes G, Lang I, Niederland V, Nekam K, Karteszi M (1989) Liver-protective action of silymarin therapy in chronic alcoholic liver diseases. Orv Hetil 130:2723–2727
Ferenci P, Dragosics B, Dittrich H, Frank H, Benda L, Lochs H, Meryn S, Base W, Schneider B (1989) Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J Hepatol 9:105–113
Flora K, Hahn M, Rosen H, Benner K (1998) Milk thistle (Silybum marianum) for the therapy of liver disease. Am J Gastroenterol 93:139–143
García-Niño WR, Pedraza-Chaverrí J (2014) Protective effect of curcumin against heavy metals-induced liver damage. Food Chem Toxicol 69:182–201
George A, Udani JK, Yusof A (2019) Effects of Phyllanthus amarus PHYLLPROTM leaves on hangover symptoms: a randomized, double-blind, placebo-controlled crossover study. Pharm Biol 57:145–153
Ghosh N, Ghosh R, Mandal V, Mandal SC (2011) Recent advances in herbal medicine for treatment of liver diseases. Pharm Biol 49:970–988
Giri BR, Baral R, Bhatt H, Khadka A, Tamrakar R, Timalsina G, Gyawali R (2023) Phytochemical screening, free-radical scavenging activity, in vitro alpha-amylase inhibitory activity, and in vivo hypoglycemic activity studies of several crude drug formulations based on selected medicinal plants of Nepal. Pharmaceut Chem J 56:1–10
Girish C, Pradhan SC (2012) Indian herbal medicines in the treatment of liver diseases: problems and promises. Fundam Clin Pharmacol 26:180–189
Gokkaya EO, Yesilot S, Ozgocmen M, Aslankoc R, Aydin Acar C (2022) Protective effects of resveratrol and avocado oil against paracetamol-induced hepatotoxicity in rats. Drug Chem Toxicol 45:2131–2139
Golabi P, Paik JM, Eberly K, De Avila L, Alqahtani SA, Younossi ZM (2022) Causes of death in patients with non-alcoholic fatty liver disease (NAFLD), alcoholic liver disease and chronic viral hepatitis B and C. Ann Hepatol 27:100556
Graebin CS (2018) The pharmacological activities of glycyrrhizinic acid (“glycyrrhizin”) and glycyrrhetinic acid. Sweeteners 2018:245-261
Gutiérrez-Rebolledo GA, Siordia-Reyes AG, Meckes-Fischer M, Jiménez-Arellanes A (2016) Hepatoprotective properties of oleanolic and ursolic acids in antitubercular drug-induced liver damage. Asian Pac J Trop Med 9:644–651
Guyton AC, Hall JE (2006) Medical physiology. Gökhan N, Çavuşoğlu H (Çeviren). 3.
Handa S (1986) Natural products and plants as liver protecting drugs. Fitoterapia. 57:307–351
Harish R, Shivanandappa T (2006) Antioxidant activity and hepatoprotective potential of Phyllanthus niruri. Food Chem 95:180–185
Hasan S, Khan R, Ali N, Khan A, Rehman M, Tahir M, Lateef A, Nafees S, Mehdi S, Rashid S (2015) 18-β Glycyrrhetinic acid alleviates 2-acetylaminofluorene-induced hepatotoxicity in Wistar rats: role in hyperproliferation, inflammation and oxidative stress. Hum Exp Toxicol 34:628–641
Henry L, Paik J, Younossi ZM (2022) The epidemiologic burden of non-alcoholic fatty liver disease across the world. Aliment Pharmacol Therapeut 56:942–956
Hikino H, Kiso Y (1988) Natural products for liver diseases. Economic and medicinal plant research/edited by H Wagner, Hiroshi Hikino, Norman R Farnsworth.
