Abstract
Background
In many countries, surgical closure of ventricular septal defects remains the recommended approach of ventricular septal defect closure. The aim of this study is to compare the safety, efficacy, and clinical effects of surgical versus transcatheter closure of a ventricular septal defect.
Methods
We conducted a comparative randomized study on patients undergoing ventricular septal defect closure. Patients were allocated to undergo either surgical (group I) or catheter (group II) ventricular septal defect closure.
Results
Seventy-two patients were included. Operation success was achieved in 100% of the surgical group versus 33 of 36 patients of the percutaneous group (91.6%) (p value 0.076). There was no significant difference regarding the residual ventricular septal defect. The postoperative echo in group I revealed severe tricuspid regurgitation in one patient (2.7%), and one patient needed a permanent pacemaker. On the other hand, in group II, during the procedure, one patient had severe tricuspid regurge (2.7%). There was a significant difference in the postoperative data favoring group II over group I regarding ventilation duration, intensive care unit stay, total hospital stay, and blood transfusion (P value < 0.001 each).
Conclusion
Both transcatheter device closure and surgical repair are effective treatments. In contrast, the psychological profile of the transcatheter device was superior to the surgical repair, especially in terms of avoiding sternotomy scar, blood loss and transfusion, and hospital stay. On the other hand, transcatheter intervention is limited only to the anatomically suitable ventricular septal defects, in addition, surgical backup is a must in case of complicated transcatheter closure, which gives the upper hand to surgery to be the recommended approach for most of the ventricular septal defects.
Clinical registration number
NCT05306483 registered 04/05/2022 (retrospectively registered) at ClinicalTrials.gov PRS.
Graphical Abstract

Similar content being viewed by others
Background
Children with ventricular septal defect (VSD) account for 20% of all Congenital heart diseases (CHDs) [1]. The most prevalent hemodynamically significant subtype is a perimembranous ventricular septal defect (pmVSD) [2]. Before catheter-based closure was available, the gold standard therapy for VSD closure was surgery [3]. However, surgical closure has several consequences, including scars from the incision, infection, and postoperative pain [4].
In 1994, Rigby and Redington used the Rashkind double umbrella device to demonstrate transcatheter closure of the VSD [5]. Hijazi et al. were the first to employ the Amplatzer VSD occluder device to close the VSD in 2002 [6], which became extensively used in numerous centers around the world due to its minimally invasive design [7]. Device-related consequences include complete heart block (CHB), tricuspid and aortic regurgitation, and device embolization limiting its usage [8]. However, recent improvements in device design and operator skills have dramatically improved the results of employing the transcatheter method to treat VSDs [9]. The bundle of His and its branches are strongly connected to the infero-posterior border of VSD. Consequently, its closure has been linked to an increased risk of CHB. Even in individuals with atrioventricular septal malalignment, surgeons now know where the conduction tissue is located and can avoid damaging it [10]. The possible risk of catheter closure was therefore identified as the occurrence of an iatrogenic CHB. As a result, in many countries, surgical closure of VSDs remains the recommended approach of VSD closure [9]. The aim of this study is to compare the safety, efficacy, and clinical effects of surgical vs. transcatheter closure of VSDs.
Methods
Setting and ethical considerations
The present study was conducted at Ain Shams University Hospitals. The study protocol was approved and registered by the local ethics committee of Ain Shams Faculty of Medicine (FMASUMS 97/2021) and registered at clinicaltrials.gov (NCT05306483 registered on 04/05/2022). The study was conducted in accordance with the declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations. The legal guardians of each patient gave an informed consent before and after randomization and submission to the procedure.
Study design and patients
We conducted a comparative randomized, prospective study that recruited patients scheduled to undergo closure of VSDs at our institutions through the period from March 2021 to March 2022. The study included 72 VSD patients suitable for both surgical and transcatheter closures according to guidelines [11]. Peri-membranous defects > 4 mm away from the aortic valve and muscular defects were considered suitable for catheter closure. Only patients with New York Heart Association (NYHA) class I–III and a weight of at least 8 kg were included. We also included patients with left-to-right shunt and Qp/Qs > 1.5. We excluded patients with other congenital cardiac or valvular abnormalities who are indicated for surgical intervention of their valvular disease, infective endocarditis, atrioventricular block, atrial or supraventricular arrhythmia, history of stroke, systemic thromboembolism, rheumatic heart disease, and/or Cushing syndrome.
Sample size calculation
Considering the very close documented operative success and major complications rate of the two interventions, we used the hospital stay duration as an indicator for the calculation of the sample size. Considering the study of Zheng et al. [12] as a reference, the sample size was calculated as a study power of 80.0% and α probability error of 5.0%. Sample size calculation was achieved using G Power (Kiel University, Germany).
Preprocedural assessment
Patients were assessed preoperatively for sociodemographic characteristics, anthropometric measures, and consanguinity. All patients underwent transthoracic echocardiographic (TTE) examination, including two-dimensional and color-flow Doppler techniques.
Randomization and blinding
Before randomization, the study objectives, selection criteria and technique, and possible risks of the study interventions were plausibly explained to the legal guardians of included patients. Before the last preoperative visit, all patients were randomized to either of the study interventions using computer-generated random tables and the sealed envelope technique. All patients were considered as one group without randomization blocks classified according to clinical or echocardiographic data (simple randomization). Randomization process was supervised by an independent researcher who wasn’t aware of the study objectives. In the last preoperative visit, all patients and/or their legal guardians were informed about the type of intervention to which they were allocated. All of them agreed to the allocated intervention and provided written informed consent.
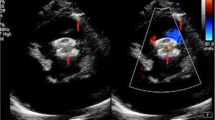
Transcatheter device implantation
VSD occluder is an expandable device. The closure was done under general anesthesia after the patients were fully heparinized (100 IU/kg). The TEE was performed intraoperatively to assess the defect during device positioning. A left ventriculogram in the left anterior oblique projection was acquired to profile the VSD. A Terumo wire was used to cross the VSD with a right Judkins catheter. The guidewire was snared from the pulmonary artery or vena cava to create an arteriovenous circuit. A long sheath (6–9 Fr) was advanced to the left ventricle. A left ventriculogram and TEE data were used to choose an occluder. The occluder was placed via the long sheath under fluoroscopic and echocardiographic guidance. Following the intervention, all patients were moved to post-Cath care unit. The ECG was continually monitored for the first 24 h. Patients who had no issues were regularly hospitalized for 24 h only. Patients with arrhythmias such as extended PR interval or atrioventricular block were hospitalized for follow-up till improvement. All patients received daily aspirin (5 mg/kg) following the procedure.
Surgical procedure
The surgical closure was performed under general anesthesia via hypothermic cardiopulmonary bypass and cardioplegic arrest. The chest was opened using the conventional median sternotomy technique. Surgical techniques were determined by the nature of each defect and include direct closure and patch closure with autologous pericardium; however, polyethylene terephthalate (Dacron; C.R. Bard, Haverhill, MA) and expanded polytetrafluoroethylene (Gore-Tex; W.L. Gore & Associates, Inc., Phoenix, AZ) may be used on occasion. Sutures were used to secure these patches in place. Direct closure (without a patch) may be used for minor faults. The majority of VSDs were corrected with right atriotomy to avoid the disadvantages of the Trans ventricular method.
Follow-up and study outcomes
The patients were followed up till they have been discharged from the hospital. The primary outcome of the present study was the rate of residual VSD shunts as detected by the 2D-TTE. The secondary endpoints include the need for blood transfusion, length of hospital and ICU stay, complications, and especially complete heart block.
Safety monitoring
There are no safety concerns as both procedures are well established. However, an interim analysis was carried out every 3 months after the initial follow-up period.
Statistical analysis
All statistical analyses were performed using SPSS version 22.0 for Windows. Continuous data were expressed as mean (± standard deviation [SD]), and categorical data were described as percentages. The association between type of closure and perioperative characteristics was tested using the Chi-square test or Independent t-test, with a p-value < 0.05 donating statistical significance.
Results
Seventy-two patients were included according to the calculated sample size There was no significant difference in the demographic data between group I and group II regarding age, weight, height, and BSA (P-value 0.1; Table 1).
Concerning the preoperative echocardiogram data, the group I showed overall, 29 (80.6%) of VSDs were perimembranous, and seven (19.4%) were muscular. The mean size of VSDs was 7.36 ± 2.80 mm. In group II, the preoperative ECHO showed that 23 (63.88%) of VSDs were perimembranous, and 13 (36.11%) were muscular. The mean size of VSDs was 5.39 ± 1.36 mm. There was no significant difference in the preoperative echocardiogram data between group I and group II regarding LVEDD, LVESD, IVS, LA, size of VSD (P-value 0.43), and RV (P-value = 0.33) (Table 1).