Ikeda K, Kawamura Y, Kobayashi M, Fukushima T, Sezaki H, Hosaka T, Akuta N, Saitoh S, Suzuki F, Suzuki Y (2014) Prevention of disease progression with anti-inflammatory therapy in patients with HCV-related cirrhosis: a Markov model. Oncology 86:295–302
Janbaz KH, Gilani AH (2000) Studies on preventive and curative effects of berberine on chemical-induced hepatotoxicity in rodents. Fitoterapia 71:25–33
Javed G, Javaid R, Ahmed F (2020) Kasni (Cichorium intybus): a Unani hepatoprotective drug. J Drug Deliv Therapeut 10:238–241
Jayaram S, Thyagarajan S, Sumathi S, Manjula S, Malathi S, Madanagopalan N (1997) Efficacy of Phyllanthus amarus treatment in acute viral hepatitis A, B and non A non B: an openclinical trial. Indian J Virol 13:59–64
Joshi R, Kamat JP, Mukherjee T (2007) Free radical scavenging reactions and antioxidant activity of embelin: biochemical and pulse radiolytic studies. Chem Biol Interact 167:125–134
Joy K, Kuttan R (1998) Inhibition by Phyllanthus amarus of hepatocarcinogenesis induced by N-nitrosodiethylamine. J Clin Biochem Nutr 24:133–139
Kashaw V, Nema AK, Agarwal A (2011) Hepatoprotective prospective of herbal drugs and their vesicular carriers-a review. Int J Res Pharmaceut Biomed Sci 2:360–374
Khoder NM, Sawie HG, Sharada HM, Hosny EN, Khadrawy YA, Abdulla MS (2022) Metformin and alpha lipoic acid ameliorate hypothyroidism and its complications in adult male rats. J Diab Metab Disord 21:1–11
Kim M, Yang S-G, Kim JM, Lee J-W, Kim YS, Lee JI (2012) Silymarin suppresses hepatic stellate cell activation in a dietary rat model of non-alcoholic steatohepatitis: αnalysis of isolated hepatic stellate cells. Int J Mol Med 30:473–479
Kimura M, Inoue H, Hirabayashi K, Natsume H, Ogihara M (2001) Glycyrrhizin and some analogues induce growth of primary cultured adult rat hepatocytes via epidermal growth factor receptors. Eur J Pharmacol 431:151–161
Kobayashi H (2022) Molecular targets for nonhormonal treatment based on a multistep process of adenomyosis development. Reprod Sci 30:1–18
Kosina P, Dokoupilová A, Janda K, Sládková K, Silberová P, Pivodová V, Ulrichová J (2017) Effect of Silybum marianum fruit constituents on the health status of rabbits in repeated 42-day fattening experiment. Anim Feed Sci Technol 223:128–140
Kuroda N, Inoue K, Ikeda T, Hara Y, Wake K, Sato T (2014) Apoptotic response through a high mobility box 1 protein-dependent mechanism in LPS/GalN-induced mouse liver failure and glycyrrhizin-mediated inhibition. PLoS ONE 9:e92884
Lavanchy D (2009) The global burden of hepatitis C. Liver Int 29:74–81
Lee CY, Peng WH, Cheng HY, Chen FN, Lai MT, Chiu TH (2006) Hepatoprotective effect of Phyllanthus in Taiwan on acute liver damage induced by carbon tetrachloride. Am J Chin Med 34:471–482
Lee JC, Tseng CK, Young KC, Sun HY, Wang SW, Chen WC, Lin CK, Wu YH (2014) Andrographolide exerts anti-hepatitis C virus activity by up-regulating haeme oxygenase-1 via the p38 MAPK/N rf2 pathway in human hepatoma cells. Br J Pharmacol 171:237–252
Lee SJ, Kang JH, Iqbal W, Kwon OS (2015) Proteomic analysis of mice fed methionine and choline deficient diet reveals marker proteins associated with steatohepatitis. PLoS ONE 10:1-17
Lee T-Y, Lee K-C, Chang H-H (2010) Modulation of the cannabinoid receptors by andrographolide attenuates hepatic apoptosis following bile duct ligation in rats with fibrosis. Apoptosis 15:904–914
Li G, Chen JB, Wang C, Xu Z, Nie H, Qin XY, Chen XM, Gong Q (2013) Curcumin protects against acetaminophen-induced apoptosis in hepatic injury. World J Gastroenterol 19:7440–7446
Li H, Sureda A, Devkota HP, Pittalà V, Barreca D, Silva AS, Tewari D, Xu S, Nabavi SM (2020) Curcumin, the golden spice in treating cardiovascular diseases. Biotechnol Adv 38:1
Li J, Pan Y, Kan M, Xiao X, Wang Y, Guan F, Zhang X, Chen L (2014) Hepatoprotective effects of berberine on liver fibrosis via activation of AMP-activated protein kinase. Life Sci 98:24–30
Li M, Liu L, Zhou Q, Huang L, Shi Y, Hou J, Lu H, Yu B, Chen W, Guo ZJaOHMTCCKDVI (2023) Phyllanthus niruri L. Applications of herbal medicine to control chronic kidney disease: volume II. Frontiers in Pharmaco 13:1-236
Li R, Liang T, He Q, Guo C, Xu L, Zhang K, Duan X (2013) Puerarin, isolated from Kudzu root (Willd.), attenuates hepatocellular cytotoxicity and regulates the GSK-3β/NF-κB pathway for exerting the hepatoprotection against chronic alcohol-induced liver injury in rats. Int Immunopharmacol 17:71–78
Liaw Y-F, Sung JJ, Chow WC, Farrell G, Lee C-Z, Yuen H, Tanwandee T, Tao Q-M, Shue K, Keene ON (2004) Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med 351:1521–1531
Lin CM, Lee JF, Chiang LL, Chen CF, Wang D, Su CL (2012) The protective effect of curcumin on ischemia-reperfusion-induced liver injury. Transplant Proc 44:974–977
Liu J, Xu Y, Yan M, Yu Y, Guo Y (2022) 18β-Glycyrrhetinic acid suppresses allergic airway inflammation through NF-κB and Nrf2/HO-1 signaling pathways in asthma mice. Sci Rep 12:3121
Lucena M, Andrade R, De La Cruz J, Rodriguez-Mendizabal M, Blanco E, De La Cuesta FS (2002) Effects of silymarin MZ-80 on oxidative stress in patients with alcoholic cirrhosis. Int J Clin Pharmacol Ther 40:2–8
Luo Q, Ding J, Zhu L, Chen F, Xu L (2018) Hepatoprotective effect of wedelolactone against concanavalin A-induced liver injury in mice. Am J Chin Med 46:819–833
Luper S (1998) A review of plants used in the treatment of liver disease: part 1. Altern Med Rev 3:410–421
Lv H, Qi Z, Wang S, Feng H, Deng X, Ci X (2017) Asiatic acid exhibits anti-inflammatory and antioxidant activities against lipopolysaccharide and d-galactosamine-induced fulminant hepatic failure. Front Immunol 8:785
Lv Y, Lei N, Wang D, An Z, Li G, Han F, Liu H, Liu L (2014) Protective effect of curcumin against cytomegalovirus infection in Balb/c mice. Environ Toxicol Pharmacol 37:1140–1147
Mabuchi A, Wake K, Marlini M, Watanabe H, Wheatley AM (2009) Protection by glycyrrhizin against warm ischemia-reperfusion–induced cellular injury and derangement of the microcirculatory blood flow in the rat liver. Microcirculation 16:364–376
Mahesh A, Jeyachandran R, Cindrella L, Thangadurai D, Veerapur V, Muralidhara Rao D (2010) Hepatocurative potential of sesquiterpene lactones of Taraxacum officinale on carbon tetrachloride induced liver toxicity in mice. Acta Biol Hung 61:175–190
Majee C, Mazumder R, Choudhary AN (2019) Medicinal plants with anti-ulcer and hepatoprotective activity: a review. Int J Pharm Sci Res 1:1–11
Malhotra B, Kulkarni GT, Dhiman N, Joshi D, Chander S, Kharkwal A, Sharma AK, Kharkwal H (2021) Recent advances on Berberis aristata emphasizing berberine alkaloid including phytochemistry, pharmacology and drug delivery system. J Herbal Med 27:100433
Manns MP, Wedemeyer H, Singer A, Khomutjanskaja N, Dienes HP, Roskams T, Goldin R, Hehnke U, Inoue H, Group ESS (2012) Glycyrrhizin in patients who failed previous interferon alpha-based therapies: biochemical and histological effects after 52 weeks. J Viral Hepatitis. 19:537–546
Marek R, Seckárová P, Hulová D, Marek J, Dostál J, Sklenár V (2003) Palmatine and berberine isolation artifacts. J Nat Prod 66:481–486
Marjani M, Baghaei P, Dizaji MK, Bayani PG, Fahimi F, Tabarsi P, Velayati AA (2016) Evaluation of hepatoprotective effect of silymarin among under treatment tuberculosis patients: a randomized clinical trial. Iranian J Pharmaceut Res 15:247
Martinou E, Pericleous M, Stefanova I, Kaur V, Angelidi AM (2022) Diagnostic modalities of non-alcoholic fatty liver disease: from biochemical biomarkers to multi-omics non-invasive approaches. Diagnostics 12:407
Masood M, Arshad M, Rahmatullh Q, Sabir S, Shoaib M, Amjad HQ, Tahir ZJP, Biology A (2021) 02. Picrorhiza kurroa: an ethnopharmacologically important plant species of Himalayan region. Pure Appl Biol 4:407–417