In group I, direct closure of VSD was done in one patient (2.7%). The pericardial patch was used in five patients (13.8%) while a Gortex patch was used in most of the patients (83.3%) (Fig. 1).
In group II, the mean disc diameter was 10.33 ± 2.53 mm. The total fluoroscopic time was 14.83 ± 11.67 min (Table 2).
Regarding intraoperative complications of the 2 groups, in the surgical group, there was one case of CHB that needed temporary PM, follow-up of the patient with continuous monitoring and frequent all lead off -PM ECG at the intermediate ICU till restoring sinus rhythm after 3 days, while in the transcatheter group, there were 3 cases of failure as discussed below (Table 3).
Procedure success
Surgical closure was attempted in 36 patients with a success rate of 100% as the operation was considered to be successful if there was no death and no large residual shunt. While in the percutaneous group, the success rate was 91.7% as there were 3 cases of failure of devices deployment (8.3%). Right anatomical assessment of the VSD is one of the most important factors that could predict the success of the transcatheter intervention. The cause of failure in the 1st patient was due to device instability mostly due to size-device mismatch. Although there were multiple trials of assessment of the anatomy and the size of the defect, the device instability occurred which should introduce the way to another additional imaging method of assessment that may eliminate this risk.
The operation was canceled and the patient has been referred to elective surgery. The second patient developed severe TR after implantation of the device due to mechanical distortion of the tricuspid valve, the device has been removed, and the patient was referred to elective surgery as he did not show any instability in the hemodynamics. The 3rd one failed due to rhythm changing into a complete heart block while introducing the sheath as the defect was too small (5 mm). The procedure was canceled, and the patient was referred to elective surgery.
Residual shunt
It was classified into 2 degrees: small if was less than 2 mm and large if more than 2 mm. In both groups, there were no significant residual shunts as in the surgical group (group I) small residual VSD was found in five patients of 36 successful patients (13.8%), while in group II, small residual VSD in 5 patients out of 33 successful patients (15.1%).
The postoperative echo in group I revealed mild tricuspid regurge in three patients (8.3%), moderate tricuspid regurge in one patient (2.7%), and severe tricuspid regurge in one patient (2.7%). On the other hand, the postoperative echo in group II revealed: mild tricuspid regurge in 4 patient (11.1%), moderate tricuspid regurge in one patient (2.7%), and severe tricuspid regurge in 1 patient (2.7%). No cases of both groups were detected with AR.
There was no significant difference in postoperative echo between both groups regarding tricuspid regurge P value 0.641 (Table 4).
Other complications were classified to major and minor. Major complications are late death due to a cause in direct relation to the procedure, thromboembolic events, repeating the operation, new onset severe valvular regurgitation that requires surgical intervention, device detachment, and the need for a permanent pacemaker. While minor complications are wound complications that required hospital admission or surgical debridement, reopening due to bleeding in the surgical group, groin hematoma in the transcatheter group, new arrhythmia, peripheral ischemia that not required endovascular intervention, increased one or two degrees of valvular regurge that not required intervention, self-limited hemolysis due to small residual, any effusion that required drainage as with chest tube or aspiration.
Major complications
In terms of major complications, there were no recorded cases of death during the period of follow-up; in the percutaneous group, there is one case of acute severe TR that was noticed during the advancement of the device as mentioned before. One patient in each group developed severe TR in the post-procedural ECHO, the two patients were known to have moderate TR before intervention. Accordingly, follow up with medical treatment as there was no clinical indication for surgical intervention at the time of follow-up.
Regarding the need for a permanent pacemaker, there were 2 cases of group II that developed complete heart block after being transferred to the ward, one of them restored normal sinus rhythm after 5 days, and a permanent pacemaker was inserted 2 weeks after transcatheter intervention in the 2nd patient. While in the surgical group, just one patient needed a permanent pacemaker after a complete heart block. No other major complications were recorded in both groups.
Minor complications
In group II, two patients (5.5%) had femoral hematoma after removing the femoral sheath, follow-up at the outpatient clinic occurred and no further intervention was needed.
ECG changes were recorded in 12 patients (33.3%) of the surgical group versus 10 patients (27.7%) of the transcatheter group. One patient in the transcatheter group had peripheral lower limb ischemia (2.7%) and presented with mild color changes in his right toe that resolved with medical treatment after 2 days with no intervention needed after follow-up. Two cases of the surgical group (5.55%) had significant bleeding that required surgical exploration. No significant difference between the two groups concerning minor complications.