Mayer K, Myers R, Lee S (2005) Silymarin treatment of viral hepatitis: a systematic review. J Viral Hepatitis 12:559–567
Meena A, Pal B, Panda P, Sannd R, Rao M (2010) A review on Rubia cordifolia: its phyto constituents and therapeutic uses. Drug Invention Today 2:244–246
Mi X-J, Le H-M, Lee S, Park H-R, Kim Y-J (2022) Silymarin-functionalized selenium nanoparticles prevent LPS-induced inflammatory response in RAW264. 7 cells through downregulation of the PI3K/Akt/NF-κB pathway. ACS Omega 7:42723–42732
Misar S (2019) Hepatoprotective and hypolipidemic effect of Kutaki (Picrorhiza kurroa ROYLE ex Benth.)-A
Mohammed E, Peng Y, Wang Z, Qiang X, Zhao Q (2022) Synthesis, antiviral, and antibacterial activity of the glycyrrhizic acid and glycyrrhetinic acid derivatives. Russ J Bioorg Chem 48:906–918
Mohi-Ud-Din R, et al (2022) Novel drug delivery system for curcumin: Implementation to improve therapeutic efficacy against neurological disorders. Combinatorial Chemistry & High Throughput Screening 25(4):607-615
Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, Murray CJ, Naghavi M (2014) Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med 12:145
Moon AM, Yang JY, Barritt Iv AS, Bataller R, Peery AFA (2020) Rising mortality from alcohol-associated liver disease in the United States in the 21st century. Offic J Am Coll Gastroenterol 115:79–87
Moro T, Shimoyama Y, Kushida M, Hong YY, Nakao S, Higashiyama R, Sugioka Y, Inoue H, Okazaki I, Inagaki Y (2008) Glycyrrhizin and its metabolite inhibit Smad3-mediated type I collagen gene transcription and suppress experimental murine liver fibrosis. Life Sci 83:531–539
Mostafa-Hedeab G, Al-Kuraishy HM, Al-Gareeb AI, Jeandet P, Saad HM, Batiha GE-S (2022) A raising dawn of pentoxifylline in management of inflammatory disorders in Covid-19. Inflammopharmacology 30:799–809
Muriel P, Rivera-Espinoza Y (2008) Beneficial drugs for liver diseases. J Appl Toxicol 28:93–103
Müzes G, Deák G, Lang I, Nékám K, Niederland V, Fehér J (1990) Effect of silimarin (Legalon) therapy on the antioxidant defense mechanism and lipid peroxidation in alcoholic liver disease (double blind protocol). Orv Hetil 131:863
Nadeem M, Dandiya P, Pasha K, Imran M, Balani D (1997) Hepatoprotective activity of Solanum nigrum fruits. Fitoterapia (Milano) 68:245–251
Navarro VJ, Belle SH, D’amato M, Adfhal N, Brunt EM, Fried MW, Reddy KR, Wahed AS, Harrison S (2019) Silymarin in non-cirrhotics with non-alcoholic steatohepatitis: a randomized, double-blind, placebo controlled trial. PLoS ONE 14:e0221683
Navekar R, Rafraf M, Ghaffari A, Asghari-Jafarabadi M, Khoshbaten M (2017) Turmeric supplementation improves serum glucose indices and leptin levels in patients with nonalcoholic fatty liver diseases. J Am Coll Nutr 36:261–267
Negi CK, Babica P, Bajard L, Bienertova-Vasku J, Tarantino G (2022) Insights into the molecular targets and emerging pharmacotherapeutic interventions for nonalcoholic fatty liver disease. Metabolism 126:154925
Nguyen TP, Tran CL, Vuong CH, Do THT, Le TD, Mai DT, Phan NM (2017) Flavonoids with hepatoprotective activity from the leaves of Cleome viscosa L. Nat Prod Res 31:2587–2592
Nicoletti NF, Rodrigues-Junior V, Santos AA Jr, Leite CE, Dias AC, Batista EL Jr, Basso LA, Campos MM, Santos DS, Souto AA (2014) Protective effects of resveratrol on hepatotoxicity induced by isoniazid and rifampicin via SIRT1 modulation. J Nat Prod 77:2190–2195
Nouri-Vaskeh M, Malek Mahdavi A, Afshan H, Alizadeh L, Zarei M (2020) Effect of curcumin supplementation on disease severity in patients with liver cirrhosis: a randomized controlled trial. Phytother Res 34:1446–1454
Orazizadeh M, Fakhredini F, Mansouri E, Khorsandi L (2014) Effect of glycyrrhizic acid on titanium dioxide nanoparticles-induced hepatotoxicity in rats. Chem Biol Interact 220:214–221