Most of the patients in group I received blood products. In group II, All patients did not bleed nor receive blood products. There was a significant difference in the postoperative data favoring group II over group I regarding ventilation duration, ICU stays, total hospital stay, blood transfusion (P-value < 0.001 each), and ECG changes (P-value = 0.005) (Table 5).
Laboratory data
Serum levels of liver enzymes, BUN, and creatinine measured before the intervention, after 1 h of transcatheter intervention and 1 h after declamping the aorta in surgical closure and every 6 h for the next 72 h (P < 0.01) (Fig. 2).
Cardiac enzymes (CK-MB and troponin I) were normal in the two groups before the intervention; after the intervention, there was a significant difference between both groups (Fig. 3).
Discussion
The VSD is preferred to be managed surgically in children especially in patients with a low birth weight with a large-sized defect. However, surgical closure has major limitations, including a prolonged hospital stay and increased blood transfusions. In the last several years, transcatheter VSD closure has gained a lot of interest. The lower incidence of complications, a shorter hospital stay, almost no blood transfusion, less trauma, and rapid recovery are among the benefits of this intervention [13].
Our findings were in line with those of Yang et al. [14], who conducted a randomized controlled trial to evaluate the difference between surgical and transcatheter closure in children with VSD. Their findings showed that both groups are comparable in terms of major adverse events and mortality. On the other hand, no cases in the transcatheter group required blood transfusion compared to 23 cases in the surgical group (p < 0.001).
A meta-analysis of five studies [15,16,17,18,19] demonstrated that the success rate was very high in both groups (surgery and transcatheter), with no significant difference (98.4% vs. 98.1), respectively [11]. Catheter closure resulted in a significantly lower residual shunt (RR = 0.44, p = 0.01) than surgical closure. Comparisons between the catheter and surgical methods showed that transfusions and hospital stays were dramatically reduced in the catheter group (RR = 0.02, p < 0.00001) and (RR = 4.81, p = 0.001), respectively. However, the overall consequences, complete atrioventricular block, and the cost of both techniques were comparable [10].
For surgery, the most common complications were myocardial dysfunction, severe hemorrhage, subaortic stenosis, aneurysm formation, complete heart block, and severe pulmonary hypertension [20,21,22,23,24,25,26].
Surgeons have a good understanding of how to diagnose and treat patients with a single large VSD [27].
The transcatheter repair of VSDs was shown to be easier and to have fewer complications. But For the aneurysmal form of transcatheter VSD closure, many technical challenges were critical. In the first place, successfully crossing the VSD was the most difficult step in transcatheter closure for aneurysmal VSD [28]. Using alternative catheters (e.g., partially cut pigtail catheters, 3DRC, or right Judkins) and wires may be useful in certain situations. It was also critical that the occluder be placed within the aneurysmal sac at all times in order to minimize cardiac rhythm disturbances and consequences in the case of an aneurysmal form of VSD [14].
Operator skill, VSD morphology, and VSD size all have a role in the effectiveness of transcatheter VSD closure. In this study, the size of VSD was 5.39 ± 1.36 mm in the group treated with transcatheter and 7.36 ± 2.80 mm in the surgery group. Approximately, 80% of the VSDs in the surgical group were pmVSD, and it was 63.9% in the transcatheter group. Catheter closure of large pmVSDs is more challenging. In El-Kadeem et al.'s meta-analysis, the majority of trials revealed similar VSD sizes; however, two studies indicated considerably lower VSD sizes in the catheter group than in the surgical group. In our study, the mean age of patients treated with transcatheter closure was insignificantly higher than the surgical group. The transcatheter group of pediatric patients was substantially older than the surgical group in the trials of Xunmin et al., Oses et al., and Chen et al. [16, 17, 19]. Transcatheter closure has a high success rate because of these factors.
Conclusions
In conclusion, the current study suggests that both transcatheter device closure and surgical repair are effective treatments, with excellent short-term outcomes. Transcatheter closure is an alternative method to surgery for the anatomically suitable VSDs in children in this study.
Limitations
The small sample size of this study may hinder the generalizability of our findings. Another limitation is the lack of long-term follow-up outcomes. In addition, we did not evaluate the predictors of success in both groups.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AR :
-
Aortic regurgitation|
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- BSA:
-
Body surface area
- BUN:
-
Blood urea nitrogen
- CHB:
-
Complete heart block
- CHDs:
-
Congenital heart diseases
- CK-MB:
-
Creatinine kinase-MB
- ECG:
-
Electrocardiogram
- EF:
-
Ejection fraction
- ICU:
-
Intensive care unit
- IVS:
-
Inter-ventricular septum
- VSD :
-
Ventricular septal defect
- LA:
-
Left atrium
- LVEDD:
-
Left ventricular end-diastolic diameter
- LVESD:
-
Left ventricular end-systolic diameter
- MR:
-
Mitral regurgitation
- PASP:
-
Pulmonary artery systolic pressure
- PM:
-
Pacemaker
- pmVSD:
-
Perimembranous ventricular septal defect
- TEE:
-
Trans-esophageal echo
- TR:
-
Tricuspid regurgitation
References
Hoffman JIE, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol United States 39:1890–1900
Penny DJ, Vick GW 3rd (2011) Ventricular septal defect. Lancet (London, England). 377:1103–12 England
Sousa JE, Costa MA, Tuzcu EM, Yadav JS, Ellis S (2005) New frontiers in interventional cardiology. Circulation United States 111:671–681
Roos-Hesselink JW, Meijboom FJ, Spitaels SEC, Van Domburg R, Van Rijen EHM, Utens EMWJ et al (2004) Outcome of patients after surgical closure of ventricular septal defect at young age: longitudinal follow-up of 22–34 years. Eur Heart J England 25:1057–1062
Rigby ML, Redington AN (1994) Primary transcatheter umbrella closure of perimembranous ventricular septal defect. Br Heart J 72:368–371
Hijazi ZM, Hakim F, Haweleh AA, Madani A, Tarawna W, Hiari A et al (2002) Catheter closure of perimembranous ventricular septal defects using the new Amplatzer membranous VSD occluder: initial clinical experience. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 56:508–15 (United States)
Bass JL, Kalra GS, Arora R, Masura J, Gavora P, Thanopoulos BD et al (2003) Initial human experience with the Amplatzer perimembranous ventricular septal occluder device. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 58:238–45 (United States)
Sullivan ID (2007) Transcatheter closure of perimembranous ventricular septal defect: is the risk of heart block too high a price? Heart. pp 284–6
Masura J, Gao W, Gavora P, Sun K, Zhou AQ, Jiang S et al (2005) Percutaneous closure of perimembranous ventricular septal defects with the eccentric Amplatzer device: multicenter follow-up study. Pediatr Cardiol United States 26:216–219
El-Kadeem S, El Nemr S, El Amrousy D, Zoair A (2019) Comparison of transcatheter versus surgical closure of perimembranous ventricular septal defect in pediatric patients: A systematic review and meta-analysis. J Saudi Hear Assoc. 31:188–97 (Elsevier)
Saxena, Anita, et al (2019) “Indian Guidelines for Indications and Timing of Intervention for Common Congenital Heart Diseases: Revised and Updated Consensus Statement of the Working Group on Management of Congenital Heart Diseases.” Annals of Pediatric Cardiology, vol. 12, no. 3, p. 254. Crossref, https://doi.org/10.4103/apc.apc_32_19
Zheng Q, Zhao Z, Zuo J, Yang J, Wang H, Yu S et al (2009) A comparative study: Early results and complications of percutaneous and surgical closure of ventricular septal defect. Cardiology 114(4):238–243. https://doi.org/10.1159/000232405. (Epub 2009 Aug 7 PMID: 19672061)
Yi K, You T, Ding Z-H, Hou X-D, Liu X-G, Wang X-K et al (2018) Comparison of transcatheter closure, mini-invasive closure, and open-heart surgical repair for treatment of perimembranous ventricular septal defects in children: A PRISMA-compliant network meta-analysis of randomized and observational studies. Medicine (Baltimore) 97:e12583
Yang J, Yang L, Yu S, Liu J, Zuo J, Chen W et al (2014) Transcatheter versus surgical closure of perimembranous ventricular septal defects in children: A randomized controlled trial. J Am Coll Cardiol 63:1159–1168
Shang XK, Zhong L, Lu R, Zhang GC, Liu M, Shen QS, et al (2016) Comparison of Outcomes of Transcatheter and Surgical Procedure in Perimembranous Ventricular Septal Defect Patients with Tricuspid Regurgitation. Ann Acad Med Singap 45(7):322–325.