Oriakhi K, Uadia PO, Shaheen F, Jahan H, Ibeji CU, Iqbal CM (2020) Isolation, characterization, and hepatoprotective properties of betulinic acid and ricinine from Tetracarpidium conophorum seeds (Euphorbiaceae). J Food Biochem 45:1-7
Othman MS, Safwat G, Aboulkhair M, Abdel Moneim AE (2014) The potential effect of berberine in mercury-induced hepatorenal toxicity in albino rats. Food Chem Toxicol 69:175–181
Panahi Y, Khalili N, Sahebi E, Namazi S, Simental-Mendia LE, Majeed M, Sahebkar A (2018) Effects of curcuminoids plus piperine on glycemic, hepatic and inflammatory biomarkers in patients with type 2 diabetes mellitus: a randomized double-blind placebo-controlled trial. Drug Res (Stuttg) 68:403–409
Panahi Y, Kianpour P, Mohtashami R, Jafari R, Simental-Mendía LE, Sahebkar A (2017) Efficacy and safety of phytosomal curcumin in non-alcoholic fatty liver disease: a randomized controlled trial. Drug research 67:244–251
Pang X, Qiao Q, Vonglorkham S, Feng Z, Pang L, Chen S, Wang D, Lao L, Lin X, Wei J (2020) Asiatic acid ameliorates acute hepatic injury by reducing endoplasmic reticulum stress and triggering hepatocyte autophagy. Biomed Pharmacother 129:110375
Parés A, Planas R, Torres M, Caballería J, Viver JM, Acero D, Panés J, Rigau J, Santos J, Rodés J (1998) Effects of silymarin in alcoholic patients with cirrhosis of the liver: results of a controlled, double-blind, randomized and multicenter trial. J Hepatol 28:615–621
Patel H, Patel J, Patel K, Seth A, Patel K (2010) Clinical study of hepatoprotective drug Phyllanthus amarus. Res J Pharm Biol Chem Sci 1:335–340
Patil VS, Harish DR, Vetrivel U, Deshpande SH, Khanal P, Hegde HV, Roy S, Jalalpure SS (2022) Pharmacoinformatics analysis reveals flavonoids and diterpenoids from Andrographis paniculata and Thespesia populnea to target hepatocellular carcinoma induced by hepatitis B virus. Appl Sci 12:10691
Payton F, Sandusky P, Alworth WL (2007) NMR study of the solution structure of curcumin. J Nat Prod 70:143–146
Polyak SJ, Morishima C, Lohmann V, Pal S, Lee DY, Liu Y, Graf TN, Oberlies NH (2010) Identification of hepatoprotective flavonolignans from silymarin. Proc Natl Acad Sci 107:5995–5999
Program NT (2011) Toxicology and carcinogenesis studies of milk thistle extract (CAS no. 84604–20–6) in F344/N rats and B6C3F1 mice (feed studies). National Toxicology Program technical report series. 1–177.
Prokunina-Olsson L, Muchmore B, Tang W, Pfeiffer RM, Park H, Dickensheets H, Hergott D, Porter-Gill P, Mumy A, Kohaar I (2013) A variant upstream of IFNL3 (IL28B) creating a new interferon gene IFNL4 is associated with impaired clearance of hepatitis C virus. Nat Genet 45:164–171
Puri A, Saxena R, Saxena R, Saxena K, Srivastava V, Tandon J (1993) Immunostimulant agents from Andrographis paniculata. J Nat Prod 56:995–999
Qin G, Xu R (1998) Recent advances on bioactive natural products from Chinese medicinal plants. Medicinal research reviews 18(6):375-382
Rahman MM, Bibi S, Rahaman MS, Rahman F, Islam F, Khan MS, Hasan MM, Parvez A, Hossain MA, Maeesa SKJB, Pharmacotherapy, (2022) Natural therapeutics and nutraceuticals for lung diseases: traditional significance, phytochemistry, and pharmacology. Biomed Pharmacother 150:113041
Rahmani S, Asgary S, Askari G, Keshvari M, Hatamipour M, Feizi A, Sahebkar A (2016) Treatment of non-alcoholic fatty liver disease with curcumin: a randomized placebo-controlled trial. Phytother Res 30:1540–1548
Rao GMM, Rao CV, Pushpangadan P, Shirwaikar A (2006) Hepatoprotective effects of rubiadin, a major constituent of Rubia cordifolia Linn. J Ethnopharmacol 103:484–490
Rastogi R, Saksena S, Garg N, Dhawan B (1995) Effect of picroliv on antioxidant-system in liver of rats, after partial hepatectomy. Phytother Res 9:364–367
Raut A, Dhami-Shah H, Phadke A, Shindikar A, Udipi S, Joshi J, Vaidya R, Vaidya AD (2022) Picrorhiza kurroa, Royle ex Benth: traditional uses, phytopharmacology, and translational potential in therapy of fatty liver disease. J Ayurveda Integr Med 100558:1-9