Xunmin C, Shisen J, Jianbin G, Haidong W, Lijun W (2007) Comparison of results and complications of surgical and Amplatzer device closure of perimembranous ventricular septal defects. Int J Cardiol Netherlands 120:28–31
Oses P, Hugues N, Dahdah N, Vobecky SJ, Miro J, Pellerin M et al (2010) Treatment of isolated ventricular septal defects in children: Amplatzer versus surgical closure. Ann Thorac Surg Netherlands 90:1593–1598
Yang J, Yang L, Yu S, Liu J, Zuo J, Chen W et al (2014) Transcatheter versus surgical closure of perimembranous ventricular septal defects in children: a randomized controlled trial. J Am Coll Cardiol United States 63:1159–1168
Chen ZY, Lin BR, Chen WH, Chen Q, Guo XF, Chen L-L et al (2014) Percutaneous device occlusion and minimally invasive surgical repair for perimembranous ventricular septal defect. Ann Thorac Surg Netherlands 97:1400–1406
Arora R, Trehan V, Kumar A, Kalra GS, Nigam M (2003) Transcatheter closure of congenital ventricular septal defects: experience with various devices. J Interv Cardiol United States 16:83–91
Janorkar S, Goh T, Wilkinson J (1999) Transcatheter closure of ventricular septal defects using the Rashkind device: initial experience. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 46:43–8 (United States)
Thanopoulos BD, Karanassios E, Tsaousis G, Papadopoulos GS, Stefanadis C (2003) Catheter closure of congenital/acquired muscular VSDs and perimembranous VSDs using the Amplatzer devices. J Interv Cardiol United States 16:399–407
Holzer R, Balzer D, Cao Q-L, Lock K, Hijazi ZM (2004) Device closure of muscular ventricular septal defects using the Amplatzer muscular ventricular septal defect occluder: immediate and mid-term results of a U.S. registry. J Am Coll Cardiol. 43:1257–63 (United States)
Marshalland AC, Lang P (2002) Closing ventricular septal defects in the cardiac catheterization laboratory. Heart Dis United States 4:51–53
Serraf A, Lacour-Gayet F, Bruniaux J, Ouaknine R, Losay J, Petit J et al (1992) Surgical management of isolated multiple ventricular septal defects. Logical approach in 130 cases. J Thorac Cardiovasc Surg. 103:437–42 (United States, discussion 443)
Backer CL, Idriss FS, Zales VR, Ilbawi MN, DeLeon SY, Muster AJ et al (1991) Surgical management of the conal (supracristal) ventricular septal defect. J Thorac Cardiovasc Surg United States 102:286–288
Daley M, Brizard CP, Konstantinov IE, Brink J, Kelly A, Jones B et al (2019) Outcomes of Patients Undergoing Surgical Management of Multiple Ventricular Septal Defects. Semin Thorac Cardiovasc Surg. 31:89–96 (United States; 2004;78:204–8)
Chen T-Y, Ju Y-T, Wei Y-J, Hsieh M-L, Wu J-M, Wang J-N (2021) Clinical Experience of Transcatheter Closure for Ventricular Septal Defects in Children Weighing under 15 kg. Acta Cardiol Sin. 37:618–24 (Taiwan Society of Cardiology)
Acknowledgements
Not applicable.
Funding
None (authors confirm they did not receive any funding to do this work).
All methods were performed according to the standard guidelines.
Author information
Authors and Affiliations
Contributions
HS (data curation; formal analysis; investigation; methodology; supervision; validation; writing – review and editing). MKE MBBCh (conceptualization; data curation; formal analysis; methodology; project administration; writing – original draft). AST (data curation; formal analysis; methodology; supervision; validation; writing – review and editing). YA (data curation; formal analysis; methodology; supervision; validation; writing – review and editing). AME (data curation; formal analysis; methodology; writing – review and editing). MAG (data curation; formal analysis; investigation; methodology; supervision; validation). The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study’s protocol was approved and registered by the local ethics committee of our institution Ain Shams University, faculty of medicine (FMASU M S 97/2021) and registered at ClinicalTrials.gov PRS (NCT05306483 registered 04/05/2022). The study was conducted in accordance with the declaration of Helsinki. The legal guardians of each patient gave an informed consent before submission to the procedure.
Consent for publication
All participants provided consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singab, H., Elshahat, M.K., Taha, A.S. et al. Transcatheter versus surgical closure of ventricular septal defect: a comparative study. Cardiothorac Surg 31, 8 (2023). https://doi.org/10.1186/s43057-023-00099-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-023-00099-6