Ray A, Chaudhuri SR, Majumdar B, Bandyopadhyay SK (2002) Antioxidant activity of ethanol extract of rhizome ofPicrorhiza kurroa on indomethacin induced gastric ulcer during healing. Indian J Clin Biochem 17:44–51
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J (2009) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The lancet 373:2223–2233
Rodriguez LG, Ruigómez A, Jick H (1997) A review of epidemiologic research on drug-induced acute liver injury using the general practice research data base in the United Kingdom. Pharmacother J Human Pharmacol Drug Ther. 17:721–728
Sahin K, Orhan C, Akdemir F, Tuzcu M, Iben C, Sahin N (2012) Resveratrol protects quail hepatocytes against heat stress: modulation of the Nrf2 transcription factor and heat shock proteins. J Anim Physiol Anim Nutr 96:66–74
Salmi H, Sarna S (1982) Effect of silymarin on chemical, functional, and morphological alterations of the liver: a double-blind controlled study. Scand J Gastroenterol 17:517–521
Sheng M, Zhou Y, Yu W, Weng Y, Xu R, Du H (2015) Protective effect of berberine pretreatment in hepatic ischemia/reperfusion injury of rat. Transplant Proc 47:275–282
Shi Q, Wang Q, Chen J, Xia F, Qiu C, Li M, Zhao M, Zhang Q, Luo P, Lu T (2022) Transcriptome and lipid metabolomics-based discovery: glycyrrhizic acid alleviates Tripterygium glycoside tablet-induced acute liver injury by regulating the activities of CYP and the metabolism of phosphoglycerides. Front Pharmacol 12:4092
Šimják P, Petr T, Kaslová B, Fejfar T, Hůlek P, Pařízek A, Vítek L (2022) Ursodeoxycholic acid use in lactating female patients is associated with clinically negligible concentrations of this bile acid in breast milk. Sci Rep 12:19543
Singh D, Arya P, Sharma A, Dobhal M, Gupta R (2015) Modulatory potential of α-amyrin against hepatic oxidative stress through antioxidant status in Wistar albino rats. J Ethnopharmacol 161:186–193
Singh D, Singh R, Singh P, Gupta RS (2009) Effects of embelin on lipid peroxidation and free radical scavenging activity against liver damage in rats. Basic Clin Pharmacol Toxicol 105:243–248
Singh H, Mishra A, Mishra AK (2018) The chemistry and pharmacology of Cleome genus: a review. Biomed Pharmacother 101:37–48
Singh V, Visen PK, Patnaik GK, Kapoor NK, Dhawan BN (1992) Effect of picroliv on low density lipoprotein receptor binding of rat hepatocytes in hepatic damage induced by paracetamol. Indian J Biochem Biophys 29:428–432
Srivastava S, Srivastava A, Patnaik G, Dhawan B (1996) Effect of picroliv on liver regeneration in rats. Fitoterapia (Milano) 67:252–256
Stanaway JD, Flaxman AD, Naghavi M, Fitzmaurice C, Vos T, Abubakar I, Abu-Raddad LJ, Assadi R, Bhala N, Cowie B (2016) The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet 388:1081–1088
Stickel F, Schuppan D (2007) Herbal medicine in the treatment of liver diseases. Dig Liver Dis 39:293–304
Suk KT, Kim DJ, Kim CH, Park SH, Yoon JH, Kim YS, Baik GH, Kim JB, Kweon YO, Kim BI (2012) A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol 107:1380–1387
Sultana T, Rashid MA, Ali MA, Mahmood SF (2010) Hepatoprotective and antibacterial activity of ursolic acid extracted from Hedyotis corymbosa L. Bangladesh J Scientific Industr Res 45:27–34
Syamasundar KV, Singh B, Thakur RS, Husain A, Kiso Y, Hikino H (1985) Antihepatotoxic principles of Phyllanthus niruri herbs. J Ethnopharmacol 14:41–44
Szabó L, et al (2022) Tailoring the structure of chitosan-based porous carbon nanofiber architectures toward efficient capacitive charge storage and capacitive deionization. ACS Applied Materials & Interfaces 14(3):4004-4021
T Krishnareddy N, Thomas JV, Nair SS, N Mulakal J, Maliakel BP, Krishnakumar I (2018) A novel curcumingalactomannoside complex delivery system improves hepatic function markers in chronic alcoholics: a double-blinded, randomized, placebo-controlled study. BioMed Res Int 2018:1-10
Tang R, Li R, Li H, Ma X-L, Du P, Yu X-Y, Ren L, Wang L-L, Zheng W-S (2021) Design of hepatic targeted drug delivery systems for natural products: insights into nomenclature revision of nonalcoholic fatty liver disease. ACS Nano 15:17016–17046
Thirupathi A, Silveira P, Nesi R, Pinho RJH, Toxicology E (2017) β-Amyrin, a pentacyclic triterpene, exhibits anti-fibrotic, anti-inflammatory, and anti-apoptotic effects on dimethyl nitrosamine–induced hepatic fibrosis in male rats. Human Exper Toxicol 36:113–122
Thyagarajan S, Jayaram S, Gopalakrishnan V, Hari R, Jeyakumar P, Sripathi M (2002) Herbal medicines for liver diseases in India. J Gastroenterol Hepatol 17:S370–S376
Tian D, Wang F, Duan M, Cao L, Zhang Y, Yao X, Tang J (2019) Coumarin analogues from the Citrus grandis (L.) osbeck and their hepatoprotective activity. J Agric Food Chem 67:1937–1947
Timmermans S, Vandewalle J, Libert C (2022) Dimerization of the glucocorticoid receptor and its importance in (patho) physiology: a primer. Cells 11:683
Trinchet JC, Coste T, Lévy VG, Vivet F, Duchatelle V, Legendre C, Gotheil C, Beaugrand M (1989) Treatment of alcoholic hepatitis with silymarin. A double-blind comparative study in 116 patients. Gastroenterol Clin Biol 13:120–124
Tu CT, Han B, Yao QY, Zhang YA, Liu HC, Zhang SC (2012) Curcumin attenuates concanavalin A-induced liver injury in mice by inhibition of toll-like receptor (TLR) 2, TLR4 and TLR9 expression. Int Immunopharmacol 12:151–157
Tu CT, Yao QY, Xu BL, Wang JY, Zhou CH, Zhang SC (2012) Protective effects of curcumin against hepatic fibrosis induced by carbon tetrachloride: modulation of high-mobility group box 1, toll-like receptor 4 and 2 expression. Food Chem Toxicol 50:3343–3351
Tujios SR, Lee WM (2018) Acute liver failure induced by idiosyncratic reaction to drugs: challenges in diagnosis and therapy. Liver Int 38:6–14
Tzeng JI, Chen MF, Chung HH, Cheng JT (2013) Silymarin decreases connective tissue growth factor to improve liver fibrosis in rats treated with carbon tetrachloride. Phytother Res 27:1023–1028
Velussi M, Cernigoi AM, Dapas F, Caffau C, Zilli M (1997) Long-term (23 months) treatment with an anti-oxidant drug (silymarin) is effective on hyperinsulinemia, exogenous insulin need and malondialdehyde levels in cirrhotic diabetic patients. J Hepatol 26:871–879
Venmathi Maran BA, Iqbal M, Gangadaran P, Ahn B-C, Rao PV, Shah MD (2022) Hepatoprotective potential of Malaysian medicinal plants: a review on phytochemicals, oxidative stress, and antioxidant mechanisms. Molecules 27:1533
Wadhwa K, Pahwa R, Kumar M, Kumar S, Sharma PC, Singh G, Verma R, Mittal V, Singh I, Kaushik D (2022) Mechanistic insights into the pharmacological significance of silymarin. Molecules 27:5327
Wang ME, Chen YC, Chen IS, Hsieh SC, Chen SS, Chiu CH (2012) Curcumin protects against thioacetamide-induced hepatic fibrosis by attenuating the inflammatory response and inducing apoptosis of damaged hepatocytes. J Nutr Biochem 23:1352–1366
Wang T, Zhao L-J, Li P, Jiang H, Lu G-C, Zhang W-D, Li H-L, Yuan B-J (2011) Hepatoprotective effects and mechanisms of dehydrocavidine in rats with carbon tetrachloride-induced hepatic fibrosis. J Ethnopharmacol 138:76–84
Wang Y, Jiang Y, Fan X, Tan H, Zeng H, Chen P, Huang M, Bi H (2015) Hepato-protective effect of resveratrol against acetaminophen-induced liver injury is associated with inhibition of CYP-mediated bioactivation and regulation of SIRT1-p53 signaling pathways. Toxicol Lett 236:82–89
Wang Y, Lou Z, Wu Q-B, Guo M-L (2010) A novel hepatoprotective saponin from Celosia cristata L. Fitoterapia 81:1246–1252
WHO (2017) Global hepatitis report. Global hepatitis report. pp 1–83
WHO (2017) Global tuberculosis report 2018. Global tuberculosis report 2017.
World Health Organization, et al (2004) Global status report on alcohol 2004. World Health Organization
Xiao HB, Sun ZL, Zhang HB, Zhang DS (2012) Berberine inhibits dyslipidemia in C57BL/6 mice with lipopolysaccharide induced inflammation. Pharmacol Rep 64:889–895
Xiaoling L, Liming Y, Xiaohong W (2014) Efficacy of magnesium isoglycyrrhizinate in treatment of hepatitis E with severe jaundice. J 临床肝胆病杂志 30:537–539
Xu G-B, Xiao Y-H, Zhang Q-Y, Zhou M, Liao S-G (2018) Hepatoprotective natural triterpenoids. Eur J Med Chem 145:691–716
Xue Q, Sun Z-L, Guo M-L, Wang Y, Zhang G, Wang X-K (2011) Two new compounds from Semen celosiae and their protective effects against CCl4-induced hepatotoxicity. Nat Prod Res 25:772–780
Yan H-M, Xia M-F, Wang Y, Chang X-X, Yao X-Z, Rao S-X, Zeng M-S, Tu Y-F, Feng R, Jia W-P (2015) Efficacy of berberine in patients with non-alcoholic fatty liver disease. PLoS ONE 10:e0134172
Yao L, Zhang J, Jin J, Li H, Li L, Han X, Raza HK, Li X, Mao Y (2022) An analysis of the efficacy and safety of compound glycyrrhizin injections in the treatment of drug-induced liver injury using a nationwide database. Int J Clin Pharm 44:731–740
Ye J-F, Zhu H, Zhou Z-F, Xiong R-B, Wang X-W, Su L-X, Luo B-D (2011) Protective mechanism of andrographolide against carbon tetrachloride-induced acute liver injury in mice. Biol Pharm Bull 34:1666–1670
Ye X-G, Su Q-M (2013) Effects of entecavir and lamivudine for hepatitis B decompensated cirrhosis: meta-analysis. World J Gastroenterol: WJG 19:6665
Yi J, Xia W, Wu J, Yuan L, Wu J, Tu D, Fang J, Tan Z (2014) Betulinic acid prevents alcohol-induced liver damage by improving the antioxidant system in mice. J Vet Sci 15:141–148
Zhang J, Xu L, Zhang L, Ying Z, Su W, Wang T (2014) Curcumin attenuates D-galactosamine/lipopolysaccharide-induced liver injury and mitochondrial dysfunction in mice. J Nutr 144:1211–1218
Zhang L, Li H-Z, Gong X, Luo F-L, Wang B, Hu N, Wang C-D, Zhang Z, Wan J-Y (2010) Protective effects of asiaticoside on acute liver injury induced by lipopolysaccharide/D-galactosamine in mice. Phytomedicine 17:811–819
Zhang MQ, Ren X, Zhao Q, Yue SJ, Fu XM, Li X, Chen KX, Guo YW, Shao CL, Wang CY (2020) Hepatoprotective effects of total phenylethanoid glycosides from Acanthus ilicifolius L. against carbon tetrachloride-induced hepatotoxicity. J Ethnopharmacol. 256:112795
Zhang P, Ma D, Wang Y, Zhang M, Qiang X, Liao M, Liu X, Wu H, Zhang Y (2014) Berberine protects liver from ethanol-induced oxidative stress and steatosis in mice. Food Chem Toxicol 74:225–232
Zhang W, Hong R, Tian T (2013) Silymarin’s protective effects and possible mechanisms on alcoholic fatty liver for rats. Biomol Therapeut 21:264
Zhang W, Lin H, Cheng W, Huang Z, Zhang W (2022) Protective effect and mechanism of plant-based monoterpenoids in non-alcoholic fatty liver diseases. J Agric Food Chem 70:4839–4859
Zhang X, Organization WH (2002). Traditional medicine strategy 2002 2005
Zhao H, Deng B, Li D, Jia L, Yang F (2022) Enzymatic-extractable polysaccharides from Cordyceps militaris alleviate carbon tetrachloride-induced liver injury via Nrf2/ROS/NF-κB signaling pathway. J Funct Foods 95:105152
Zhao H, Wang Y, Zhang T, Wang Q, Xie W (2020) Drug-induced liver injury from anti-tuberculosis treatment: a retrospective cohort study. Med Sci Monit Int Med J Exper Clin Res 26:e920350-920351
Zhou Y, Chen K, He L, Xia Y, Dai W, Wang F, Li J, Li S, Liu T, Zheng Y, Wang J, Lu W, Yin Q, Lu J, Teng H, Guo C (2015) The protective effect of resveratrol on concanavalin-A-induced acute hepatic injury in mice. Gastroenterol Res Pract 506390:24
Zhou Y, Yang L, Liao Z, He X, Zhou Y, Guo H (2013) Epidemiology of drug-induced liver injury in China: a systematic analysis of the Chinese literature including 21 789 patients. Eur J Gastroenterol Hepatol 25:825–829
Author information
Authors and Affiliations
Contributions
BP, RB, and SP wrote and arranged the paper. RB, SP, AK, and BP edited the text and arranged the paper. BP and SP provided supervision and direction. All authors critically read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pandey, B., Baral, R., Kaundinnyayana, A. et al. Promising hepatoprotective agents from the natural sources: a study of scientific evidence. Egypt Liver Journal 13, 14 (2023). https://doi.org/10.1186/s43066-023-00248-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00248-w